Abstract
Background: People with multiple sclerosis (MS) fall frequently, and there are few clinically valid tools to measure the risk factors for falls. We assessed the unidimensionality of the 7-item Falls Efficacy Scale–International (FES-I), a measure of fear of falling, and determined whether the 7-item FES-I is associated with recurrent falls in people with MS.
Methods: Falls were counted prospectively for 6 months using fall calendars in 58 people with MS (age, 18–50 years; Expanded Disability Status Scale score, 0–6). The FES-I was administered at baseline, and its unidimensionality was assessed by confirmatory factor analysis. The relationship between FES-I score and future falls, after adjusting for recurrent falls in the past year, was assessed by logistic regression.
Results: Fifty-four participants who completed all assessments were included in the analysis. Goodness-of-fit indices confirmed a single-factor solution for the 7-item FES-I (discrepancy χ2, P = .101; Tucker-Lewis index, 0.953; comparative fit index, 0.969; root mean square error of approximation, 0.098). There was a significant association between fear of falling and falls in the following 3 months, independent of recurrent falls in the past year (odds ratio = 1.22, 95% confidence interval, 1.04–1.43, P = .016).
Conclusions: The 7-item FES-I demonstrates good construct validity, allowing the total score to be used as a measure of fear of falling in people with MS. Fear of falling, as measured by the 7-item FES-I, is associated with future recurrent falls independent of past recurrent falls in people with MS.
People with multiple sclerosis (MS) fall frequently.1 Between 52% and 63% of people with MS fall at least once in a 2- to 6-month period,2–4 and recurrent falls are also common in this population.5 Approximately 50% of people with MS who fall once during a study period also experience recurrent (two or more) falls.2,3 Studies in older adults6 and people with Parkinson's disease7 have demonstrated that recurrent falls (two or more falls in a year) are more clinically relevant than a single fall because recurrent falls are likely to indicate worse health. Given the high prevalence of recurrent falls in people with MS, the factors associated with recurrent falls in this population warrant further investigation.
Risk factors associated with falls may be physiologic or psychological. To date, most studies have focused on assessing the association between physiologic factors and falls,2,8–10 and there is a paucity of research on the association between psychological factors and falls in MS.11 Psychological factors related to fatigue12 and balance confidence13 have been previously evaluated and have been found to be associated with falls in people with MS. Fear of falling, measured in a variety of ways, has also been identified as a psychological risk factor for falls in MS,3,14,15 and there is a high prevalence of fear of falling in this population.14
Fear of falling and falls are interrelated. Older adults with increased fear of falling are at higher risk for falls, and individuals who fall are at a higher risk for developing fear of falling.16 This results in a vicious cycle of falls, fear of falling, functional decline, and more falls. Given the variability in the measurement of fear of falling in previous studies,8,14,15 and the interdependence between falls and fear of falling, it remains uncertain whether fear of falling independently predicts recurrent falls in people with MS.
The Falls Efficacy Scale–International (FES-I) is a valid and reliable measure of fear of falling in older adults,17–19 and recently the psychometric properties of this tool were assessed in people with MS using item response theory.20 The authors found that the FES-I provided valid assessments of fear of falling and that the shortened 7-item version of the original 16-item FES-I had better psychometric properties in people with MS.20 In practice, use of the total score of a rating scale to represent a single underlying construct assumes unidimensionality of the scale.21 Because a lack of unidimensionality can lead to ambiguity and misinterpretation of the score,22 we evaluated this psychometric property by applying the 7-item FES-I in a sample of people with MS using confirmatory factor analysis. We hypothesized that the 7-item FES-I would be unidimensional, indicated by a single-factor solution. We then evaluated the association between the construct of “fear of falling” as measured by the FES-I and future falls in the prospective cohort design. We hypothesized that the total score on the 7-item version of the FES-I would predict the risk of recurrent falls (two or more falls) in people with MS independent of past recurrent falls. In addition, we evaluated the association between the total score on the 7-item version of the FES-I and falls and injurious falls in the following 6 months.
