Abstract
Objective
To pilot-test the feasibility and preliminary effect of a community health worker (CHW) intervention to reduce hospital readmissions.
Design
Patient-level randomized quality improvement intervention.
Setting
An academic medical center serving a predominantly low-income population in the Boston, Massachusetts area and 10 affiliated primary care practices.
Participants
Medical service patients with an in-network primary care physician who were discharged to home (n = 423) and had one of five risk factors for readmission within 30 days.
Intervention
Inpatient introductory visit and weekly post-discharge telephonic support for 4 weeks to assist patient in coordinating medical visits, obtaining and using medications, and in self-management.
Main Outcome Measures
Number of completed CHW contacts; CHW-reported barriers and facilitators to assisting patients; primary care, emergency department and inpatient care use.
Results
Roughly 70% of patients received at least one post-discharge CHW call; only 38% of patients received at least four calls as intended. Hospital readmission rates were lower among CHW patients (15.4%) compared with usual care (17.9%); the difference was not statistically significant.
Conclusion
Under performance-based payment systems, identifying cost-effective solutions for reducing hospital readmissions will be crucial to the economic survival of all hospitals, especially safety-net systems. This pilot study suggests that with appropriate supportive infrastructure, hospital-based CHWs may represent a feasible strategy for improving transitional care among vulnerable populations. An ongoing, randomized, controlled trial of a CHW intervention, developed according to the lessons of this pilot, will provide further insight into the utility of this approach to reducing readmissions.
Keywords: inpatient readmissions, community health worker, quality improvement, safety net
Introduction
Low-income adult patient populations in the United States including Medicaid beneficiaries and uninsured patients experience 30-day hospital readmission rates that are comparable to Medicare fee-for-service patients [1]. Nevertheless, research on transitional care is dominated by studies of elderly populations [2–4], individuals with specific diagnoses [5–8], selected groups such as veterans [9] or English-speaking patients only [10]. The most promising care transition interventions for the elderly have used multiple components, including enhanced discharge preparation, cross-site communication, medication reconciliation, outpatient follow-up and self-management skills [2, 7, 8, 11]. However, these interventions have featured a high level of post-discharge contact between licensed care professionals and patients to bridge the gap between inpatient discharge and outpatient follow-up care.
Safety-net hospitals, which predominantly serve low-income populations, may not be financially equipped to replicate approaches requiring costly professional staff [12]. Further, it is unclear to what extent these interventions generalize to low-income patient populations. Within low-income populations, difficult life circumstances and a lack of services that address medical needs, social support and transportation to clinical appointments and pharmacies are additional impediments to recuperation from hospitalization and receipt of post-discharge care [13, 14]. Difficulties in communication and appointment scheduling may also play a role in increasing the risk of hospital readmissions among safety-net patients, of whom 30–40% may speak a language other than English at home [15].
Community health workers (CHWs) may offer a cost-effective strategy to address these types of barriers to care [16]. They provide multiple services to support improved self-management and access to care, including health education, patient advocacy, interpreter services, navigation of community and medical services, and social support [17]. Frequently, members of the neighborhoods they serve, their community knowledge and linguistic and cultural compatibility with clients are thought to enhance their effectiveness [18, 19]. The unique skills and services that CHWs offer are well-aligned with the barriers to recuperation and post-discharge care that safety-net patients encounter. There is promising evidence that CHWs can improve health care utilization and outcomes [20, 21] and increasing interest in applying their unique skills to reducing hospital readmissions [22].
This pilot study evaluated the feasibility of a CHW intervention to reduce inpatient readmissions within 30 days of discharge for medical patients at high risk of readmission. Specifically, we sought to answer three questions: (i) did patients accept care transition services from a paraprofessional CHW? (ii) To what extent did the PN function per protocol? (iii) What were the preliminary effects of the intervention relative to usual care on the probability of outpatient follow-up, emergency department visit or inpatient readmission?
