Abstract
Background: Nonambulatory patients may be at risk for poor access to preventive health screening. Few studies have reported on this access in severely disabled women with multiple sclerosis (MS). We sought to describe preventive medical care in the most disabled women with MS and to identify factors that may influence access to care.
Methods: Patient records from the Partners MS Center database were reviewed. Women with Expanded Disability Status Scale scores of 7 or greater were selected. Proportions of patients with preventive-care visits were compared with 2012 Centers for Disease Control and Prevention (CDC) guidelines and normative data. Logistic regression was used to assess demographic and disease effects on receiving services.
Results: Forty-eight percent of patients had annual mammograms versus 72% of healthy women and the CDC target of 81%; 41.8% had Papanicolaou smears within 3 years compared with 82% of healthy women and the target of 93%; and 61.2% aged 50 years and older ever had a colonoscopy compared with the target of 70%. Younger age predicted lower rates of colonoscopy (P < .002) and mammography (P < .004), and shorter disease duration predicted lower rates of mammography (P < .004). Obesity was associated with a lower likelihood of colonoscopy (P = .007) and bone density screening (P = .02).
Conclusions: Women with severe MS disability are vulnerable to significantly decreased access to preventive care. The influence of patient and physician factors and the possible consequent delays in cancer diagnosis should be further clarified.
There is a need for preventive health-care services for all populations to avoid premature morbidity and mortality. Multiple sclerosis (MS) presents unique challenges to severely disabled women seeking necessary preventive care. Although the life span of women with MS is similar to that of age-matched healthy populations, MS may result in impaired mobility, cognitive difficulties, and mood disorders, all of which have the potential to negatively affect health-care access and outcomes. Previous studies have documented factors that adversely affect all physically disabled patients' access to care, including inadequate insurance coverage, lack of accessible offices, transportation challenges, and care providers who are not well informed about the unique needs of this population, especially when it comes to reproductive health.1,2 In addition, the immediate and life-threatening health-care needs of patients with severe physical disabilities often take up the bulk of the time and energy of health-care providers to the detriment of less acutely relevant preventive health-care services.1,3–6
These barriers to adequate care threaten the health of physically disabled individuals. Several studies7,8 have found significantly diminished use of Papanicolaou tests and mammography in women who have mobility impairments, even when controlling for demographic factors such as insurance coverage and consistent sources of care.8 However, access to general preventive services, such as blood pressure and cholesterol testing, did not depend on mobility status.7 This finding suggests that decreased preventive-care access among disabled women may not be solely due to lack of physician focus on such services but rather may involve factors of accessibility and physical limitations, such as placing legs in stirrups for cervical smear tests or the need to stand in a radiology suite for mammograms.2,7 Another study of breast and cervical cancer screening9 in disabled patients also strongly suggests that accessibility issues play a key role in decreased cervical cancer screening in women with disabilities.
Few studies have reported on access to preventive care in patients with MS with a focus on the most severely disabled women. Thus, we aimed to explore preventive-care access in women with an Expanded Disability Status Scale (EDSS) score of 7 or greater in one health-care system to determine how preventive-care screening access compared with that of the healthy population and current medical recommendations.
Methods
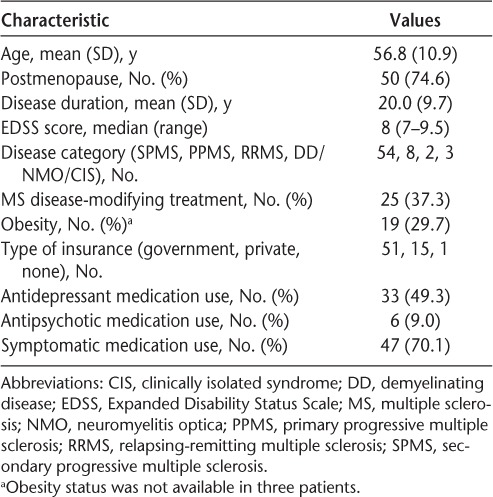
The study protocol was approved by the Brigham and Women's Hospital Institutional Review Board. Patient records from the Partners MS Center Oracle database were reviewed to identify women with EDSS scores of 7 or greater who had all their care delivered within Partners Health System. Sixty-seven patients who met these criteria were analyzed in the study. Extracted data from the electronic medical records included age, body-mass index (BMI), disease duration, EDSS score, clinical disease subtype, treatment for MS, history of hypertension, dates of annual primary-care physician (PCP) visits, and dates of screening mammography, Papanicolaou smear, colonoscopy, and bone density scans (Table 1). In the present patients, depression was ascertained by noting antidepressant drug use at the time of the most recent documented visit to either a PCP or a neurologist or noting antidepressant drug use at any time in conjunction with depression listed as a problem in the electronic medical record. Obesity was ascertained by a documented BMI of 30 or higher or specific mention of the patient's obesity by a PCP or neurologist in the medical record or obesity listed as a problem in the electronic medical record.