Methods
Human Subjects Protections
The institutional review boards of the Department of Veterans Affairs medical center and the academic medical center where this prospective cohort study was conducted approved the study protocol. All potential participants were given a verbal explanation of the experimental protocol, a detailed informed consent document, and an opportunity to ask questions. All the participants gave written informed consent to participate in this study.
Participants
Fifty-eight individuals with MS were recruited for a study of mechanisms of imbalance and falls in MS at an academic medical center and its affiliated Department of Veterans Affairs medical center in the northwestern United States. Potential participants were recruited using flyers posted at the clinics of these institutions and via flyers and announcements at patient education programs and MS support groups. Of the 58 participants, 54 completed all aspects of data collection and were included in this analysis (Figure 1).
Figure 1.
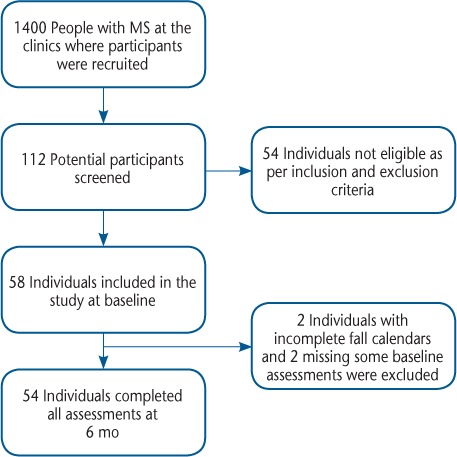
Participant recruitment and retention
MS, multiple sclerosis.
Inclusion and Exclusion Criteria
The participants in this study met the following inclusion criteria: confirmed diagnosis of MS by the McDonald criteria23; any subtype of MS, including relapsing-remitting, primary progressive, or secondary progressive24; aged 18 to 50 years; mild-to-moderate MS disability as defined by an Expanded Disability Status Scale (EDSS) score of 6.0 or less25; willing and intellectually able to understand and sign an informed consent form and to adhere to protocol requirements; sufficient motor function to complete a written daily record of falls for 6 months; and community dwelling.
MS severity was assessed at baseline using the EDSS,25 which is based on a clinical neurologic examination. Each participant was assigned an EDSS step from 0 to 10. Step 0 indicates normal neurologic function and step 10 indicates death due to MS. Step 6, the highest score among participants in this cohort, indicates intermittent or unilateral constant assistance (cane, crutch, or brace) required to walk approximately 100 m with or without resting.
The following exclusion criteria were applied: a self-reported musculoskeletal or neurologic condition other than MS known to affect balance or gait and to be associated with falls, such as a lower-extremity joint replacement, peripheral neuropathy, a vestibular disorder, alcoholism, stroke, or seizure; unable to follow directions in English; unhealed bone fractures or other conditions that put individuals at risk for injury during balance testing; and blindness (corrected visual acuity worse than 20/200).
Study Instruments
The FES-I was completed by all the participants. This scale assesses concern for falling while performing activities that range from basic (eg, getting dressed, getting in and out of a chair, and reaching up and bending down) to more physically demanding (eg, walking on a slope and going out to social events). Participants indicated their level of concern about falling while performing each activity on a 4-point scale, where 1 is “not concerned at all” and 4 is “very concerned.”17 The 16-item FES-I was administered to all the study participants, and the responses to the subset of items that composed the 7-item FES-I were used to calculate the 7-item FES-I score. In the case of missing responses, total scores were calculated using scoring criteria reported in earlier validation studies.17,18 The different versions of the FES-I are available at the Prevention of Falls Network Europe website (http://www.profane.eu.org/fesi.html).
In addition to the FES-I, participants completed a demographic data and retrospective fall questionnaire at baseline. The questionnaire asked how many times the participant recalled having fallen in the previous 12 months and how many of these falls resulted in injuries such as a bruise, cut, graze, pain, or other trauma.