Methods
Setting
The study was conducted within a 200-bed academic medical center safety-net hospital and 10 affiliated adult primary care practices that are part of Cambridge Health Alliance (CHA). CHA is an integrated health care system including 2 hospitals and 10 community health clinics serving 100 000 patients in the Boston, Massachusetts area. The patient population is low-income and ethnically diverse, comprising 54% white, 15% Hispanic, 13% black and 3% Asian individuals. About one-third speak a language other than English at home; Portuguese (19%) and Spanish (9%) constitute the largest subgroups.
Intervention development
Two primary sources informed the development of the intervention: research on care transition interventions and the clinical experience of the quality improvement (QI) team led by a physician with shared responsibilities as a hospitalist and outpatient primary care clinician. As noted earlier, key features of effective transition interventions have included discharge preparation, communication between outpatient and inpatient providers, outpatient follow-up and enhancing self-management skills [2, 7, 8, 11]. Members of this QI team had previously developed and evaluated a successful care transition intervention that addressed two of these activities, discharge preparation and cross-site communication [23]. While effective for many patients, the team observed that a subset of patients required more intensive intervention to facilitate outpatient follow-up, including services that addressed non-medical barriers to care.
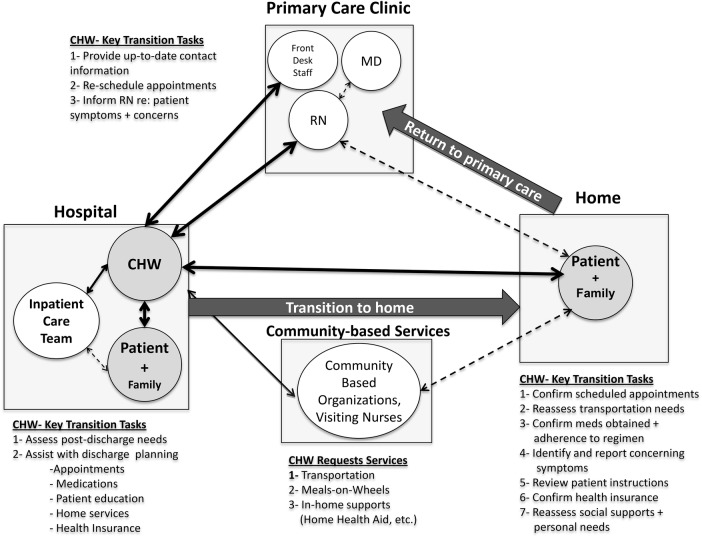
The QI team developed a 30-day intervention in which a hospital-based, bilingual CHW worked with the patient, caregivers and the inpatient and outpatient care teams to facilitate the transitions from hospital to home and back to the primary care provider (PCP). Fig. 1 illustrates the conceptualized role of the CHW within the discharge and post-discharge care process. We anticipated that the CHW would improve post-discharge outcomes through enhanced communication—to identify, trouble-shoot and respond to patient concerns—that supported recovery in the post-discharge period. As such, this intervention required CHWs to assess and respond to a broad array of potential needs across multiple settings [19].
Figure 1.
Role of community health worker in post-discharge care process.
The CHW spoke English and Portuguese, the dominant language among the health system's non-English-speaking patients. Telephone interpreter services were readily available for other languages. The intervention approach included the following components: one or more introductory visits with patients in the hospital; CHW participation in the hospital discharge process; semi-structured CHW outreach calls to patients on at least a weekly basis to elicit patient concerns; and liaison calls, as needed, to primary care nurses to assist in scheduling or to respond to patient concerns. A telephone script for the outreach calls prompted the CHW to address topics such as reminders and transportation assistance for upcoming appointments, barriers to obtaining medications, concerns that might require nurse intervention and poor understanding of self-management instructions.
The CHW intervention was piloted as a randomized QI initiative. This approach allowed the health system to leverage limited resources to test the feasibility of the intervention before making a more substantial financial commitment to a CHW program. The randomized nature of the pilot strengthened the evaluation of the preliminary effects of the intervention on health care use.
