Abstract
Introduction:
Graphic warning labels have been shown to be more effective than text-only labels in increasing attention and perceived health risks, but most U.S. studies have involved single exposures in laboratory or Internet settings.
Methods:
We recruited a convenience sample (N = 202) of U.S. adult smokers from population subgroups with higher rates of smoking and smoking-related deaths who had participated in a larger survey about graphic warning labels. Participants were randomized to get 1 of 9 graphic + text labels or a text-only label. Research staff affixed a warning label sticker to participants’ cigarette pack(s) at enrollment. Color graphic labels covered slightly more than the lower half of packs. Black and white labels of current U.S. text-only warnings covered the existing side warning to prompt attention to the label (i.e., attention control). Participants received extra stickers of the same label for subsequent packs, and completed 3 telephone interviews in 1 week.
Results:
Participants reported low avoidance (<34%) and consistent use of the stickers (91%). Smokers consistently paid more attention to graphic than text-only labels. Only 5 of the 9 graphic warning labels were significantly associated with greater thoughts of health risks. Thinking about quitting and stopping smoking did not differ by label. Qualitative data illustrated differences in the “stickiness,” self-referencing, and counterarguments of graphic warning labels.
Conclusions:
U.S. smokers’ reactions to graphic warning labels on their own packs were similar to other, more controlled studies. Qualitative findings underscore the need for warning labels that encourage self-referential processing without increasing defensive reactions.
Introduction
In the United States, one of four text-only Surgeon General’s warning labels has been included on the side of all cigarette packs since 1984. Other countries have added larger graphic images to their warning labels.1 When required on packs and store displays, graphic warning labels provide high reach and frequency of exposure for communicating the health risks of smoking to the public.2 Graphic warnings may be especially influential given that tobacco companies increasingly rely on cigarette packaging and point-of-sale displays to communicate with consumers due to restrictions placed on other forms of advertising.3–5
Much of the research on individuals’ reactions to warning labels has been conducted in countries that have adopted graphic cigarette warning labels. Observational studies outside the United States suggest that graphic labels produced a significant reduction in national smoking rates and increased quit attempts.6–8 Although some debate the strength of this observational research,9–11 reviews of the literature suggest that compared with text-only warning labels, graphic labels are more likely to draw attention, and result in greater information processing, message recall, and perceived health risks of smoking.2,12,13 Greater message processing has been associated with greater intentions to quit and behavior change.14 Further, the positive effects of graphic warning labels are not offset by avoidance behaviors reported by a minority of people.2,15 Graphic labels also may be more effective among smokers, minorities, and those with low education,2,16–18 but may be less effective among dependent smokers and those with low intention to quit smoking.19
Previous research on graphic warning labels in the United States has generally involved brief experimental exposures to one or more graphic warnings in an Internet study or laboratory setting.17,20–23 Like two creative experiments that exposed non-U.S. smokers to a single graphic warning label over time (1–2 weeks),24,25 our efforts sought to more authentically expose U.S. smokers to graphic cigarette warning labels over time, and compare their cognitive reactions to graphic versus text-only warning labels. Further, because most studies have compared graphic versus text-only warning labels, this study focuses on differences across nine graphic warning labels selected by the Food and Drug Administration (FDA).
More research is needed to understand what features of graphic warning labels elicit positive and negative reactions, and increase persuasion. Graphic warning labels may impact recipients’ attitudes and behaviors indirectly through increased cognitive and affective reactions (i.e., “mediational pathways”).21,22 Greater attention, recall, engagement, emotional response, and self-referential thinking related to the warning may indicate more elaborative information processing.26–28 Self-referencing, relating a message to one’s personal (recalled) experiences, may include increased perceptions of personal involvement or relevance, as well as “activation of personal memories”.27 For example, some images may allow viewers to better imagine the harms from smoking happening to them. In one study, graphic, but impersonal images (e.g., a diseased mouth) were more personally relevant than images of an individual suffering from smoking harms (e.g., a man with a breathing mask).18 Also, images of babies may provide more motivation to quit smoking among women than men.17 Although self-referential thinking has been associated with greater recall and message persuasion, it may increase counterarguments when perceived message quality (e.g., argument strength) is low or message-processing demands exceed the value of the information provided.29 Counterarguments are defensive strategies that undermine motivation to change one’s risk behavior, and may be inherently (even if somewhat unconsciously) self-referential because they are meant to protect the self-concept from threats (e.g., smoking risk information). In previous research, smokers reported more negative emotions after viewing aversive (e.g., diseased mouth) versus not aversive (woman with empty baby buggy) images; however, they also reported more positive cognitions and positive implicit attitudes about smoking, and no differences in quit intentions.30 Such positive cognitions and implicit attitudes of smoking following aversive warnings may indicate defensive or reactant responding as a method for coping with negative affect.31,32 The present study sought to explore whether we could expose smokers to graphic warning labels over time and the extent to which smokers would attend to, and be persuaded by, those warnings. Additionally, we sought to explore cognitive and behavioral reactions to graphic warning labels among smokers, especially defensive responses such as counterarguing and reactance.33
Method
Sample, Study Design, and Procedures
Adult smokers who participated in a larger survey about graphic warning labels (June 2012 –March 2013) were eligible for the randomized experiment if they had a working phone and at least one half-full cigarette pack with them at enrollment. For the larger survey, we used targeted recruitment through community partners in 14 states to enroll a diverse, convenience sample of participants from five population sub-groups with high rates of smoking and/or smoking-related morbidity and mortality: low-income and rural Americans, Blacks, American Indians, U.S. military personnel, and blue-collar workers.34–38 Participants spent 30min completing the larger survey, which exposed them to all nine graphic warning labels on iPads as they responded to questions about each label individually (in random order) and completed card sort activities to categorize the nine labels in response to different questions. The iPad surveys presented images of the graphic labels alone and on unbranded cigarette packs. The nine graphic warning labels (Supplementary Appendix) used in this study were selected by the FDA to be used on all cigarette packs in the United States starting in September 2012. Legal challenges by the tobacco industry have since caused the FDA to propose the design of new labels that will comply with mandates in the Family Smoking Prevention and Tobacco Control Act and the First Amendment.
Of 504 adult smokers in the larger study, a convenience subset of 202 was enrolled in the randomized experiment. Participants agreed to be randomized to one of 10 conditions: one of nine FDA proposed graphic warning labels and a text-only condition in which participants were then randomized to one of the four text labels currently on U.S. cigarette packs. Research staff affixed warning label stickers to participants’ own cigarette pack(s) at enrollment. Extra stickers were provided to participants along with instructions to affix them to packs they used during the follow-up period. The number of extra stickers provided was based on the number of cigarettes they reported smoking per day at the time of enrollment. The same randomly assigned warning label was used by each participant throughout the whole week-long study.
Graphic warning stickers covered more than the lower half of the front of the pack, whereas text-only stickers covered the same area on the side of a pack as existing text warnings. Although the control condition’s warnings duplicated current warnings from the Surgeon General, we provided stickers in an attempt to reorient smokers to the warning labels and to ensure that all groups experienced the action of affixing warning labels to their own packs during the follow-up period (i.e., attention control). Trained interviewers administered computer-assisted telephone surveys to participants at approximately 2, 4, and 6 days follow-up. Participants were given gift cards of increasing amounts for completing each follow-up ($5, $10, $35). Each telephone survey took about 10min to complete. All study procedures and materials were approved by Washington University’s Institutional Review Board.
Measures
The same quantitative (fixed-choice) and qualitative (open-ended) questions were assessed at each follow-up (i.e., days 2, 4, and 6). Fixed-choice survey questions ensured standard and efficient data collection. Responses to open-ended questions were generally brief. Trained interviewers typed gist responses directly into the survey database. Two open-ended questions (“When you would see the warning label…what did you think?” and “…how did you feel”) assessed participants’ unique reactions to the warning labels they received. To better engage and learn from participants, we also asked them to elaborate on “yes” responses to many fixed-choice questions.