Future fall events were measured prospectively using paper fall calendars. At the baseline visit, all the participants were provided with monthly fall calendars to record their falls and fall-related injuries (ie, a bruise, cut, graze, pain, or other trauma) each day. A fall was defined as any unanticipated event that results in a participant coming to rest on the ground, floor, or lower surface.26,27 At the end of each month, participants mailed back the single page providing the month's fall record. If the page was not received within 1 week after the end of the month, a research assistant telephoned the participant to ask for the page to be sent in. For analysis, total fall and injurious fall counts for the 6 months after the baseline visit were determined. The fall variable was dichotomized as “fallers” (at least one fall) or “nonfallers” (no falls); “recurrent fallers” (two or more falls) or “nonrecurrent fallers” (one or no falls); and “injurious fallers” (at least one injurious fall) or “noninjurious fallers” (no injurious falls).
Statistical Analysis
All the analyses were performed using Stata version 12.1 software (StataCorp, College Station, TX), and a significance level of P < .05 was set for all hypothesis testing. Descriptive statistics were used to assess the central tendency and variability of all the measured variables. To compare means of continuous variables, Mann-Whitney U tests and t tests were performed for nonparametric and parametric data, respectively. Ordinal variables were compared using χ2 tests.
The distribution of the total scores from the 7-item FES-I was first assessed as a continuous variable. Then the reliability and construct validity of the 7-item FES-I was assessed. To evaluate reliability, the Cronbach α was calculated. Confirmatory factor analysis was used to assess the construct validity, and commonly accepted confirmatory factor analysis fit indices (χ2, Tucker-Lewis index [TLI], comparative fit index [CFI], and root mean square error of approximation [RMSEA]) were used to assess the goodness of fit. The a priori hypothesis was that the 7-item version of the FES-I represents a single underlying construct.
Logistic regression was used to assess the relationship between the total score on the 7-item FES-I and being a recurrent faller in the following 3 or 6 months. Relationships were tested after adjustment for recurrent falls in the past year, EDSS score, age, and sex.
Results
Demographic and Baseline Characteristics
Fifty-four participants (93.1%) completed all the baseline assessments and the 6-month prospective fall counts and were included in the analysis (Table 1). The mean age of the participants was 39.6 years, and the female-to-male ratio was 2.2 to 1. A total of 94.4% of the participants had relapsing-remitting MS, and 5.6% had the secondary progressive type. The mean EDSS score at baseline was 2.7 (range, 0–6). At baseline, 41 participants (75.9%) reported at least one fall in the past year, and 34 (63.0%) reported two or more falls in the past year. In addition, 24 participants (44.4%) reported at least one injurious fall in the past year.
Table 1.
Demographic and fall characteristics of the 54 study participants
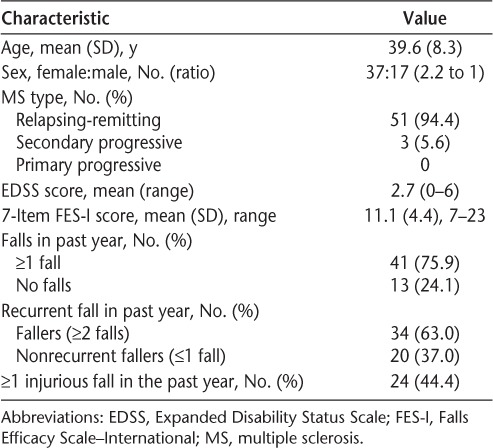
There were some significant differences in baseline EDSS and FES-I scores between recurrent and nonrecurrent fallers over the previous year (Table 2). People with MS who fell recurrently in the previous year had a higher 7-item FES-I mean score (12.1 vs. 9.4, P = .01). The mean EDSS score was also higher for past recurrent fallers than for nonrecurrent fallers (3.1 vs. 2.1, P = .01); however, there were no statistically significant differences in the average age or the distribution of men and women between recurrent and nonrecurrent fallers at baseline.
Table 2.
