Abstract
Background: Multiple sclerosis (MS) affects approximately 100,000 people in the United Kingdom, with rising emergency admissions to the hospital. The multiple sclerosis specialist nurse plays a pivotal role in managing MS care in the United Kingdom, and there is anecdotal evidence that this role can help avoid emergency presentations and unnecessary hospital admissions.
Methods: A retrospective service evaluation took place in one established MS nursing service. The impact of the introduction of proactive nurse-led management and a rapid response service on rates of emergency presentation, hospital admission, and bed use was examined. The primary intervention was the introduction of extra nursing hours (6 hours per week) and the reallocation of some routine administrative duties, which allowed the service to move to a proactive management model aimed at avoiding the need for unplanned care. In addition, a care pathway was implemented in the emergency department for patients with MS who did present.
Results: Reduction in utilization was from a mean of 2700 bed-days per year (2002–2006) to a mean of 198 bed-days per year (2007–2013).
Conclusions: During a 10-year period, moving from reactive management to proactive management demonstrated an increase in complex specialist nursing interventions and led to a decrease in emergency presentation and bed use at the local acute-care center.
Multiple sclerosis (MS) is a common cause of neurologic disability in younger adults. In Europe, MS is the leading cause of nontraumatic neurologic disability, with a prevalence of 83 per 100,000.1 Mackenzie et al.2 estimated that 126,669 people were living with MS in the United Kingdom in 2010 (203.4 per 100,000 population), with significant physical effects, such as pain, spasticity, visual impairment, continence issues, fatigue, and impaired mobility.3 In addition, patients can experience significant psychological effects. These range from distress at diagnosis, which can have subsequent consequences when developing coping strategies,4 to substantial biographical disruption.5,6 Another effect is cognitive impairment, and all of these factors have an effect on quality of life.7
In the United Kingdom, the number of emergency admissions to acute-care hospitals has continued to rise annually, despite general acceptance that admitting patients as emergency cases is disruptive, costly, and frequently avoidable. In a recent report, the Nuffield Trust reported that 35% of all inpatient stays were emergency admissions, at a cost of £11 billion.8 The unpredictable nature of MS can lead to the use of emergency and unscheduled care services. Hospital Episode Statistics (HES) data for 2010 to 2011 (England) show a total of 3779 emergency hospital admissions, with a mean length of stay of 20 days (median, 12.5 days) for patients with MS (mean age, 43 years).9 This has risen from a mean length of stay of 12.3 days in 2002 to 2006 for 4102 emergency admissions.9 Emergency management, particularly of symptoms, represents a challenge to the acute-care hospital, general practice, and patients with MS, who are unlikely to see a specialist in a timely manner if presenting in these settings.
The role of multiple sclerosis specialist nurse (MSSN) has developed since its introduction in the United Kingdom in the early 1990s, and is now well defined.10 One of the benefits of this role is the reduction of unnecessary emergency presentations and admissions via the emergency department. The evidence for this has been collected anecdotally and through comparisons with Patient at Risk of Readmission scores in English primary-care trusts10 and local successful admission avoidance initiatives that remain in the gray literature.
The cornerstone of specialist practice is the delivery of nursing interventions, proactive management, and vigilance. This evaluation examines the effectiveness of the introduction of a proactive case management model in 2006 to 2007 in a primary-care–based MS specialist nursing service in England with a caseload of 420 people with MS. The service had been provided by 0.6 whole-time-equivalent (WTE) band 7 and 0.4 WTE band 6 nurses and was extended by an additional 6 hours or 0.2 WTE band 6 MSSN in 2006 to 2007. The extra 0.2 WTE MSSN allowed the development of a rapid response team approach using proactive case management.11–13 There was also a refocus of working practices (the reallocation of some administrative work to a lower-band worker, allowing more patient contact time) and an emergency care pathway into the local emergency department for patients presenting with MS-related morbidity.
The evaluation has a particular focus on MS emergency management and service satisfaction of patients and general practitioners. Before introduction of the proactive management model, the mean number of emergency admissions for MS at the local acute-care center was 225 per year (range, 200–250 during 2003–2006 admitted for issues related to MS). Examination of these cases showed that standard practice was to admit for a neurologic review as the default.