Randomized QI intervention
Participant selection
The QI team focused its limited intervention resources, a half-time CHW, on patients with one or more established risk factors for readmission: admission diagnosis of CHF, COPD or pneumonia [7, 24, 25]; length of stay >3 days [26]; weekend discharge [27]; age >60 [26] or hospitalization within the previous 6 months. These high-risk patients were eligible for the trial if they were discharged to home and had a CHA PCP.
Procedure
Patients were identified using data available in CHA's electronic medical record (EMR). During the 6-month pilot, patients were enrolled only for their first hospital admission that met eligibility criteria. One patient per day was randomly assigned to receive CHW services plus usual care (UC); remaining eligible patients were assigned to the control group. The control group received only UC for medical patients discharged to home, including a comprehensive, individualized home care plan reviewed by the medical service floor nurse with the patient, electronic transmission of the plan to the patient's primary care nursing staff and a telephone call from a primary care nurse to the discharged patient within 72 h of discharge to address medical questions or needs.
Patients were randomized when they became eligible for the intervention. This determination was made at admission for admitting diagnosis, age and hospitalization in the past 6 months. Patients who became eligible because of hospital stay >3 days were randomized on the fourth day of their stay. Patients discharged on the weekend were randomized on the following Monday. Due to practical constraints, discharge destination was unknown at randomization, although the intervention focused exclusively on patients discharged to home. Thus, we excluded from our analytic sample patients who died in the hospital or who were discharged to a destination other than home. The pilot CHW intervention began on 23 July 2010 and concluded on 13 December 2010.
Data and measures
Data
Data on patient demographics, study eligibility criteria, readmission, emergency room and primary care visits were obtained from CHA EMR. The CHW maintained a daily activity log, completed using an online survey tool that summarized the day's work, including attempted and completed contacts. Using these data, we assessed patient acceptance of the intervention and whether the CHW completed planned activities. Members of the QI team conducted a debriefing interview with the CHW at the close of the pilot to assess her perceptions about successes and failures in completing the protocol, achieving program objectives and suggestions for improving the approach.
Outcomes
We defined patient acceptance of the intervention as completion of at least one post-discharge telephone call with the CHW. Our primary measure of fidelity to the protocol was completion of at least four weekly telephone calls. We used binary variables to assess any PCP visit and any emergency department (ED) visit within 15 days and any hospital readmission within 15 and 30 days.
Analysis
Our analysis included descriptive statistics summarizing data from the CHW activity log, preliminary patient outcomes and a textual summary of the CHW interview. We conducted multivariable logistic regression to adjust for potential differences in the treatment and UC groups. These results were consistent with the unadjusted analyses, so we present only the unadjusted comparisons.
Results
Participant characteristics
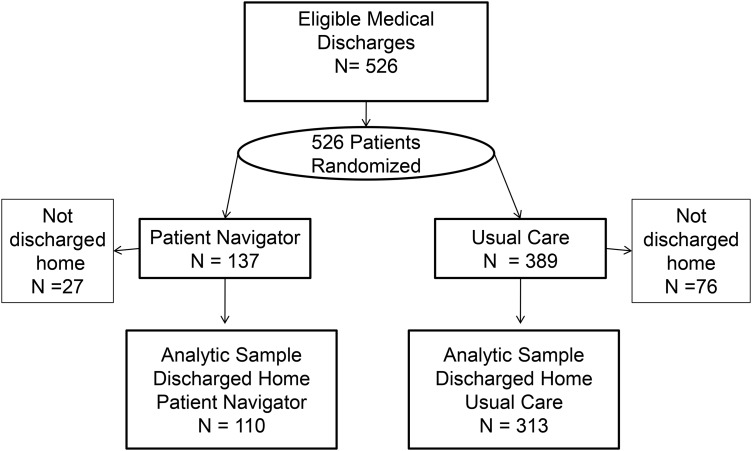
A total of 526 patients met study eligibility criteria and were randomized to the CHW or UC groups (Fig. 2). After exclusions for inpatient death or discharge to a destination other than home, the analytic sample included 110 CHW and 313 UC patients. There were no statistically significant differences in the socio-demographic characteristics of patients in the two study groups (Table 1). Men comprised slightly less than half of the sample and ∼40% of patients were non-native English speakers. The groups were balanced across most eligibility criteria. However, 51.8% of subjects in the CHW group were >60 years of age compared with 66.5% assigned to UC. Additionally, 40% of the CHW group was discharged on the weekend compared with 24% of the UC group, and three times as many patients whose only entry criterion was weekend discharge were assigned to the CHW (18.2%) compared with UC (6.4%) (results not shown).