Characteristics of recurrent and nonrecurrent fallers at baseline
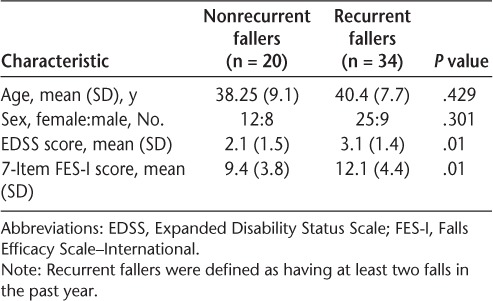
Unidimensionality of the 7-Item FES-I
For the 54 participants who completed all phases of data collection, the baseline mean (SD) score on the 7-item FES-I was 11.1 (4.4), and the range of the total score was 7 to 23. Scores on the 7-item FES-I were not normally distributed (kurtosis: 3.27) and were skewed to the right (skewness: 1.07). The Cronbach α was 0.91 for the 7-item FES-I scale, indicating high internal reliability.
The unidimensionality of the 7-item FES-I was assessed using confirmatory factor analysis with data from 52 individuals. Two participants did not answer one question each and were, therefore, excluded from this analysis. The goodness-of-fit indices for a one-factor solution are presented in Table 3. The discrepancy χ2 statistic, TLI, CFI, and RMSEA all supported a unidimensional measurement construct for the 7-item FES-I as applied to this sample of people with MS.
Table 3.
Model fit statistics for confirmatory factor analysis of the 7-item FES-I (n = 52)
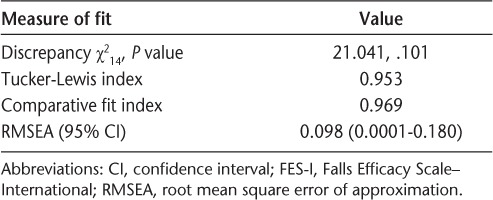
Fear of Falling as Measured by the 7-Item FES-I as a Predictor of Recurrent Falls
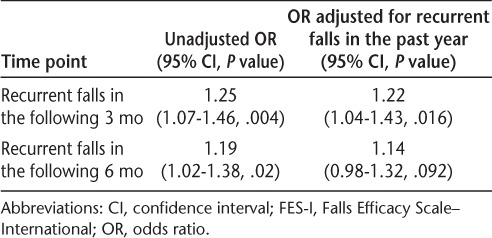
The crude and adjusted odds ratios (ORs) describing the relationship between fear of falling (as measured by the 7-item FES-I) and recurrent falls are shown in Table 4. In the bivariate analysis, we found that fear of falling was strongly associated with recurrent falls in the following 3 and 6 months. For each point increase in the 7-item FES-I total score, the odds of recurrent falls in the following 3 and 6 months increased by 25% and 19%, respectively.
Table 4.
Unadjusted and adjusted associations between scores on the 7-item FES-I and the risk of future recurrent falls
In multivariate analysis, we explored the effects of age, sex, and EDSS score (measured at baseline) on the relationship between the fear of falling (as measured at baseline) and falls in the following 6 months by adding each of these covariates one at a time into the model to identify whether any of these variables were confounders, that is, whether the point estimate of the OR changed by more than 10%. We found that the estimate of association between fear of falling and future recurrent falls did not change after adjusting for age, sex, and EDSS score, confirming that these variables did not appreciably confound the relationship between fear of falling and falls in people with MS. Thus, age, sex, and EDSS score were not retained in the final multivariate model to avoid unnecessary complex high dimensionality.
To test the principal hypothesis, that is, whether the total score on the 7-item version of the FES-I could predict the risk of recurrent falls (two or more falls) in people with MS, independent of past recurrent falls, we adjusted for past recurrent falls in the final model. We found that the total score on the 7-item FES-I was predictive of future recurrent falls: for each point increase in the 7-item FES-I total score, the odds of recurrent falls in the following 3 and 6 months increased by 22% and 14%, respectively. After adjusting for past recurrent falls, the 7-item FES-I total score was also found to be significantly associated with recurrent falls in the following 3 months (OR = 1.22; 95% confidence interval, 1.04–1.43; P = .016), and there was a trend toward significance for an association with recurrent falls in the following 6 months (OR = 1.14; 95% confidence interval, 0.98–1.32; P = .092).