Table 1.
Demographic characteristics of the 67 study patients
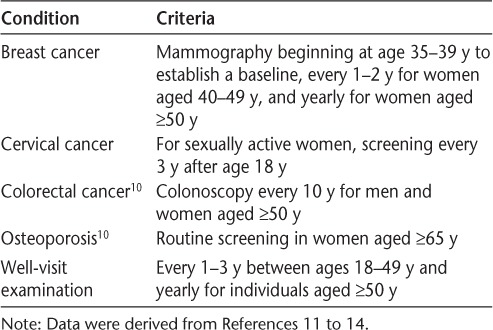
The health organization–recommended guidelines for breast cancer, cervical cancer, colorectal cancer, osteoporosis, and general wellness are provided in Table 2. For each of these conditions, the proportion of patients who met the recommended guideline was calculated. In addition, the exact binomial 95% confidence interval (CI) for the proportion was calculated, and this was compared with the health organization guidelines and healthy population data. Logistic regression was used to assess the effect of age, disease duration, EDSS score, depression, and obesity on the probability of meeting the recommended guideline.
Table 2.
Screening recommendations for breast cancer, cervical cancer, colorectal cancer, osteoporosis, and routine health visits with primary-care providers
Results
A total of 67 records were analyzed between November 1, 2011, and May 31, 2012; the demographic characteristics of the sample are provided in Table 1. The proportion of women with a mammogram during the previous year was 48% (95% CI, 35.4%–60.3%), and the proportion in women 50 years and older was 55.1% (95% CI, 40.2%–69.3%). This proportion is significantly lower than the proportion in healthy women (72%) and the Centers for Disease Control and Prevention (CDC) target rate (81%).15 The proportion of women with a Papanicolaou smear within 3 years was 41.8% (95% CI, 29.8%–54.5%). This is also significantly lower than the proportion in healthy women (82%) and the CDC target rate (93%).15 Of patients 50 years and older, 61.2% (95% CI, 46.2%–74.8%) had a colonoscopy, and this is not significantly different from the target of 70%.15 The proportion of women who ever had a screening bone density test was 68.6% (95% CI, 56.2%–79.4%), and 61.2% (95% CI, 48.5%–72.9%) had annual PCP visits. The proportions of women who had other screening tests are provided in Table 3.
Table 3.