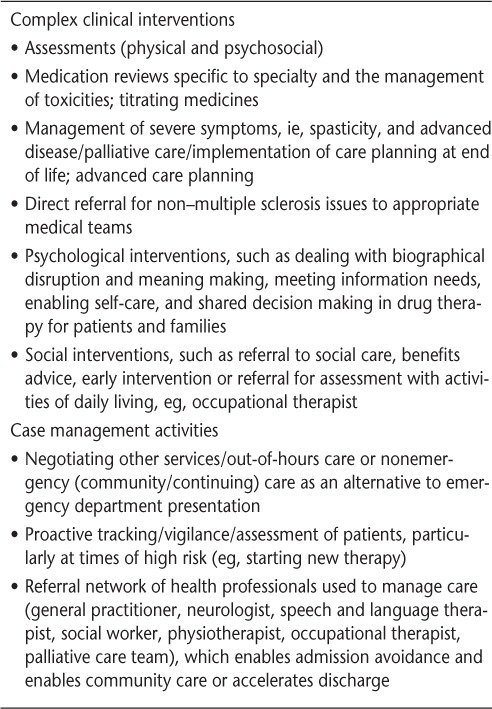
A previous evaluation of the service14 examined the reasons for presentation to local emergency care providers by people with MS. Although specific case-by-case data were not collected, according to thematic local data, the most common reasons for presentation were relapse, infection (chest or urinary tract), breakdown in social care provision, psychological problems or anxiety causing distress and somatic presentation, and toxicity due to medication; retrospective analysis14 demonstrated avoidable issues for which a series of interventions could be initiated proactively. These interventions are shown in Table 1 and include intensive case management using a high level of nursing vigilance at times of increased risk and planned and managed admission for further treatment rather than default to the emergency department. These interventions included an assessment of the issue and the actual risk from an MS expert nursing perspective and introduction of a management plan for common presentations (rather than the admission as default), which has been described previously.14
Table 1.
Examples of nursing interventions introduced or increased as a result of extra resources
This study did not seek to perform an economic evaluation; however, costs locally were calculated to be approximately £2000 per emergency admission. In this study, the commonly used National Health Service Institute for Innovation and Improvement15 figure of £250 per bed-day is used as part of the retrospective service evaluation.
Materials and Methods
The geographic area served by the MSSN service has one acute trust with an emergency department, which was the emergency care provider for the population served by the MSSN service. The appointment of the extra 6 MSSN hours and the reallocation of some administrative work allowed more time to be spent on proactive as opposed to reactive case management and a rapid response service to emergency physical and psychosocial issues. A collaborative approach was also taken with the local emergency department, leading to the development of an evidence-based16 pathway14 for those presenting with MS.14 This allowed for a structured assessment to better manage risk to guide treatment of immediate issues and then discharge back to the expert nurse for community follow-up.
To evaluate the impact of this change in management, the Health and Social Care Information Centre provided HES data for presentation and admission of the World Health Organization International Classification of Diseases, Tenth Revision (ICD-10) code G35 (Multiple Sclerosis) at the local acute trust for 2007 to 2013 (6 years). For 2002 to 2006 (the 4-year period before the implementation period), data were obtained via the HES online self-service facility, which was available until April 2013.
The HES search for the period after implementation (2007–2013) included arrival mode, attendance category (ie, initial or follow-up), disposal (ie, destination), duration to assessment, duration to treatment, duration to conclusion, duration to departure, source of referral, clinical diagnosis (including subanalysis), treatment, and current primary-care trust of residence; this included linkage from ICD-10 code to accident and emergency. The self-service data set used for the pre-implementation period did not allow for this level of detail and so captured only emergency admission and length of stay (mean and median per year).
To allow discrimination between those presenting with issues relating to their MS and those presenting for other reasons (eg, road traffic accidents) but with an incidental diagnosis of MS, the HES diagnosis and treatment codes were used in the post-implementation group,17 and locally collected data (reason for admission) were used in the pre-implementation group.
To further evaluate the service, questionnaires were developed to gauge satisfaction with the service by the patient/family (n = 35) and the general practitioner (n = 30). These were 7- and 10-item questionnaires, respectively, examining issues such as overall satisfaction, speed of service, satisfaction with the level of intervention, and other experience-related items.
This was a service evaluation using secondary data analysis and, therefore, was not presented to an ethics committee. The evaluation was reviewed internally.
Results
For the reasons cited previously herein, the data for 2002 to 2006 are not matched to the post-2007 data set in terms of fields. Thus, comparisons are made with the post-implementation group where possible but otherwise with national data.
In 2002 to 2006 (before implementation), there were a mean of 225 emergency admissions per year for the ICD-10 code for MS at the acute-care center. Locally collected data correlate with this and show that MS was the primary reason for admission. The mean length of stay was 12 days.
Between 2007 and 2013 (after implementation), there were 48 accident and emergency presentations at the local acute-care center with both an ICD-10 code for MS and an MS-related reason for presentation. Of these 48 patients, 33 were admitted and 15 were either discharged or referred to another health-care professional (one is coded as refused). Overall, the mean length of stay in the 2007 to 2013 group was 6 days. The mean total admission bed-days per year in the 2002 to 2006 (before implementation) group was 2700 bed-days and in the 2007 to 2013 (after implementation) group was 198 bed-days (both of these values are based on the mean length of stay).