Figure 2.
Study enrollment.
Table 1.
Descriptive characteristics of analytic sample by treatment assignment
| Patient navigator | Usual care | |
|---|---|---|
| N = 110 | N = 313 | |
| Male (%) | 46.3 | 49.2 |
| Race (%) | ||
| White | 60.9 | 63.6 |
| Black | 21.8 | 18.5 |
| Asian/other | 11.8 | 14.7 |
| Unknown | 5.5 | 3.2 |
| Non-native English speaker (%) | 40.9 | 37.7 |
| Discharged AMA (%) | 1.8 | 1.9 |
| High-risk study eligibility criteria (%) | ||
| Hospitalization in past 6 months | 30 | 29.7 |
| Age >60 | 51.8 | 66.5* |
| Pneumonia, CHF or COPD | 14.5 | 15.7 |
| LOS (mean) | 3.2 | 3.2 |
| Weekend discharge | 40 | 24.3* |
| Study-eligible based on a single criterion (%) | 54.5 | 50.2 |
AMA, against medical advice; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; LOS, level of service.
*P < 0.05.
Patient acceptance and protocol completion
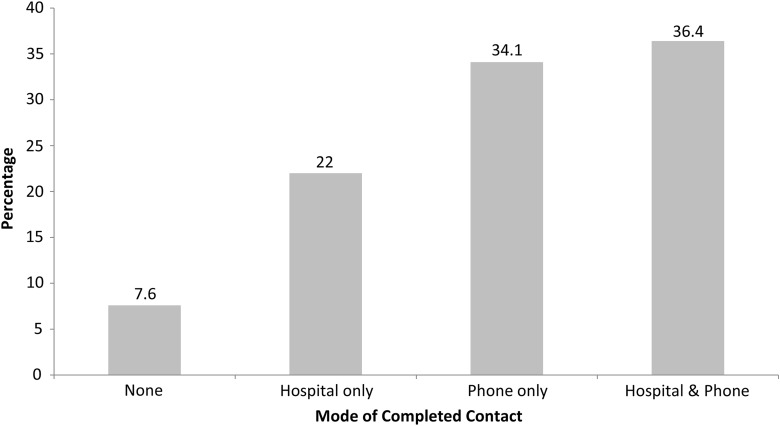
The CHW completed at least one telephone call with 70% of patients (Fig. 3). Approximately 7% of patients received no direct CHW contact in the hospital or by telephone, whereas 22% received direct CHW contact in the hospital only. The intended four-call protocol was completed for 38% of patients assigned to the CHW.
Figure 3.
Percentage of patients in CHW group with direct CHW contact.
Several themes emerged from the interview with the CHW that may explain the low protocol completion rate. The CHW suggested that patient contact during the inpatient stay and participation in the discharge meeting was important for developing a personal relationship with the patient. However, the CHW was frequently unaware of the timing of discharge meetings and often did not participate. As such, the CHW had no contact with 40% of patients while they were in the hospital, a factor that may have limited patients' responsiveness to follow-up call attempts.
The CHW had no dedicated electronic tools to manage the list of patients assigned to her. It was challenging for her to execute and track calls—particularly multiple call attempts relative to the patient's discharge date. Thus, limited logistical support tools for the CHW likely contributed to imperfect adherence to the call protocol. Similarly, information about outpatient appointments that were scheduled after discharge, missed outpatient appointments and readmissions was not quickly available to the CHW. Lacking this information, the CHW was not routinely poised to deliver calls when they may have been most welcome or effective.