Exposure
Participants were asked to report how many full or partial cigarette packs they had smoked since the start of the study and on how many packs they had placed the warning label stickers. Participants who reported as many stickers used as number of packs used were considered compliant and all others were categorized as noncompliant. Avoidance of the warning label was assessed by measures from previous studies.39,40 Specifically, participants were asked to what extent (0 = none of the time to 4 = all of the time) did they ever: (a) try to cover up the label, (b) keep the label out of sight, (c) use a cigarette case or cover, or (d) decide not to use the warning label sticker or tear it off.
Attention
Participants were asked to what extent (0 = none of the time to 4 = all of the time) they looked at the warning label when opening their pack to get a cigarette. An open-ended question was used to classify whether they only briefly glanced at it or actually read/thought about it. We assessed subjective recall by asking participants if they remembered what the warning label on their package was about (yes/no), followed by an open-ended question that asked them to describe the label. Interviewers did not repeat the question or probe for further details once a participant offered a recollection of the label. Thus, we coded objective recall as correct if the participant correctly recalled any aspect of the image or text of their assigned warning label. Vague responses such as “surgeon general’s warning” and “smoking is harmful” were coded as incorrect. We also coded these responses across the three follow-up time points to determine whether participants were “ever accurate” and/or “always accurate” (yes/no). We were interested in both subjective and objective recall measures because they may reflect different levels of information processing.41,42 Further, smokers who perceive that they correctly recall the warning on their cigarette packs may be less inclined to think further about health risks or seek additional information or resources for quitting. Thus, acknowledging a general risk “Smoking kills” may prevent some individuals from deeper processing of the risk information (e.g., blunters).43
Reactions
Participants were asked if seeing the warning label on their cigarette pack ever: (a) made them think about the health risks of smoking, (b) made them think about quitting, (c) made them think twice about smoking, (d) stopped them from smoking, and (e) made them want to smoke more.39,40 Each question was answered yes/no; if yes, participants were asked to explain their answer (open-ended).
Potential covariates were assessed using standard measures in our larger survey: gender (male/female), age, race (Black, White, other), education (less than high school, high school/GED, some college, college degree or more), income (<$25,000 vs. ≥$25,000), and children living in the participant’s home (yes/no). We applied the rural-urban commuting areas (RUCA) taxonomy to recruitment locations and defined rurality as a RUCA code of 4 or above.44 The likelihood of using cessation resources to quit smoking was assessed as a mean score (α = .91) of 5 items measured on a 7-point scale (1 = not at all likely, 7 = extremely likely): How likely is it that…? (a) you will buy a nicotine replacement product to help you quit smoking, (b) you will take a prescription medication to help you quit smoking, (c) you will call 1-800-QUIT-NOW to help you quit smoking, (d) you will enroll in a quit smoking program if one were available to you at minimal cost and easy access, and (e) you will talk to a medical professional about how to quit smoking. Self-efficacy for quitting smoking was assessed as a mean score (α = .90) of 4 items measured on a 7-point scale (1 = strongly disagree to 7 = strongly agree): (a) if you tried to quit smoking, you would succeed; (b) I feel confident that I can quit smoking; (c) I feel confident that I can find help to quit smoking; and (d) I feel confident that I can overcome the barriers to quit smoking. Participants were also asked the number of packs smoked during the follow-up period.
Data Analysis
Logistic regression was used to examine associations between smoker’s responses and type of label. The generalized estimating equations method was used to account for the correlation of repeated measures on each participant over the three follow up surveys (days 2, 4, and 6).45 We specified an unstructured working correlation matrix for all models. Models included nine graphic warning label variables dummy coded with the text-only label as the referent. Two time variables were dummy coded with day 2 as the referent. Only significant covariates were retained in each model. We report adjusted odds ratios (AOR). Odds ratios are frequently used as estimates of effect size; OR = 1.5 is considered small, OR = 2.5 is medium, and OR = 4.3 is large.46,47
Qualitative data were used in two ways. First, we used qualitative data to quantify particular reactions or utterances to compare across study conditions (content analysis).48 Quantifying responses was appropriate for the two attention measures because the questions had a single focus, were answered by most participants, and involved categorical responses. For example, interviewers specifically asked (open-ended) each participant the extent to which they looked at the label, which resulted in two categories: briefly glanced at the warning label and actually read/thought about it. Similarly, two independent reviewers (AM, SB; κ = .93) compared open-ended recall responses to each participant’s assigned label and judged the responses for accuracy (yes/no); the first author’s ratings were used for analysis.
Second, we used qualitative data to illustrate conceptual themes grounded within participants’ reactions to the labels and identified via constant interaction with the data.49,50 In addition to the open-ended follow-up questions described above, participants were asked “how they felt”; and “what they thought” when they saw the warning label sticker. No probing questions were asked. Because response content varied widely, trained research staff coded these responses using traditional methods for analyzing qualitative data including using a codebook that was developed iteratively. Qualitative responses were recoded for all emergent codes (e.g., mismatch) just like a priori deductive codes (e.g., negative affect) (a copy of the final codebook can be obtained from the first author). The first author checked at least 5% of coded responses during each phase of coding to ensure reliable classification of responses (κ > .80); any discrepancies were discussed to reach consensus. As suggested by an anonymous reviewer, we reported frequencies for defensive reactions and included this variable as a covariate in analyses. Thus, for that variable, two authors (AM, SB) independently repeated the coding to ensure a comprehensive capture of quotes (κ > .95) and consensus in our estimates, rather than simply consensus in the representative themes that were evident in the data. Results were discussed among investigators, providing opportunities to challenge perceptions, explore potential negative and deviant cases, and reduce the potential for confirmatory bias.51,52 The conceptual analysis of the codes produced a few relevant themes (results), which we define below. Illustrative excerpts from interviewers’ notes are shown as participants’ responses in italic font. The themes reflect a combination of related codes (e.g., self-referential), as well as domains within a broadly-defined code (e.g., defensive reactions). We relied on published literature to help interpret the related findings in this study.26,27,29,33,53
Results
Sample
The sample was diverse in age, race, marital status, children living in the home, employment status, education, and income (Table 1). Most participants smoked more than one pack of cigarettes during the short follow-up period (M = 4.9, SD = 2.9). Because of small cell sizes, we did not examine statistical differences in socio-demographics by study condition. Over the 1-week study period, two participants (both assigned to graphic warning labels) were lost to follow-up.
Table 1.
Randomized Experiment Sample Characteristics
| Total sample (N = 202) | Graphic labels (N = 185) | Text-only labels (N = 17) | |
|---|---|---|---|
| Age (range 18–71) | M = 38.3 (SD = 13.5) | M = 38.6 (SD = 13.6) | M = 34.9 (SD = 12.2) |
| Male | 105 (52%) | 96 (52%) | 9 (53%) |
| Race | |||
| White | 89 (44%) | 82 (44%) | 7 (41%) |
| Black | 85 (42%) | 78 (42%) | 7 (41%) |
| Other | 28 (14%) | 25 (14%) | 3 (18%) |
| Marital status | |||
| Never been married | 83 (41%) | 72 (39%) | 11 (65%) |
| Married/coupled | 57 (28%) | 53 (29%) | 4 (24%) |
| Divorced/separated | 49 (24%) | 48 (26%) | 1 (6%) |
| Widowed | 7 (3%) | 7 (4%) | 0 |
| Children (<18) living at home | 82 (41%) | 75 (41%) | 7 (41%) |
| Employed | 82 (42%) | 77 (42%) | 5 (29%) |
| Education | |||
| Less than high school | 32 (16%) | 29 (16%) | 3 (18%) |
| High school/GED | 79 (39%) | 75 (41%) | 4 (24%) |
| Some college | 59 (29%) | 54 (29%) | 5 (29%) |
| ≥College degree | 30 (15%) | 25 (14%) | 5 (29%) |
| Income | |||
| <$10,000 | 62 (31%) | 57 (31%) | 5 (29%) |
| Over $10,000 but <$25,000 | 50 (25%) | 46 (25%) | 4 (24%) |
| Over $25,000 but <$50,000 | 51 (25%) | 47 (25%) | 4 (24%) |
| Over $50,000 | 22 (11%) | 20 (11%) | 2 (12%) |
| Rural | 14 (7%) | 12 (6%) | 2 (12%) |
| Likelihood of using resources to quit | M = 3.4 (SD = 1.9) | M = 3.4 (SD = 1.9) | M = 3.3 (SD = 2.1) |
| Self-efficacy to quit | M = 4.9 (SD = 1.7) | M = 4.9 (SD = 1.7) | M = 4.8 (SD = 2.0) |
| Packs smoked during study | |||
| 0–2 | 41 (20%) | 36 (19%) | 5 (29%) |
| >2–5 | 79 (39%) | 74 (40%) | 5 (29%) |
| >5–10 | 68 (34%) | 62 (34%) | 6 (35%) |
| >10–20 | 7 (3%) | 7 (4%) | 0 |
Note. GED = General Education Diploma. Totals may not equal 100 due to missing data.