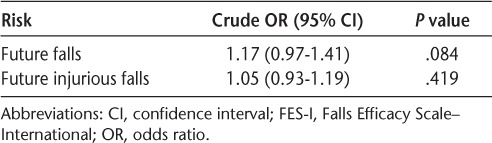
The relationships between fear of falling (as measured by the total score on the 7-item FES-I) and falls and injurious falls in the following 6 months are summarized by the ORs presented in Table 5. We found that fear of falling was not significantly associated with either falls or injurious falls in the following 6 months.
Table 5.
Unadjusted and adjusted associations between scores on the 7-item FES-I and the risk of future falls and future injurious falls in the following 6 months
Discussion
This analysis demonstrates that in people with MS, the 7-item FES-I is unidimensional and that fear of falling, as measured by the 7-item FES-I, predicts recurrent falls in the following 3 months, independent of falls in the past year. At the 6-month time point, the association does not reach statistical significance.
Confirmation of a single-factor solution supports the findings of a previous study that the 7-item FES-I has good construct validity in people with MS.20 The unidimensionality of the 7-item version of the scale justifies using the total score on the 7-item FES-I to represent the construct of fear of falling in people with MS. The fit indices evaluated in this study, including the χ2 test of model fit, the CFI, and the TLI, support this unidimensionality.28 The RMSEA also supported a single-factor model; although the point estimate was greater than 0.05, the lower limit of the 90% confidence interval for the RMSEA is considerably smaller than 0.05, which indicates acceptable model fit.29
The present study addresses an important gap in understanding the relationship between fear of falling and falls in people with MS. Previous cross-sectional studies have shown an association between fear of falling and an increased risk of falls in people with MS.3,14 The present study is the only study to assess the effect of past falls on this relationship. We assessed whether previous falls modify the relationship between fear of falling and future falls, as past falls are a strong predictor of future falls in people with MS.30 We found that fear of falling, as measured by the 7-item FES-I, is associated with recurrent falls in the following 3 months independent of past recurrent falls. The association between fear of falling and falls in the following 6 months was not statistically significant after adjusting for past recurrent falls. Although the association between fear of falling and falls in the following 6 months is attenuated with adjustment for past recurrent falls, the point estimate of the OR differs by less than 10% (14% compared with 19% increase in odds per point increase in the 7-item FES-I score), suggesting that the past recurrent falls are not likely confounding this association.
Although we found that fear of falling as measured by the total score on the 7-item FES-I was significantly associated with future recurrent falls in 3 months, the relationship between fear of falling and future falls or future injurious falls was not statistically significant. In people with Parkinson's disease, clinical measures of fear of falling, strength, and walking ability are known to be different between single fallers and recurrent fallers.7 It is not known whether this holds true for people with MS. Further research is warranted to investigate the difference in the relationships between fear of falling and characteristics of falling (recurrent falls vs. any falls vs. injurious falls) in people with MS.
Three previous studies have assessed fear of falling as a risk factor for prospectively counted falls in people with MS. Nilsagard et al.4 and Gunn et al.8 did not find fear of falling to be associated with falls in the following 3 months, whereas van Vliet et al.20 found that individuals who report recurrent falls in the following 6-month period have a higher fear of falling. This inconsistency among studies may be due to differences in how fear of falling was assessed or differences in the level of physical activity in these cohorts. Whereas Nilsagard et al. used a single question to assess fear of falling, we used the 7-item version of the FES-I. Gunn et al. used the 16-item FES-I, and van Vliet et al. used both the 16- and 7-item versions of the FES-I. Studies in older adults have found that a single-item question to assess fear of falling is less sensitive than a multi-item questionnaire.31,32 In addition, physical activity may mediate the relationship between fear of falling and future falls, and the level of activity may have differed among these cohorts.33 We recommend that future studies of people with MS use multi-item scales to assess fear of falling and also include measures of physical activity to evaluate the impact of this variable on the relationship between fear of falling and falls.
How fear of falling increases the risk of falls is unknown. The association between fear of falling and falls may reflect shared physiologic risk factors, such as increased postural instability.34,35 Fear of falling may also result in curtailment of activity and subsequent deconditioning that then increases the risk of falls.15,36 Additional studies are needed to more fully understand this complex relationship.