Patient health care utilization
Assignment to the CHW did not appear to increase the rate of PCP visits within 15 days compared with UC (60.0 vs. 66.1%, respectively). (Table 2) The rate of ED visits was higher in the CHW group vs. UC (18.2 vs. 13.4%, respectively), although these rates varied dramatically by patient gender. ED use was lower among women seen by the CHW relative to UC (11.9 vs. 15.1%), whereas among men, ED use was significantly higher (25.5 vs. 11.7%, respectively, P < 0.05).
Table 2.
Primary care contact, emergency room use and hospital readmission for patients assigned to the community health worker and UC
| Full sample |
Women |
Men |
||||
|---|---|---|---|---|---|---|
| Patient navigator | Usual care | Patient navigator | Usual care | Patient navigator | Usual care | |
| % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | % (SE) | |
| PCP visit within 15 days | 60.0 (4.7) | 66.1(2.7) | 59.3 (6.5) | 64.2 (3.8) | 60.8 (6.9) | 68.2 (3.8) |
| ED visit within 30 days | 18.2 (3.7) | 13.4 (1.9) | 11.9 (4.2) | 15.1 (2.8) | 25.5 (6.1) | 11.7 (2.6)* |
| Readmission within 15 days | 14.5 (3.3) | 12.5 (1.9) | 16.9 (4.9) | 17.0 (3.0) | 11.8 (4.6) | 7.8 (2.2) |
| Readmission within 30 days | 15.4 (3.5) | 17.9 (2.2) | 16.9 (4.9) | 21.4 (3.3) | 13.7 (4.9) | 14.3 (2.8) |
| N | 110 | 313 | 59 | 159 | 51 | 154 |
SE, standard error; PCP, primary care provider; ED, emergency department.
*P < 0.05
In the full analytic sample, 15-day hospital readmission rates were higher among patients randomly assigned to the CHW (14.5%) compared with UC (12.5%). When stratified by gender, we observed no difference in 15-day readmission rates between women assigned to the CHW (16.9%) and to UC (16.9%), whereas 11.8% of men assigned to the CHW were readmitted compared with 7.8% of men assigned to UC. At 30 days post-discharge, hospital readmission rates were lower among patients assigned to the CHW (15.4%) than among UC patients (17.9%). The observed reduction was larger for female patients (16.9 vs. 21.4%) than for male patients (13.7 vs. 14.3%).
Discussion
This QI study demonstrated both the promise and challenges of a using a hospital-based CHW to reduce hospital readmissions in a safety-net health system. More than two-thirds of high-risk medical patients accepted at least one post-discharge telephone call from the CHW, indicating willingness to receive CHW services. However, the CHW completed the minimum protocol of four weekly calls for just 38% of patients. Nonetheless, the trend toward lower 30-day readmission rates among CHW patients (15.4%) relative to UC patients (17.9%) was encouraging, especially for women. Importantly, the lessons that emerged from the pilot study provide clear direction for redesigning the intervention to improve its effectiveness.
The low completion rate poses the most immediate challenge to the feasibility of such an intervention, but one that appears surmountable. The effectiveness of CHWs derives in part from the problem-solving, social support and service facilitation provided through routine contact with patients [18]. Absent these interactions, the potential CHW effect on readmissions is diminished. However, we were encouraged from our interview with the CHW that the most significant barriers to routine patient contact are modifiable. In general, these barriers are related to poor communication systems to plan participation in the discharge process while qualifying patients are in the hospital, and a lack of adequate logistical and informational support for the CHW. These limitations are particularly important to overcome as the patient caseload would increase for a CHW in a larger trial or in any ‘real-world’ hospital setting. To improve the feasibility of a CHW intervention, we have developed new system-level strategies that include a user-friendly relational database that is refreshed daily from hospital and outpatient data for the CHW. This database includes contact management tools, immediate notification of missed medical appointments, and facilitates coordination with nursing staff. Moreover, the database prompts the CHW to record the content and outcome of patient contacts to improve continuity. We also observed that once patient contact is made, the relatively broad responsibilities of the CHW to assess and respond to patient concerns indicated the need for additional training and support. These strategies have now been integrated into the approach used in an ongoing, randomized, controlled trial of a redesigned CHW intervention. The strategy includes: formalized training of CHWs in motivational interviewing, available community resources and contacts; closer supervision and mentoring of CHWs; and dedicated patient and contact management tools as described above for a team of CHWs [28].