Exposure
Participants reported high levels of compliance using the stickers on their packs and not tearing them off at the first follow-up (Table 2). Compliance did not change over time. Few participants reported avoidant behaviors such as using a case or cover to hide the warning label (Table 2). Logistic regression analysis results are shown in Table 3. Only one of nine comparisons was statistically significant: smokers given the label with the child in a smoke cloud (label 2) were less likely to cover up the label compared with smokers assigned to the text-only label (Table 3). More participants admitted to keeping the label out of sight (Table 2), but we found no significant correlates of this behavior (Table 3).
Table 2.
Participant Reactions to Warning Labels at Each Follow-Up
| Graphic labels | Text-only labels | |||||
|---|---|---|---|---|---|---|
| Day 2 (n = 185) | Day 4 (n = 184) | Day 6 (n = 183) | Day 2 (n = 17) | Day 4 (n = 17) | Day 6 (n = 17) | |
| Exposure to warning labels | ||||||
| Number of packs used since enrolled | M = 2.1 (SD = 1.3) | M = 3.6 (SD = 2.1) | M = 5.0 (SD = 3.0) | M = 2.0 (SD = 0.8) | M = 3.1 (SD = 1.9) | M = 4.7 (SD = 2.7) |
| 100% compliance putting stickers on packs | 169 (91%) | 155 (84%) | 129 (70%) | 15 (88%) | 15 (88%) | 14 (82%) |
| Ever did not use label or tore it off (%yes) | 4 (2%) | 5 (2.7%) | 3 (1.6%) | 1 (5.9%) | 1 (5.9%) | 1 (5.9%) |
| Tried to cover label up—none of the time | 151 (82%) | 156 (85%) | 158 (86%) | 15 (88%) | 15 (88%) | 15 (88%) |
| Kept label out of sight— none of the time | 123 (66%) | 134 (73%) | 136 (74%) | 12 (71%) | 13 (77%) | 12 (71%) |
| Used a case or cover to hide label (%yes) | 1 (1%) | 1 (1%) | 1 (1%) | 2 (12%) | 3 (18%) | 3 (18%) |
| Attention to warning labels | ||||||
| Looked at label when opened pack—most/all of the time | 121 (65%) | 117 (64%) | 121 (67%) | 2 (12%) | 8 (47%) | 8 (47%) |
| Self-report: recalled what label was about | 176 (95%) | 182 (99%) | 182 (99.5%) | 17 (100%) | 17 (100%) | 17 (100%) |
| Coded: any correct recall | 158 (85%) | 164 (89%) | 163 (89%) | 7 (41%) | 8 (47%) | 8 (47%) |
| Correct recall for message | 66 (36%) | 66 (36%) | 65 (36%) | 7 (41%) | 8 (47%) | 8 (47%) |
| Correct recall for graphic image | 130 (70%) | 125 (68%) | 132 (72%) | |||
| Correct recall for both image and message | 38 (21%) | 27 (15%) | 34 (19%) | |||
| Reactions to warning labels | ||||||
| Label made you think about health risks of smoking (%yes) | 146 (79%) | 151 (83%) | 158 (86%) | 10 (59%) | 11 (65%) | 10 (59%) |
| Label made you think about quitting (%yes) | 130 (71%) | 136 (75%) | 133 (73%) | 8 (47%) | 10 (59%) | 11 (65%) |
| Label made you think twice about smoking (%yes) | 132 (71%) | 131 (71%) | 128 (70%) | 12 (71%) | 12 (71%) | 11 (65%) |
| Label ever stopped you from smoking (%yes) | 57 (31%) | 65 (36%) | 70 (38%) | 6 (35%) | 6 (35%) | 8 (47%) |
| Label made you want to smoke more (%yes) | 3 (2%) | 2 (1%) | 5 (3%) | 0 (0%) | 1 (6%) | 1 (6%) |
Note. Totals (n) may not equal 100 due to missing data. Percentages are based on the column N.
Table 3.
Logistic Regression Analysis of Participant Exposure, Attention, and Reactions to Warning Labels
| Exposure | Attention | Reactions | |||||
|---|---|---|---|---|---|---|---|
| Warning labels | Tried to cover label up— none vs. some/most/all of the time | Kept label out of sight— none vs. some/most/all of the time | Looked at label when opened pack—most/all vs. none of the time | Any correct recall (coded variable)—yes vs. no | Label made you think about health risks of smoking—yes vs. no | Label made you think about quitting—yes vs. no | Label ever stopped you from smoking—yes vs. no |
| 1. Throat | 1.31 (0.31–5.64) | 1.43 (0.48–4.24) | 4.75 (1.44–15.66) | 5.12 (1.52–17.26) | 15.83 (3.14–79.93) | 2.67 (0.58–12.30) | 0.87 (0.21–3.58) |
| 2. Child in smoke cloud | 0.29 (0.08–0.99) | 0.58 (0.18–1.88) | 6.21 (1.85–20.92) | 13.09 (3.26–52.47) | 8.68 (1.76–42.72) | 3.14 (0.56–17.74) | 0.75 (0.21–2.7) |
| 3. Crying woman | 4.15 (0.81–21.23) | 1.33 (0.42–4.25) | 5.26 (1.66–16.65) | 4.07 (1.33–12.51) | 2.87 (0.71–11.60) | 0.81 (0.22–3.04) | 0.94 (0.25–3.53) |
| 4. Diseased mouth | 0.31 (0.09–1.1) | 0.68 (0.21–2.14) | 5.94 (1.68–21.08) | 8.13 (2.02–32.73) | 3.99 (1.12–14.21) | 1.16 (0.27–4.95) | 1.12 (0.30–4.22) |
| 5. Mask | 0.83 (0.22–3.17) | 1.00 (0.32–3.08) | 8.30 (2.66–25.89) | 6.05 (1.71–21.41) | 5.39 (1.2–24.19) | 2.88 (0.55–14.92) | 0.66 (0.17–2.58) |
| 6. Infant | 0.87 (0.21–3.57) | 1.02 (0.34–3.13) | 4.94 (1.65–14.76) | 31.33 (6.57–149.53) | 3.90 (1.14–13.4) | 2.49 (0.67–9.31) | 0.90 (0.19–4.25) |
| 7. Quit man | 1.82 (0.42–7.94) | 1.21 (0.37–3.99) | 4.27 (1.18–15.53) | 16.41 (2.91–92.66) | 2.67 (0.71–10.02) | 2.83 (0.37–21.32) | 0.86 (0.26–2.83) |
| 8. Diseased lung | 0.56 (0.17–1.85) | 0.48 (0.16–1.45) | 9.44 (2.24–39.71) | 8.57 (1.94–37.82) | 3.32 (0.93–11.85) | 1.63 (0.26–10.17) | 2.07 (0.41–10.44) |
| 9. Cadaver | 0.61 (0.16–2.36) | 1.19 (0.34–4.20) | 5.15 (1.53–17.37) | 21.19 (4.03–111.5) | 3.26 (0.90–11.74) | 0.36 (0.07–1.85) | 1.40 (0.36–5.49) |
| 10. Text-only | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Covariates | |||||||
| Day 4 | – | – | – | – | 1.26 (0.84–1.88) | – | 1.33 (0.82–2.15) |
| Day 6 | – | – | – | – | 1.74 (1.11–2.73) | – | 1.68 (1.09–2.60) |
| Day 2 | – | – | – | 1.00 | – | 1.00 | |
| Female | – | – | – | – | – | – | 2.47 (1.26–4.83) |
| Male | – | – | – | – | – | – | 1.00 |
| Black | – | 1.52 (0.92–2.49) | – | – | 4.10 (2.10–7.99) | – | – |
| Other | – | 1.00 (0.46–2.2) | – | – | 10.66 (2.54–44.68) | – | – |
| White | – | 1.00 | – | 1.00 | – | – | |
| Less than high school | – | – | 4.31 (1.49–12.42) | – | – | 3.03 (0.82–11.20) | – |
| High school grad | – | – | 4.22 (1.67–10.69) | – | – | 5.15 (1.68–15.78) | – |
| Some college | – | – | 2.58 (1.09–6.14) | – | – | 2.52 (0.92–6.92) | – |
| College degree | 1.00 | – | – | 1.00 | – | ||
| Use resources to quit | – | – | – | – | – | 1.56 (1.27–1.92) | 1.60 (1.35–1.90) |
| Self-efficacy to quit | – | – | 1.28 (1.06–1.55) | – | – | 1.43 (1.12–1.83) | – |
| Packs smoked | – | – | – | – | – | – | 0.79 (0.69–0.91) |
| Any defensive comments | – | – | 0.32 (0.15–0.66) | – | 0.27 (0.13–0.53) | 0.38 (0.16–0.88) | 0.33 (0.14–0.79) |
| No defensive comments | – | – | 1.00 | – | 1.00 | 1.00 | 1.00 |
Note. – = nonsignificant covariates were dropped from the model. Statistically significant associations are in bold font.