A strength of the present study was the prospective ascertainment of falls using daily calendars, thus minimizing information bias. Furthermore, minimal loss to follow-up reduced the possibility of a differential bias (93.1% of the participants completed the study at 6-month follow-up). In addition, we studied fear of falling in a younger cohort of people with MS, in whom the phenomenon has rarely been assessed.
There are several limitations to this study that restrict the generalizability and interpretation of the results. The small sample size decreases the power of the study. The absence of participants with primary progressive MS, the EDSS score upper limit of 6.0, and the upper age limit of 50 years limit the generalizability of these results. In addition, the participants in this study were recruited for a study of balance and falls, which may explain why they reported a higher rate of falls than in previous studies (72% vs. 50%–63% during the 6-month follow-up). This raises the possibility of differentially biasing the relationship between fear of falling and the outcome away from the null.
In conclusion, these findings support use of the 7-item version of the FES-I as a valid measure of fear of falling in people with MS and indicate that a higher score on the 7-item FES-I may be predictive of a higher risk of future recurrent falls, whether the individual has or has not fallen recurrently in the past.
PracticePoints.
The 7-item version of the Falls Efficacy Scale–International (FES-I) is a valid measure of fear of falling in people with MS.
Higher scores on the 7-item version of the FES-I are associated with a higher risk of future recurrent falls, whether the individual has or has not fallen recurrently in the past.
Footnotes
From Oregon Health & Science University, Portland, OR, USA (RM); Department of Public Health and Preventive Medicine, Oregon Health & Science University, Portland, OR, USA (WEL, TN); Department of Neurology, Oregon Health & Science University, Portland, OR, USA (DNB, MHC); and Portland Veteran Administration Medical Center, Portland, OR, USA (DNB, MHC).
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: Dr. Mazumder was supported by the Oregon Multidisciplinary Training Program in Health Services Research (grant T32 HS017582) from the Agency for Healthcare Research and Quality and by funding from the 2012 Foundation of the Consortium of Multiple Sclerosis Centers Workforce of the Future. Dr. Cameron was supported by a CDA-2 from the Department of Veterans Affairs Rehabilitation Research and Development Service. Secure data storage was supported by the Oregon Clinical and Translational Research Institute (grant 1 UL1 RR024140 01). This work was supported, in part, by a Canadian Institutes of Health Research Planning Grant (Funding Reference Number 129594).
References
- 1.Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. PM R. 2011;3:624–632. doi: 10.1016/j.pmrj.2011.04.015. quiz 632. [DOI] [PubMed] [Google Scholar]
- 2.Cattaneo D, De Nuzzo C, Fascia T, Macalli M, Pisoni I, Cardini R. Risks of falls in subjects with multiple sclerosis. Arch Phys Med Rehabil. 2002;83:864–867. doi: 10.1053/apmr.2002.32825. [DOI] [PubMed] [Google Scholar]
- 3.Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:1274–1279. doi: 10.1016/j.apmr.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Nilsagard Y, Lundholm C, Denison E, Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis: a longitudinal study. Clin Rehabil. 2009;23:259–269. doi: 10.1177/0269215508095087. [DOI] [PubMed] [Google Scholar]
- 5.Gunn H, Creanor S, Haas B, Marsden J, Freeman J. Frequency, characteristics and consequences of falls in multiple sclerosis: findings from a cohort study. Arch Phys Med Rehabil. 2014;95:538–545. doi: 10.1016/j.apmr.2013.08.244. [DOI] [PubMed] [Google Scholar]
- 6.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]
- 7.Mak MK, Pang MY. Parkinsonian single fallers versus recurrent fallers: different fall characteristics and clinical features. J Neurol. 2010;257:1543–1551. doi: 10.1007/s00415-010-5573-9. [DOI] [PubMed] [Google Scholar]
- 8.Gunn H, Creanor S, Haas B, Marsden J, Freeman J. Risk factors for falls in multiple sclerosis: an observational study. Mult Scler. 2013;19:1913–1922. doi: 10.1177/1352458513488233. [DOI] [PubMed] [Google Scholar]
- 9.Prosperini L, Fortuna D, Gianni C, Leonardi L, Pozzilli C. The diagnostic accuracy of static posturography in predicting accidental falls in people with multiple sclerosis. Neurorehabil Neural Repair. 2013;27:45–52. doi: 10.1177/1545968312445638. [DOI] [PubMed] [Google Scholar]