We expected that the CHW would reduce readmission rates in part by reconnecting the patient to the PCP. However, we observed no improvement in the rate of PCP follow-up among CHW patients. It is premature to conclude that PCP follow-up is insensitive to a CHW intervention in light of the limited fidelity to the intervention in the pilot. However, because of the observed correlation between post-discharge outpatient follow-up and readmission risk [29, 30], future research is needed to understand why one-third of patients did not follow-up with their PCP within 15 days.
Notably, 75% of study patients readmitted within 30 days after discharge were readmitted within the first 15 days, during which time the CHW intervention was not associated with a reduction in readmissions. This finding may signal either CHW ineffectiveness or, conversely, CHW effectiveness at identifying and promptly facilitating needed post-discharge care (including readmissions). In the revised CHW intervention, a richer set of patient, CHW and provider data will permit exploration of the dynamics of post-discharge contact with the CHW, other providers, and the timing of readmissions. Additionally, the CHW will ensure that a follow-up PCP appointment is scheduled within 7 days after discharge. The system supports described earlier will further enable the CHW to monitor missed appointments and nurse follow-up calls in a more timely way.
Although the pilot study sample size does not support a formal test of outcome differences by gender, men appeared to be less responsive to the CHW intervention than women. It is unclear to what extent this is a function of different underlying clinical or social issues, gender discordance with the CHW, or random variation in a small sample. The revised intervention will evaluate CHW effectiveness by gender, controlling for differences in clinical complexity and social problems such as substance abuse or mental health disorders.
Limitations
CHA patients may have used health care outside of CHA. Because QI outcomes were measured using data that could be obtained from existing data systems, we did not capture out-of-network care. However, there is no reason to expect differential out-of-network care use across the two study arms. Moreover, the established patient–provider relationships and potentially higher out-of-pocket costs likely minimized out-of-network care.
The generalizability of the CHW intervention to other health care settings may be limited. However, CHA has many characteristics in common with other urban safety-net delivery systems nationally that account for a large share of Medicaid and charity care hospitalizations, including a diverse patient population and mission-driven approaches to managing complex patients [31]. Should further study demonstrate effectiveness and cost-effectiveness of the CHW intervention, integration of a CHW into post-discharge care will be a familiar concept to safety-net systems that have historically relied on these paraprofessionals [17]. Whether similar approaches might succeed in non-safety-net settings is unknown. However, reducing readmission rates is a growing priority, and all hospitals must determine how to use resources most cost-effectively to do so. Our model is unique in that it employs a bilingual hospital-based CHW, but many of the issues they address in ensuring care continuity after discharge are common in all settings.
Conclusion
Under payment systems based on performance [32], there is much at stake financially for under-resourced safety-net hospitals. Interventions that leverage low-cost resources commonly available within a safety-net health system will be vital. This QI project provides suggestive evidence that with sufficient logistical and training supports, hospital-based CHWs may have a role to play in reducing readmissions for vulnerable patient populations.
Funding
This work was supported by a Systems Improvement Grant Program Project from Partners Community Healthcare, Inc, and a faculty research grant from the Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, Inc.