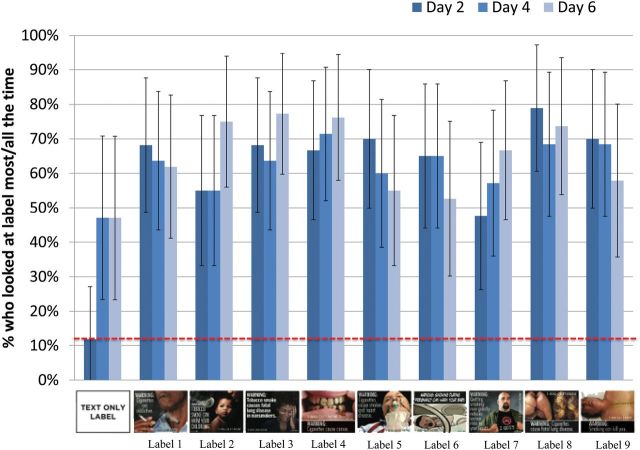
Attention
Compared to graphic warning labels, the text-only labels garnered little attention until after participants were asked about them during the first follow-up interview (Figure 1). Participants who received a graphic warning label reported looking at the label significantly more often than participants who received a text-only warning label, and this difference was consistent across all graphic labels (Table 3). Looking at the label was also associated with having lower education and greater self-efficacy to quit (Table 3).
Figure 1.
The extent of attention paid to graphic versus text-only cigarette warning labels every time a pack was opened. Note. The graph shows the percentage of smokers who looked at the label most or all of the time, with error bars showing the 95% confidence interval.
Subjective recall of the assigned label was over 95% at the first follow-up for both groups (Table 2). However, participants assigned to graphic labels more often correctly described some aspect of their label’s contents (image or message) compared with participants assigned to text-only labels (Table 2). Recall of graphic images was more often reported than message text for our general measure of recall (Table 2). Incorrect recall by text-only participants was due in part to vague responses like “surgeon general’s warning” or “smoking kills” and 35% of text-only participants never demonstrated correct recall over the three time points. Incorrect recall by graphic label participants was mainly due to descriptions of other (not assigned) graphic warning labels and 8% of participants never demonstrated correct recall. The odds of reporting any correct recall was greater for graphic versus text-only labels, and the pattern of associations was consistent for all graphic labels (Table 3).
Reactions
When we compared each graphic label separately in repeated measures analyses, the labels that showed a man smoking with a tracheotomy (label 1), the child in a smoke cloud (label 2), the diseased mouth (label 4), the oxygen mask (label 5) and the infant in an incubator (label 6) prompted significantly more thoughts about health risks than text-only labels (Table 3). There was also a significant effect of time: thinking about health risks was greater at the last versus first follow-up (Table 3). Compared with Whites, Blacks and other racial groups were more likely to report thinking about the health risks of smoking (Table 3). Ever making defensive comments about the labels was associated with decreased odds of thinking about the health risks of smoking (Table 3).
There was no association between warning labels and participants’ reported smoking-related cognitions and behavior regarding thinking about quitting, thinking twice about smoking, stopping smoking even temporarily, or smoking more (Table 2). Those who completed high school/GED had more thoughts of quitting compared to those with a college degree (Table 3). Those who reported greater likelihood of using cessation resources and self-efficacy for quitting had more thoughts of quitting, whereas reporting any defensive comments was related to fewer thoughts of quitting (Table 3). Reports that the labels ever made participants stop smoking were greater at the last follow-up versus the first (Table 3). Women (45%) were more likely than men (26%) to report that the labels ever made them stop smoking (Table 3). Those who reported higher likelihood for using resources to quit smoking were more likely to stop smoking. Those who smoked more packs of cigarettes during the study or made any defensive reactions were less likely to stop smoking in response to the warning label (Table 3).
Emergent Thematic Qualitative Results
Effect of Label Over Time
Some participants reported an increased or lingering effect of having a graphic warning label on their cigarette pack, perhaps due to its vividness: “I have become more bothered by the sticker. Now I think about it more. All of the time, even when I don’t look at it, even if I open a new pack with no label, I visualize the label on the pack, so I get a similar thought.” Others reported a waning effect over the short follow-up period, “At first I felt pretty wicked and now I have become kind of numb to it; it’s repetitive.” Additionally, many participants reported that the labels had no effect on them: “It doesn’t bother me at all” and “Just normal, I guess. I pretty much ignored it.”
Self-Referential Thinking
The label made some participants think about: (a) their own health problems related to smoking (e.g., dental, breathing, cough, asthma); “I worry about my health. Smoking isn’t good for a diabetic,” (b) how bad it would be if they experienced the negative health effect portrayed in the label; “Basically I would think about how I hoped that it (tracheotomy) wouldn’t happen to me,” and (c) someone in their own life who suffered from smoking, “My grandpa only smoked for a year or two and got lung cancer when he was 60 and died” or were at risk because of smoking “I thought about how second-hand smoke could harm my family and grandkids.” Other statements illustrated self-questioning responses to seeing the warning labels such as “why am I smoking?” and “Am I killing myself like this?”