Based on £250 per bed-day,15 the 2002 to 2006 (before implementation) group seems more resource intensive against the cost of the service than the 2007 to 2013 (after intervention) group. The rate of specialist nurse–recorded complex interventions rose (Figure 1), which would be expected as a component of proactive management.
Figure 1.
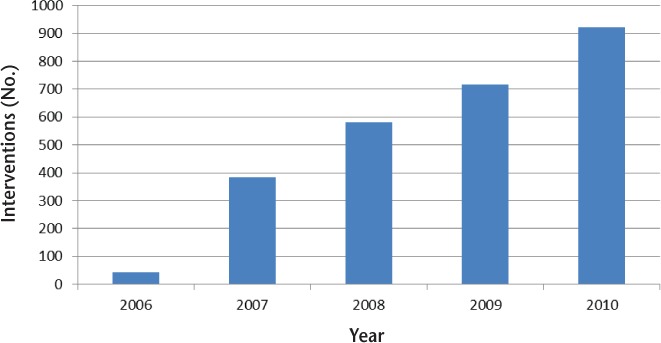
Complex nursing interventions delivered to avoid emergency admissions as a component of proactive management
Both patients/families and general practitioners reported an improvement in service and high levels of satisfaction. Of the 30 general practitioners surveyed, 14 (46.7%) responded. All 14 respondents said that they would use the service again and considered it essential in managing care, and 9 (64.3%) felt that they were sending fewer patients for emergency or acute unscheduled care because of the service. Thirteen general practitioners (92.9%) said it was an improvement over previous care, and 12 (85.7%) thought that it eased their workload. Twelve respondents (85.7%) thought that it improved outcomes for patients.
Of the 35 patients/families surveyed, 13 responded. All the respondents stated that overall they were satisfied with the service, and all were also satisfied in terms of speed and level of support from the MSSNs.
Discussion
During a 10-year period, moving from reactive management to proactive management demonstrated an increase in complex specialist nursing interventions and led to a decrease in emergency presentations and bed use at the local acute-care center. The aim of this study was to evaluate the effect on emergency presentation and hospital admission in terms of emergency bed use by implementing an expert level of nursing practice in the community, which allows for proactive management and rapid response to emerging issues rather than default to emergency care. It would be difficult to differentiate between the impact of proactive case management and the introduction of the emergency care pathway, but the reduction in presentation is likely to have been due to the move to proactive rather than reactive management because all other factors remained static in the service.
The proactive case management of MS plus rapid response to emerging clinical situations (physical and psychosocial) is central to reducing emergency care but requires clinical acumen and expertise because the nursing interventions offered were complex and multiple in nature, similar to those required in other long-term conditions.18,19 It is likely that this level of advanced practice could be offered only by an experienced practitioner.
Within the locality of the study, this work demonstrates the value of a community-based MS nursing service, both in cost savings to the local economy and in reacting to service users' needs to receive care closer to home in a prompt, timely manner. Although before the evaluation there was confidence that the service was providing value for money and reducing unnecessary hospital attendance, this evaluation demonstrated the sheer scale of the impact of the straightforward intervention, and the reductions are far beyond what had been anticipated. Demonstrating value for money in the local health economy is paramount to securing future services, and emergency care is one of the most expensive methods of delivering health care in England. Although no economic evaluation was performed in this study, the results suggest the need to continue to invest in a community-based MS nursing service that uses a proactive management model and builds strong working relationships with the local acute-care center.
This was a retrospective study of available data as part of a service evaluation with a small sample size. The data set is incomplete because of changes in the recording of, and restrictions on accessing, national data (HES) and only partial collection of local data. For this reason, few demographic data were available, and no inferential statistical analyses were performed. A larger, well-designed study would yield far more data and be more methodologically robust. Further research is needed to determine whether this effect is a common one.
Conclusion
Over a 10-year period, moving from reactive management to proactive management demonstrated an increase in complex specialist nursing interventions and led to a decrease in emergency presentations and bed use at the local acute-care center. There are approximately 235 WTE MSSNs20 in the United Kingdom. If workload permits proactive management in partnership with patients, caregivers, and primary care, it is likely that this group represents a good return on investment, and, thus, an economic evaluation of these roles would be of benefit in informing the commissioning of these services.
PracticePoints.
The work of the MS specialist nurse is pivotal to care, particularly in avoiding unnecessary emergency admissions to the hospital.
Moving from reactive management to proactive case management can cause a large decrease in unnecessary emergency admissions and higher satisfaction with care.
Acknowledgments
We thank Vicki Matthews, nurse advisor, MS Trust (until 2012); Carolyn Derry and Richard Glasspool, Northampton Healthcare National Health Service Trust; Helen Newick for assistance with data handling; and Geoff Punshon for assistance with preparation of the manuscript.