- 10.Kasser SL, Jacobs JV, Foley JT, Cardinal BJ, Maddalozzo GF. A prospective evaluation of balance, gait, and strength to predict falling in women with multiple sclerosis. Arch Phys Med Rehabil. 2011;92:1840–1846. doi: 10.1016/j.apmr.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther. 2013;93:504–513. doi: 10.2522/ptj.20120231. [DOI] [PubMed] [Google Scholar]
- 12.Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil. 2013;94:616–621. doi: 10.1016/j.apmr.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 13.Nilsagard Y, Carling A, Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int. 2012;2012:613925. doi: 10.1155/2012/613925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsuda PN, Shumway-Cook A, Ciol MA, Bombardier CH, Kartin DA. Understanding falls in multiple sclerosis: association of mobility status, concerns about falling, and accumulated impairments. Phys Ther. 2012;92:407–415. doi: 10.2522/ptj.20100380. [DOI] [PubMed] [Google Scholar]
- 15.Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler. 2007;13:1168–1175. doi: 10.1177/1352458507079260. [DOI] [PubMed] [Google Scholar]
- 16.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? a longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 17.Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age Ageing. 2005;34:614–619. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- 18.Kempen GI, Yardley L, van Haastregt JC et al. The short FES-I: a shortened version of the Falls Efficacy Scale-International to assess fear of falling. Age Ageing. 2008;37:45–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- 19.Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The Falls Efficacy Scale International (FES-I): a comprehensive longitudinal validation study. Age Ageing. 2010;39:210–216. doi: 10.1093/ageing/afp225. [DOI] [PubMed] [Google Scholar]
- 20.van Vliet R, Hoang P, Lord S, Gandevia S, Delbaere K. Falls Efficacy Scale-International: a cross-sectional validation in people with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:883–889. doi: 10.1016/j.apmr.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 21.Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- 22.Smith EV., Jr. Detecting and evaluating the impact of multidimensionality using item fit statistics and principal component analysis of residuals. J Appl Meas. 2002;3:205–231. [PubMed] [Google Scholar]
- 23.McDonald WI, Compston A, Edan G et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 24.Lublin FD, Reingold SC, National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis Defining the clinical course of multiple sclerosis: results of an international survey. Neurology. 1996;46:907–911. doi: 10.1212/wnl.46.4.907. [DOI] [PubMed] [Google Scholar]
- 25.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 26.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe and Outcomes Consensus Group Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 27.Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2001;3:CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 28.Raykov T, Marcoulides GA. Introduction to Psychometric Theory. New York, NY: Routledge; 2011. p. 335. [Google Scholar]
- 29.Brown M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 30.Cameron MH, Thielman E, Mazumder R, Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int. 2013;2013:496325. doi: 10.1155/2013/496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–P243. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 32.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994;49:M140–M147. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 33.Wijlhuizen GJ, Chorus AM, Hopman-Rock M. Fragility, fear of falling, physical activity and falls among older persons: some theoretical considerations to interpret mediation. Prev Med. 2008;46:612–614. doi: 10.1016/j.ypmed.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 34.Kalron A, Achiron A. Postural control, falls and fear of falling in people with multiple sclerosis without mobility aids. J Neurol Sci. 2013;335:186–190. doi: 10.1016/j.jns.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 35.Kasser SL, Jacobs JV, Littenberg B, Foley JT, Cardinal BJ, Maddalozzo GF. Exploring physical activity in women with multiple sclerosis: associations with fear of falling and underlying impairments. Am J Phys Med Rehabil. 2014;93:461–469. doi: 10.1097/PHM.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 36.Tinetti ME, Powell L. Fear of falling and low self-efficacy: a case of dependence in elderly persons. J Gerontol. 1993;48:35–38. doi: 10.1093/geronj/48.special_issue.35. Spec No. [DOI] [PubMed] [Google Scholar]