All participants had been exposed to multiple graphic warning labels as part of the larger study and 29 participants (14%) in the randomized experiment perceived a mismatch in the label assigned to them, reporting that they thought another label would have suited them better. Although the labels that people thought would be effective for them varied by participant, some got more attention than others (e.g., man smoking with tracheotomy, baby in an incubator): “The sticker I got isn’t really a good one. The one with the guy with the hole in his neck is a good one. That one makes you think a bit. The same with the one with the cancer on the lip.” Several reported that they did not have children or were not going to get pregnant so the labels with children were “not relevant,” “not relatable,” and “least effective” for them. However, several others thought the labels with babies would have been more effective for them: “If I had the one with the little babies on it maybe I would feel differently, but this one—nothing.” One person would have hidden some images if assigned: “Of all the ones I saw, this one was least bothersome, worrisome. Ones I would have hid—the one with the stoma and the one with the premature baby in the incubator. Those would have needed to be hidden. More graphic.” Some participants’ responses illustrated low perceived similarity to, and appeal of, specific images: “I feel pretty disconnected from the image because I’ve known many smokers throughout my life that have never had a tracheotomy.”
Defensive Reactions
Defensive reactions, voiced by a minority of the sample (N = 35; 17%), illustrate a variety of strategies for reducing the perceived threat to the self (Table 4). Types of defenses evident in our data include message rejection, in which an individual denigrates the veracity of the message (text and/or image) or source (Table 4). Other defensive strategies allow individuals to acknowledge a harm in general, but (a) normalize it as a way of minimizing the importance of any specific risk, or (b) deny personal relevance by suggesting a reason an individual is not personally at risk (self-exemption) (Table 4). Psychological reactance is evident when individuals feel their personal choice or autonomy has been threatened and so respond negatively to the message. For example, several comments specifically mentioned personal liberties and choice (Table 4). Defensive comments (any vs. none) were not associated with demographics, packs smoked during follow-up, avoidance of label, or study condition (graphic vs. text-only, and within graphic).
Table 4.
Qualitative Responses Illustrating Defensive Information Processing (From a Total of 64 Comments From 35 Individuals)
| Suppression: self-exemption (19 comments from 14 individuals) |
| • I had a complete physical a year ago. I have the lungs of a 25-year old and I’ve been smoking for 47 years. It hurts you if you’re sitting, but I stay active. |
| • I’m one of the people where genetics is going good. My father smoked for 59 years, 5 packs a day. Gave it up when he was 79 because he didn’t like the taste. He lived until 89. |
| • Poor guy (in the label). Like most people that smoke it’ll be someone else not me. |
| Counterarguing: message rejection (17 comments from 12 individuals) |
| • I don’t feel it’s that true. I don’t think cigarette smoking is the major cause of someone’s teeth going bad. |
| • This is all information I already know but I do not agree with it all—especially information about secondhand smoke. |
| • I think it’s misinformed. The warning label is suggesting that if you don’t smoke you might not get bad teeth, but that’s not true. |
| • I think about carbon monoxide and the warning and think that that wasn’t fully true because then how could they sell cigarettes legally? |
| • Think it’s mis-informative. There are many reasons the mouth may look like that. |
| Counterarguing: normalize the harm (11 comments from 8 individuals) |
| • If there are labels like that on cigarettes there should be labels on other things like that…like fat kids on McDonald’s things or pictures of drunk driving on alcohol. |
| • I wondered why they didn’t put warning labels on cars if they are going to put them on cigarettes. |
| • The image was offensive—perhaps too forceful and graphic. Perhaps not fair to target smokers in this manner—why not a graphic image of an injury on beer bottles. |
| • Smoking is dangerous to your health, but death is inevitable. |
| • There are so many things that people can do to harm themselves. When I think about smoking I think that it may shave off 15 years of your life but is that a bad thing? I may lay in a bed dying for about 10 years and have never been a smoker like my grandma who lost her vision and her mental capacity and she never smoked. |
| Counterarguing: reactance (14 comments from 6 individuals) |
| • They were intrusive and an infringement upon liberties. |
| • I feel violated—my personal rights and liberties were trespassed. I believe the government is lying about the message behind smoking. |
| • I just thought it was kind of getting into people’s business; you shouldn’t take pictures and threaten them with it. |
| • The sticker reinforces my belief that this is demonizing smoking habits. I smoke because I choose to smoke and feel that smoking is targeted. |
| • I think it’s kind of extreme to put these on packages. It’s everyone’s right, constitutional right, to smoke if they want to. It hasn’t been proven that cigarettes cause all the health effects that the labels are saying; it could be from other things like air pollution. These measures are a little bit drastic. |
Discussion
Our unique study design allowed for the investigation of adult U.S. smokers’ reactions to graphic cigarette warning labels on their own packs while living with them for a week. This method of exposure is unique for U.S. audiences, who are generally shown graphic warnings in a laboratory or Internet environment at one point in time. Reliance on such laboratory exposures for testing fear appeals has been criticized.54 Although our small sample sizes require cautious interpretation of the results, study findings confirm differences in smokers’ reactions to graphic versus text-only cigarette warning labels.
Only two participants failed to complete all follow-up surveys in the randomized experiment, which may be due to our in-person recruitment of adults who had already completed our larger survey study, our increasing incentive structure, and the low burden on participants who were asked to affix stickers to their cigarette packs and complete a brief telephone survey three times during 1 week. These results are in contrast with those of Moodie et al.24 who knocked on doors in selected neighborhoods in Scotland and asked participants to use their own packs or transfer their cigarettes to plain brown packs with the same “Smoking Kills” text on the front and the diseased versus healthy lung graphic on the back for 2 weeks (randomly assigned). Participants received weekly reminders to use the correct packs and to return two surveys each week; however only 34% of participants completed the full study as intended.
Consistent with an eye-tracking study,23 smokers in the graphic labels condition in our more “real-world” experiment also reported significantly greater attention and correct recall compared with smokers in the text-only labels condition. The reported exposure to assigned warning labels was high across all conditions and avoidance was low. Participants who received text-only labels appeared to pay attention to the warning label much more often after the first follow-up (47%) compared with initial reports (<12%), perhaps in anticipation of being asked about the label in subsequent surveys. However, graphic warning labels consistently garnered more attention, and images were more often recalled accurately. Details of images were probably easier to recall than message details; however, our recall measure was general and did not probe for recall of both image and message elements. Text-only participants may have believed that since they had seen related text warnings for years that they accurately recalled what it said and spent less time looking at it as a result. Warning labels can only be effective if noticed and our results showed that graphic labels were better at getting smokers’ attention. Although the pattern of positive associations was similar, few graphic labels had significantly greater odds of making smokers think about health risks. The label showing a man smoking with a tracheotomy prompted thoughts about harms, but the qualitative data suggests mixed reactions. Although some felt it was persuasive, others noted the uniqueness of a smoker with a tracheotomy, which may reduce personal relevance and perceived susceptibility. Future studies should explore any negative effects of remembering the graphic image, but having no recall or incorrect recall of the warning’s message (e.g., thinking the label of the man smoking with a tracheotomy warned about lung cancer).
The behavioral impact of graphic and text warning labels did not differ; about one-third of all participants reported that each type of label prompted them to stop smoking even temporarily. The reason for this result is unknown. Previous studies have reported effects of graphic warning labels on forgoing a cigarette, quit attempts, or cessation after national implementation of graphic cigarette warning labels where no control condition existed. Rates of behavior change vary considerably in these studies (10%–27%), possibly due to differences in behavioral measures and follow-up intervals.14,15,19,55,56 Given our short follow-up, our measure of temporary behavioral effects is consistent with our expectation that few, if any, participants would report quit attempts lasting 24hr or more.