References
- 1.Wier LM, Barrett M, Steiner C, et al. Rockville, MD: Healthcare Cost and Utilization Project; 2011. all-cause readmissions by payer and age, 2008: statistical brief #115. June 8. [Google Scholar]
- 2.Coleman EA, Parry C, Chalmers S. The care transitions intervention—results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 3.Nazareth I, Burton A, Shulman S, et al. A pharmacy discharge plan for hospitalized elderly patients—a randomized controlled trial. Age Ageing. 2001;30:33–40. doi: 10.1093/ageing/30.1.33. [DOI] [PubMed] [Google Scholar]
- 4.Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning for the hospitalized elderly—a randomized clinical-trial. Ann Intern Med. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure—a meta-analysis. JAMA. 2004;291:1358–67. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 6.Rich MW, Beckham V, Wittenberg C, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive-heart-failure. N Engl J Med. 1995;333:1190–5. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 7.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders—a randomized clinical trial. JAMA. 1999;281:613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 8.Naylor MD, Brooten DA, Campbell RL, et al. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 9.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 10.Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes a randomized trial. JAMA Intern Med. 2014;174:535–43. doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 11.Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–8. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 12.Berenson J, Shih A. Washington, DC: The Commonwealth Fund; 2012. Higher readmissions at safety-net hospitals and potential policy solutions. Contract No. 1651. [PubMed] [Google Scholar]
- 13.Kripalani S, Henderson LE, Jacobson TA, et al. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83:529–35. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- 14.Strunin L, Stone M, Jack B. Understanding rehospitalization risk: can hospital discharge be modified to reduce recurrent hospitalization? J Hosp Med. 2007;2:297–304. doi: 10.1002/jhm.206. [DOI] [PubMed] [Google Scholar]
- 15.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76:351–70. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Outcomes of community health worker interventions. Evidence Report/Technology Assessment No. 181. [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenthal EL, Brownstein JN, Rush CH, et al. Community health workers: part of the solution. Health Aff. 2010;29:1338–42. doi: 10.1377/hlthaff.2010.0081. [DOI] [PubMed] [Google Scholar]
- 18.Witmer A, Seifer SD, Finocchio L, et al. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85:1055–8. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riddick S. Improving access for limited English-speaking consumers: a review of strategies in health care settings. J Health Care Poor Underserv. 1998;9:S40–61. [Google Scholar]
- 20.Viswanathan M, Kraschnewski JL, Nishikawa B, et al. Outcomes and costs of community health worker interventions a systematic review. Med Care. 2010;48:792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- 21.Fisher EB, Strunk RC, Highstein GR, et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med. 2009;163:225–32. doi: 10.1001/archpediatrics.2008.577. [DOI] [PubMed] [Google Scholar]
- 22.Kangovi S, Long JA, Emanuel E. Community health workers combat readmission. Arch Intern Med. 2012;172:1756–7. doi: 10.1001/2013.jamainternmed.82. [DOI] [PubMed] [Google Scholar]
- 23.Balaban RB, Weissman JS, Samuel PA, et al. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23:1228–33. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross JS, Chen J, Lin Z, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010;3:97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friedman B, Jiang HJ, Elixhauser A. Costly hospital readmissions and complex chronic illness. Inquiry. 2008;45:408–21. doi: 10.5034/inquiryjrnl_45.04.408. [DOI] [PubMed] [Google Scholar]
- 26.Shalchi Z, Saso S, Li HK, et al. Factors influencing hospital readmission rates after acute medical treatment. Clin Med. 2009;9:426–30. doi: 10.7861/clinmedicine.9-5-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mackie AS, Lonescu-Ittu R, Pilote L, et al. Hospital readmissions in children with congenital heart disease: a population-based study. Am Heart J. 2008;155:577–84. doi: 10.1016/j.ahj.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Ross-Degnan D. 2011 Evaluating Sequential Strategies to Reduce Readmissions in a Diverse Population Agency for Healthcare Research and Quality. 1R01HS020628. [Google Scholar]
- 29.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–22. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 30.Sharma G, Kuo YF, Freeman JL, et al. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–70. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Washington, DC: American Association of Medical Colleges; 2010. How do teaching hospitals serve America's communities? 8-5-2010. Report No. [Google Scholar]
- 32.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152:114––7. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]