Footnotes
From the School of Health and Social Care, London Southbank University, London, UK (AL); Northamptonshire Healthcare National Health Service Foundation Trust and Multiple Sclerosis Trust, Northampton, UK (DQ); and Multiple Sclerosis Trust, London, UK (AB).
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This study was unfunded, but the HES extraction costs were funded by the MS Trust.
References
- 1.Koutsouraki E, Costa V, Baloyannis S. Epidemiology of multiple sclerosis in Europe: a review. Int Rev Psychiatry. 2010;22:2–13. doi: 10.3109/09540261003589216. [DOI] [PubMed] [Google Scholar]
- 2.Mackenzie IS, Morant SV, Bloomfield GA, MacDonald TM, O'Riordan J. Incidence and prevalence of multiple sclerosis in the UK 1990–2010: a descriptive study in the General Practice Research Database. J Neurol Neurosurg Psychiatry. 2014;85:76–84. doi: 10.1136/jnnp-2013-305450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scolding N, Wilkins A. Multiple Sclerosis. Oxford, UK: Oxford University Press; 2012. The causes and mechanisms of multiple sclerosis; pp. 23–31. [Google Scholar]
- 4.Johnson J. On receiving a diagnosis of multiple sclerosis: managing the transition. Mult Scler. 2003;9:82–88. doi: 10.1191/1352458503ms856oa. [DOI] [PubMed] [Google Scholar]
- 5.Bury M. Chronic illness and biographical disruption. Soc Health Illness. 1982;4:167–182. doi: 10.1111/1467-9566.ep11339939. [DOI] [PubMed] [Google Scholar]
- 6.Green G, Todd J, Pevalin D. Biographical disruption associated with multiple sclerosis: using propensity scoring to assess the impact. Soc Sci Med. 2007;55:524–535. doi: 10.1016/j.socscimed.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez O, Baumstarck-Barrau K, Simeoni M, Auquier P. Patient characteristics and determinants of quality of life in an international population with multiple sclerosis: assessment using the MusiQoL and SF-36 questionnaires. Mult Scler. 2011;17:1238–1249. doi: 10.1177/1352458511407951. [DOI] [PubMed] [Google Scholar]
- 8.Nuffield Trust. Trends in Emergency Admission 2004–9: Is Greater Efficiency Breeding Inefficiency? London, UK: Nuffield Trust; 2010. [Google Scholar]
- 9.Health and Social Care Information Centre. Hospital Episode Statistics. http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=202. Accessed August 1, 2012.
- 10.United Kingdom Multiple Sclerosis Specialist Nurse Association. Multiple Sclerosis Specialist Nurses: Adding Value and Delivering Targets. Stevenage, UK: UKMSSNA; 2006. [Google Scholar]
- 11.Department of Health. Supporting People with Long-Term Conditions: Liberating the Talents of People Who Care for People with Long-Term Conditions. London, UK: TSO London; 2005. [Google Scholar]
- 12.Oliver S, Leary A. Return on investment: workload, complexity and value of the CNS. Br J Nurs. 2012;21:32–37. doi: 10.12968/bjon.2012.21.1.32. [DOI] [PubMed] [Google Scholar]
- 13.Baxter J, Leary A. Productivity gains by specialist nurses. Nurs Times. 2011;107:15–17. [PubMed] [Google Scholar]
- 14.Quinn D. A collaborative care pathway to reduce multiple sclerosis admissions to secondary care. Br J Neurosci Nurs. 2011;7:497–499. [Google Scholar]
- 15.NHS Institute for Innovation and Improvement. Return on Investment (ROI) calculator. http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/Return_on_Investment_(ROI)_calculator.html. Accessed June 2013.
- 16.National Institute for Health and Clinical Excellence. Multiple Sclerosis: Management of Multiple Sclerosis in Primary and Secondary Care. London, UK: National Institute for Health and Clinical Excellence; 2003. [PubMed] [Google Scholar]
- 17.Health and Social Care Information Centre. Hospital Episode Statistics Data Dictionary (Accident & Emergency) Leeds, UK: Health and Social Care Information Centre; 2009. pp. 5–97. [Google Scholar]
- 18.Anionwu E, Leary A. Understanding the Contribution of the Sickle Cell & Thalassaemia Specialist Nurses: A Summary Report. NHS Screening Programme 2012. http://www.tinyurl.com/sickle-cell-thal. Accessed November 2013.
- 19.Mackie D, Warren M, Leary A. The complexity of non face-to-face work with patients affected by metastatic breast cancer and their carers: the “hidden consultations.”. Eur J Oncol Nurs. 2012;16:460–464. doi: 10.1016/j.ejon.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Multiple Sclerosis Trust. Defining the Value of MS Specialist Nurses. Letchworth, UK: Multiple Sclerosis Trust; 2012. [Google Scholar]