Self-referential thinking may be an important mediator of the impact of graphic cigarette warning labels. In previous studies, it has been associated with greater learning and recall, a positive attitude toward a product, and greater perceived risk and intention for health behavior change.27,57 Further, Dunlop and colleagues have concluded that media messages may promote both self-referential emotions (e.g., fear) and plot-referent emotions (e.g., sadness). Self-referential emotions have been associated with greater cognitive elaboration, engagement with a story, and greater perceived risk and intention.57,58 Graphic warning labels or other antitobacco media campaigns that prompt self-referential thoughts such as those reported by participants in this study (“Why am I still smoking?” or “What will it take for me to quit?”) may produce more perceived susceptibility and cessation attempts. Self-referential thinking was also illustrated when participants discussed the “mismatch” regarding their assigned label, and some responses revealed defensive reactions. Viewing others’ faces on warning labels may be distracting for some people and inhibit more self-referential thinking compared to impersonal images (i.e., diseased mouth).18 More research is needed to identify new methods and messages that will prompt effective self-referential thinking.59–61
Our mixed-methods study design provided unique qualitative data of the varied reactions to the cigarette warning labels. Such data are not meant to generalize to all smokers, but provide illustrations of authentic reactions to warning labels in a U.S. sample. Although defensive reactions were voiced by a minority of participants, reactance, and message rejection have been reported in previous studies of smokers exposed to graphic warnings,30,62 and self-exemption and normalizing the harm beliefs about smoking have been reported by smokers in previous studies.63,64 Fear arousal may prompt defensive responses, which reduce persuasion.65 In this study, defensive reactions were negatively related to looking at the label, thinking of health risks and quitting, and stopping smoking after seeing the warning label. Disturbing images may grab viewers’ attention, but individuals who feel vulnerable or threatened because the threat is personally relevant may be distracted from attending to the accompanying text warning as demonstrated in eye-tracking studies,66 as well as be more likely to “efficiently disengage” their attention from the image based on the results of studies measuring brain activity.67,68 The stage model of processing of fear-arousing communication posits that people who feel vulnerable to a severe threat will engage in defensive, but systematic information processing to criticize and minimize the threat.69 Smokers in our study mostly voiced counterarguments, which may be the most effective defensive strategy to resist attitude change.70 Counterarguing often involves attacks on the message or source credibility, which requires more conscious information processing or elaboration than simple message avoidance or blunting defenses. Such elaboration may instill greater confidence in one’s attitudes; thus, reducing the persuasive effect of the risk message. Several strategies for reducing defenses and increasing unbiased information processing and message acceptance have been examined, but more experimentation is needed before any of these strategies are likely to be used routinely in practice.60,71–76 Pre-testing warning labels before national implementation is warranted to identify particular labels or characteristics that prompt undesirable reactions such as reactance. Research on defensive reactions has been limited and few conceptual models and measures for defensive responses exist.33,63,77,78 More research is needed to determine the role and relative effects of different defensive reactions on attitude and behavior change.
Our results suggest qualitative differences in the “stickiness”79 of certain graphic images. Our participants clearly described images they remembered from their earlier participation in the larger survey study. Multiple participants explained why a particular graphic warning label would have been more effective or relevant to them than the label they were assigned, and this effect was not limited to those assigned text-only labels. Although previous research suggests that warning labels need to be refreshed and changed over time to reduce “wear-out effects,”80 it is also important to note that for some smokers, certain graphic images may linger in their thoughts and motivations to quit. Because specific graphic warning labels cannot be matched to individual smokers in the real world, selecting labels that appeal to wider audiences may improve their overall impact. Additionally, media campaigns that feature a variety of graphic images and role models can reinforce and augment the effects of specific graphic warning labels received by smokers that are less salient to them than others, and increase the elaboration, understanding, and personal relevance of the warnings.81
Limitations
The small sample size per condition reduces our ability to detect statistically significant differences between labels and increases the variability in our reported estimates, as illustrated by the large confidence intervals. Such variability also may be due to unmeasured moderator variables that could be examined in future studies, such as conceptual understanding of smoking risks and perceived relevance of each warning label. Further, we did not correct for the number of analyses performed which may increase Type I errors. The convenience sample and recruitment strategies may affect selection bias and limit the ability to generalize our findings. However, we sought to involve smokers from population subgroups that have higher than average rates of, and health disparities due to, smoking from multiple U.S. regions and settings. We relied on participants’ self-reported adherence to assess exposure to assigned warning labels rather than objective measures, but we found no differences across conditions. Having participants affix warning labels to their own packs may have produced greater effects than real-world exposure to pre-printed warnings on cigarette packs due to forced attention during the act of affixing the sticker on their pack and due to cognitive dissonance.31 Perhaps placing warning labels on their own cigarette packs induced feelings of hypocrisy among participants, which motivated attitude change.82,83 Although the type of warning label (text vs. graphic) is confounded with the placement on the pack (side vs. front), we used this design to mimic conditions in the real world, which we consider a strength. Both the novelty and the placement of the graphic warning label on the front of packs may be responsible for some of the observed effects. Similarly, the graphic image dominated participants’ recall of the label and interviewers did not probe for message-specific recall, thus limiting our ability to adequately compare message recall across groups.
Although the short follow-up period limited our ability to show changes in cognitions and behavior over longer periods of time, we wanted to maximize our ability to retain (and assure greater compliance among) such diverse participants in our unique longitudinal study. We did not expect warning labels to have an immediate and direct impact on behavior and we did not explicitly encourage participants to quit smoking. We did not specifically assess intention to quit or quit attempts in our brief follow-up surveys, but we were able to control for the effects of related variables from the larger survey (i.e., likelihood of using resources to quit and self-efficacy for quitting). Unlike previous studies that explored the effects of different images with similar text warnings or different warning themes,13,18,84 our study sought to explore reactions to the nine FDA selected graphic warning labels, which limited the possible comparisons within type of graphic label.
Our participants may have been more amenable to seeing graphic warning labels on cigarette packs than the larger population of smokers due to their willingness to participate in two studies exposing them to these graphic images. The frequency of defensive responding may be higher in the larger population of smokers. Our qualitative data comprised brief open-ended responses to interviewer prompts during the quantitative surveys. Trained research staff typed responses in real-time rather than transcribing them from audio-recordings due to time and resource limitations for this study. Although our method may lose some of participants’ natural language and emphasis, we are confident that the variety and nature of their thoughts and feelings were accurately captured. Our method of verifying only a subset of coded data (5%) after extensive training and discussions to finalize the codebook may have reduced the total number of quotes appropriately identified and coded for each variable examined, but the limitation of this method was less likely to influence consensus for the global, conceptual themes that emerged from the data.
Conclusions
Consistent with the results of prior observational and cross-sectional experimental research, our week-long study of real-world exposure to cigarette warning labels among adult U.S. smokers found that graphic cigarette warning labels were more effective than text-only warning labels in capturing the attention of smokers every time they opened their pack for a cigarette, in being correctly recalled, and in promoting more thoughts about the health harms of smoking. Because some graphic labels were more effective than others in eliciting these responses and because labels had no effect on behavior, future research should explore specific strategies to optimize the impact of warning labels. Because real-world distribution of warning labels cannot be tailored to individual differences, graphic images that encourage self-referential processing without increasing defensive reactions may be most effective.
Supplementary Material
Supplementary Appendix can be found online at http://www.ntr.oxfordjournals.org
Funding
Research reported in this publication was co-funded by the Food and Drug Administration (FDA) and the National Cancer Institute of the National Institutes of Health (NIH) as a supplement to the National Cancer Institute’s Centers of Excellence in Cancer Communication Research program (P50 CA95815-09S1; PI: MWK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA. The first author was also supported by an American Cancer Society Mentored Research Scholar Grant (CPPB-113766).
Declaration of Interests
None declared.
Supplementary Material
References
- 1. World Health Organization. 2012 global progress report on implementation of the WHO Framework Convention on Tobacco Control 2012. http://apps.who.int/iris/bitstream/10665/79170/1/9789241504652_eng.pdf Accessed January 22, 2014.
- 2. Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20:327–337. [DOI] [PubMed] [Google Scholar]
- 3. Kotnowski K, Hammond D. The impact of cigarette pack shape, size and opening: evidence from tobacco company documents. Addiction. 2013;108:1658–1668. [DOI] [PubMed] [Google Scholar]
- 4. Moodie C, Hastings G. Tobacco packaging as promotion. Tob Control. 2010;19:168–170. [DOI] [PubMed] [Google Scholar]
- 5. Wakefield M, Morely C, Horan JK, Cummings KM. The cigarette pack as image: new evidence from tobacco industry documents. Tob Control. 2002;11(suppl 1):i73–i80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Azagba S, Sharaf MF. The effect of graphic cigarette warning labels on smoking behavior: evidence from the Canadian experience. Nicotine Tob Res. 2013;15:708–717. [DOI] [PubMed] [Google Scholar]
- 7. Fathelrahman AI, Lin L, Borland R, et al. Stronger pack warnings predict quitting more than weaker ones: finding from the ITC Malaysia and Thailand surveys. Tob Induc Dis. 2013;11:20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang J, Chaloupka FJ, Fong GT. Cigarette graphic warning labels and smoking prevalance in Canada: a critical examination and reformulation of the FDA regulatory impact analysis. Tob Control. 2014;23i7–12. 10.1136/tobaccocontrol-2013-051170. [DOI] [PMC free article] [PubMed]
- 9. Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Showing leads to doing: graphic cigarette warning labels are an effective public health policy. Eur J Public Health. 2006;16223. .org/10.1093/eurpub/ckl037. [DOI] [PubMed] [Google Scholar]
- 10. Ruiter RAC, Kok G. Response to Hammond et al. Showing leads to doing, but doing what? The need for experimental pilot testing. Eur J Public Health. 2006;16:225. [Google Scholar]
- 11. Ruiter RAC, Kok G. Saying is not (always) doing: cigarette warning labels are useless. Eur J Public Health. 2005;15:329. [DOI] [PubMed] [Google Scholar]
- 12. Hammond D. Tobacco packaging and labeling policies under the U.S. Tobacco Control Act: research needs and priorities. Nicotine Tob Res. 2012;14:62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hammond D, Reid JL, Driezen P, Boudreau C. Pictorial health warnings on cigarette packs in the United States: an experimental evaluation of the proposed FDA warnings. Nicotine Tob Res. 2013;15:93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hammond D, Fong GT, McDonald PW, Cameron R, Brown KS. Impact of the graphic Canadian warning labels on adult smoking behaviour. Tob Control. 2003;12:391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hammond D, Fong GT, McDonald PW, Brown S, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers. Am J Public Health. 2004;94:1442–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cantrell J, Vallone DM, Thrasher JF, et al. Impact of tobacco-related health warning labels across socioeconomic, race and ethnic groups: results from a randomized web-based experiment. PLoS One. 2013;8:e52206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O’Hegarty M, Pederson LL, Nelson DE, Mowery P, Gable JM, Wortley P. Reactions of young adult smokers to warning labels on cigarette packages. Am J Prev Med. 2006;30:467–473. [DOI] [PubMed] [Google Scholar]
- 18. Thrasher JF, Carpenter MJ, Andrews JO, et al. Cigarette warning label policy alternatives and smoking-related health disparities. Am J Prev Med. 2012;43:590–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Willemsen MC. The new EU cigarette health warnings benefit smokers who want to quit the habit: results from the Dutch Continuous Survey of Smoking Habits. Eur J Public Health. 2005;15:389–392. [DOI] [PubMed] [Google Scholar]
- 20. Berg CJ, Thrasher JF, Westmaas JL, Buchanan T, Pinsker EA, Ahluwalia JS. College student reactions to health warning labels: sociodemographic and psychosocial factors related to perceived effectiveness of different approaches. Prev Med. 2011;53:427–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Emery LF, Romer D, Sheerin KM, Jamieson KH, Peters E. Affective and cognitive mediators of the impact of cigarette warning labels. Nicotine Tob Res. 2014;16:263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peters E, Romer D, Slovic P, et al. The impact and acceptability of Canadian-style cigarette warning labels among U.S. smokers and nonsmokers. Nicotine Tob Res. 2007;9:473–481. [DOI] [PubMed] [Google Scholar]
- 23. Strasser AA, Tang KZ, Romer D, Jepson C, Cappella JN. Graphic warning labels in cigarette advertisements: recall and viewing patterns. Am J Prev Med. 2012;43:41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moodie C, Mackintosh AM, Hastings G, Ford A. Young adult smokers’ perceptions of plain packaging: a pilot naturalistic study. Tob Control. 2011;20:367–373. [DOI] [PubMed] [Google Scholar]
- 25. Rooke S, Malouff J, Copeland J. Effects of repeated exposure to a graphic smoking warning image. Curr Psychol. 2012;31:282–290. [Google Scholar]
- 26. Dunlop SM, Wakefield MK, Kashima Y. The contribution of antismoking advertising to quitting: intra- and interpersonal processes. J Health Commun. 2008;13:250–266. [DOI] [PubMed] [Google Scholar]
- 27. Dunlop SM, Wakefield MK, Kashima Y. Pathways to persuasion: cognitive and experiential responses to health-promoting mass media messages. Commun Res. 2010;37:133–164. [Google Scholar]
- 28. Petty R, Cacioppo J. The elaboration likelihood model of persuasion. Adv Exp Soc Psychol. 1986;19:123–205. [Google Scholar]
- 29. Chang C. Enhancing self-referencing to health messages. J Consum Aff. 2011;45:147–164. [Google Scholar]
- 30. Süssenbach P, Niemeier S, Glock S. Effects of and attention to graphic warning labels on cigarette packages. Psychol Health. 2013;28:1192–1206. [DOI] [PubMed] [Google Scholar]
- 31. Festinger L. A Theory of Cognitive Dissonance. Vol 2 Stanford, CA: Stanford University Press; 1962. [Google Scholar]
- 32. Witte K. Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59:329–349. [Google Scholar]
- 33. McQueen A, Vernon SW, Swank PR. Construct definition and scale development for defensive information processing: an application to colorectal cancer screening. Health Psychol. 2013;32:190–202. [DOI] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2005–2012. Morb Mortal Wkly Rep. 2014;63:29–34. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6302a2.htm?s_cid=mm6302a2_w Accessed December 22, 2014. [PMC free article] [PubMed] [Google Scholar]
- 35. DeSantis C, Naishadham D, Jemal A. Cancer statistics for African Americans, 2013. CA Cancer J Clin. 2013;63:151–166. [DOI] [PubMed] [Google Scholar]
- 36. Ham DC, Przybeck T, Strickland JR, Luke DA, Bierut LJ, Evanoff BA. Occupation and workplace policies predict smoking behaviors: analysis of national data from the current population survey. J Occup Environ Med. 2011;53:1337–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Meyer PA, Yoon PW, Kaufmann RB. CDC Health disparities and inequalities report - United States, 2013. Morb Mortal Wkly Rep. 2013;62:3–5. http://www.cdc.gov/mmwr/pdf/other/su6203.pdf Accessed December 22, 2014. [PubMed] [Google Scholar]
- 38. Vander Weg MW, Cunningham CL, Howren MB, Cai X. Tobacco use and exposure in rural areas: findings from the Behavioral Risk Factor Surveillance System. Addict Behav. 2011;36:231–236. [DOI] [PubMed] [Google Scholar]
- 39. Borland R, Yong H-H, Wilson N, et al. How reactions to cigarette packet health warnings influence quitting: findings from the ITC four-country survey. Addiction. 2009;104:669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. ITC. International Tobacco Control Policy Evaluation Project http://www.itcproject.org/surveys. Accessed January 9, 2015.
- 41. Craik FIM, Lockhart RS. Levels of processing: a framework for memory research. J Verb Learn Verb Beh. 1972;11:671–684. [Google Scholar]
- 42. Houts P, Doak C, Doak L, Loscalzo M. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61:173–190. [DOI] [PubMed] [Google Scholar]
- 43. Miller S. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease: implications for cancer screening and management. Cancer. 1995;76:167–177. [DOI] [PubMed] [Google Scholar]
- 44. WWAMI Rural Health Research Center. Rural urban commuting area codes http://depts.washington.edu/uwruca/ruca-codes.php Accessed February 5, 2014.
- 45. Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 46. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New Jersey, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 47. Pampel FC. Logistic Regression: A primer. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- 48. Weber RP. Basic Content Analysis. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 1990. [Google Scholar]
- 49. Bernard HR. Research Methods in Anthropology. Plymouth, UK: AltaMira Press; 2011. [Google Scholar]
- 50. Maxwell JA. Qualitative Research Design: An Interactive Approach. 3rd ed. Thousand Oaks, CA: Sage Publications Inc; 2013. [Google Scholar]
- 51. Esterberg KG. Qualitative Research Methods in Social Research. Boston, MA: McGraw-Hill; 2002. [Google Scholar]
- 52. Pidgeon NF, Henwood KL. Using grounded theory in psychological research. In: Hayes N, ed. Doing Qualitative Analysis in Psychology. Hove, UK: Psychology Press; 1997:245–273. [Google Scholar]
- 53. Debevec K, Romeo JB. Self-referent processing in perceptions of verbal and visual commercial information. J Consum Psychol. 1992;1:83–102. [Google Scholar]
- 54. Hastings G, Stead M, Webb J. Fear appeals in social marketing: strategic and ethical reasons for concern. Psychol Market. 2004;21:961–986. [Google Scholar]
- 55. Hammond D, Fong G, Borland R, Cummings K, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: findings from the international tobacco control four country study. Am J Prev Med. 2007;32:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Koval JJ, Aubut JL, Pederson LL, O’Hegarty MO, Chan SSH. The potential effectiveness of warning labels on cigarette packages. Can J Public Health. 2005;96:353–356. http://www.jstor.org/stable/41994587. Accessed January 9, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dunlop S, Wakefield M, Kashima Y. Can you feel it? Negative emotion, risk, and narrative in health communication. Media Psychol. 2008;11:52–75. [Google Scholar]
- 58. Keller PA, Block LG. Increasing the persuasiveness of fear appeals: the effect of arousal and elaboration. J Consum Res. 1996;22:448–459. [Google Scholar]
- 59. Baldwin AS, Rothman AJ, Vander Weg MW, Christensen AJ. Examining causal components and a mediating process underlying self-generated health arguments for exercise and smoking cessation. Health Psychol. 2013;32:1209–1217. [DOI] [PubMed] [Google Scholar]
- 60. Glock S, Müller BCN, Ritter S. Warning labels formulated as questions positively influence smoking-related risk perception. J Health Psychol. 2013;18:252–262. [DOI] [PubMed] [Google Scholar]
- 61. Mevissen FEF, Meertens RM, Ruiter RAC, Schaalma HP. Bedtime stories: the effects of self-constructed risk scenarios on imaginability and perceived susceptibility to sexually transmitted infections. Psychol Health. 2012;27:1036–1047. [DOI] [PubMed] [Google Scholar]
- 62. Erceg-Hurn DM, Steed LG. Does exposure to cigarette health warnings elicit psychological reactance in smokers? J Appl Soc Psychol. 2011;41:219–237. [Google Scholar]
- 63. Oakes W, Chapman S, Borland R, Balmford J, Trotter L. ‘Bulletproof skeptics in life’s jungle’: which self-exempting beliefs about smoking most predict lack of progression towards quitting. Prev Med. 2004;39:776–782. [DOI] [PubMed] [Google Scholar]
- 64. Peretti-Watel P, Halfen S, Gremy I. Risk denial about smoking hazards and readiness to quit among French smokers: an exploratory study. Addict Behav. 2007;32:377–383. [DOI] [PubMed] [Google Scholar]
- 65. Umeh K, Stanley S. Effects of communicator credibility and fear on adaptive and maladaptive coping reactions to the HIV threat. J Appl Biobehav Res. 2005;10:183–198. [Google Scholar]
- 66. Brown SL, Richardson M. The effect of distressing imagery on attention to and persuasiveness of an antialcohol message: a gaze-tracking approach. Health Educ Behav. 2012;39:8–17. [DOI] [PubMed] [Google Scholar]
- 67. Kessels LTE, Ruiter RAC, Jansma BM. Increased attention but more efficient disengagement: neuroscientific evidence for defensive processing of threatening health information. Health Psychol. 2010;29:346–354. [DOI] [PubMed] [Google Scholar]
- 68. Kessels LTE, Ruiter RAC, Wouters L, Jansma BM. Neuroscientific evidence for defensive avoidance of fear appeals. Int J Psychol. 2014;49:80–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. de Hoog N, Stroebe W, de Wit J. The impact of fear appeals on processing and acceptance of action recommendations. Pers Soc Psychol Bull. 2005;31:24–33. [DOI] [PubMed] [Google Scholar]
- 70. Jacks JZ, Cameron KA. Strategies for resisting persuasion. Basic Appl Soc Psych. 2003;25:145–161. [Google Scholar]
- 71. Armitage CJ, Harris PR, Hepton G, Napper L. Self-affirmation increases acceptance of health-risk information among UK adult smokers with low socioeconomic status. Psychol Addict Behav. 2008;22:88–95. [DOI] [PubMed] [Google Scholar]
- 72. Block L, Williams P. Undoing the effects of seizing and freezing: decreasing defensive processing of personally relevant messages. J Appl Soc Psychol. 2002;32:803–833. [Google Scholar]
- 73. Das E, Vonkeman C, Hartmann T. Mood as a resource in dealing with health recommendations: how mood affects information processing and acceptance of quit-smoking messages. Psychol Health. 2012;27:116–127. [DOI] [PubMed] [Google Scholar]
- 74. Green MC, Clark JL. Transportation into narrative worlds: implications for entertainment media influences on tobacco use. Addiction. 2013;108:477–484. [DOI] [PubMed] [Google Scholar]
- 75. Kotz D, Huibers MJH, West RJ, Wesseling G, van Schayck OCP. What mediates the effect of confrontational counselling on smoking cessation in smokers with COPD? Patient Educ Couns. 2009;76:16–24. [DOI] [PubMed] [Google Scholar]
- 76. Mukherjee A, Dube L. Mixing emotions: the use of humor in fear advertising. J Consu Behav. 2012;11:147–161. [Google Scholar]
- 77. Blumberg SJ. Guarding against threatening HIV prevention messages: an information-processing model. Health Educ Behav. 2000;27:780–795. [DOI] [PubMed] [Google Scholar]
- 78. Dillard JP, Shen L. On the nature of reactance and its role in persuasive health communication. Commun Monogr. 2005;72:144–168. [Google Scholar]
- 79. Heath C, Heath D. Made to Stick: Why Some Ideas Survive and Others Die. New York, NY: Random House; 2007. [Google Scholar]
- 80. Borland R, Wilson N, Fong GT, et al. Impact of graphic and text warnings on cigarette packs: findings from four countries over five years. Tob Control. 2009;18:358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Brennan E, Durkin SJ, Cotter T, Harper T, Wakefield MA. Mass media campaigns designed to support new pictorial health warnings on cigarette packets: evidence of a complementary relationship. Tob Control. 2011;20:412–418. [DOI] [PubMed] [Google Scholar]
- 82. Aronson E, Fried C, Stone J. Overcoming denial and increasing the intention to use condoms through the induction of hypocrisy. Am J Public Health. 1991;81:1636–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Stone J, Aronson E, Crain AL, Winslow MP, Fried C. Inducing hypocrisy as a means of encouraging young adults to use condoms. Personality and Social Psychology Bulletin. 1994;20:116–128. [Google Scholar]
- 84. Cameron LD, Pepper JK, Brewer NT. Responses of young adults to graphic warning labels for cigarette packages [published online ahead of print April 26, 2013]. Tob Control. http://tobaccocontrol.bmj.com/content/early/2013/04/25/tobaccocontrol-2012–050645.full.pdf+html Accessed January 9, 2015 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.