Proportion of patients who had each screening procedure and univariate association between each screening procedure and potential predictors
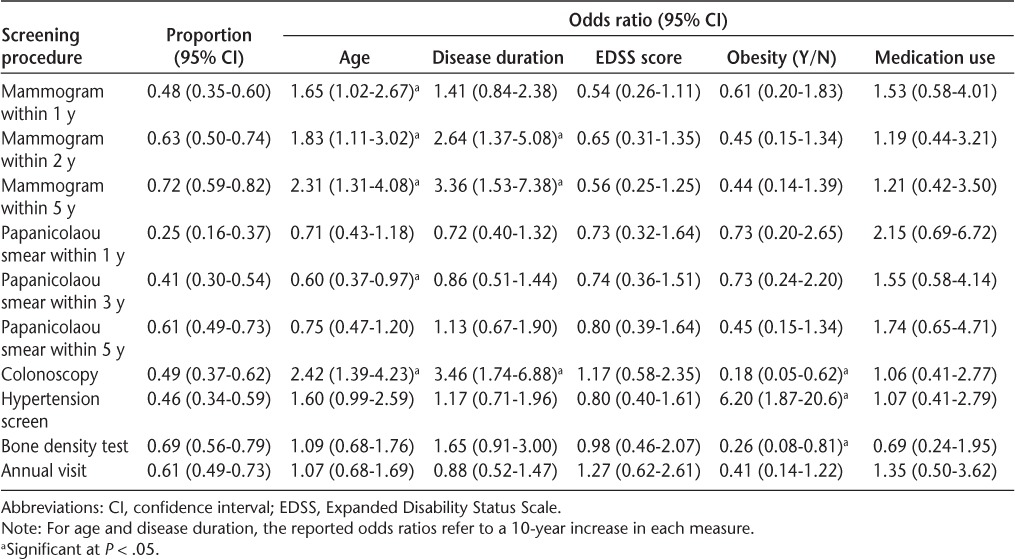
In addition, the demographic predictors of meeting the recommended criteria were investigated, and the results of univariate analyses are shown in Table 3. Younger age was associated with a lower likelihood that a patient had received colonoscopies (P = .002), a higher likelihood of Papanicolaou smears within the previous 3 years (P = .04), and a lower likelihood of mammography for all year cutoffs (P < .05 for each comparison). Restricting the analysis to individuals 50 years and older, younger age was no longer significantly associated with a decreased likelihood of getting a colonoscopy, but the direction of the associations remained (odds ratio [OR] = 1.45; 95% CI, 0.61–3.42; P = .40).
Shorter disease duration was associated with a lower likelihood of colonoscopies (P = .004) and mammograms within 2 or 5 years (P < .004 for each comparison). Obesity was associated with a lower likelihood of colonoscopies (P = .007) and bone density screening (P = .02) and a greater likelihood of hypertension screening (P = .003). Restricting the analysis to patients 50 years and older did not affect these associations, and the effect remained significant (disease duration: estimated OR = 2.60; 95% CI, 2.26–5.33; P = .01; obesity: estimated OR = 0.21; 95% CI, 0.05–0.85; P = .03).
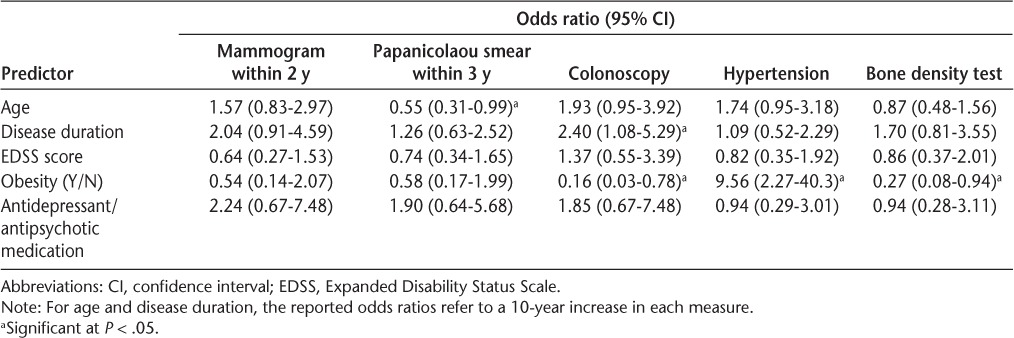
In a multivariate analysis (Table 4), obesity was also associated with a lower likelihood of colonoscopies (P = .02) and bone density screens (P = .04) and was linked to a higher likelihood of receiving hypertension screening (P = .002). In addition, increasing age was associated with a decreased chance of having a Papanicolaou smear, and increased disease duration was associated with an increased chance of having a colonoscopy. Finally, there was no significant association between annual PCP visits and the other screening tests.
Table 4.
Multivariate analysis for the odds ratio association with specific screening results
Discussion
Patients with MS have only a slightly shortened life expectancy relative to the general population.16 All-cause mortality for patients with MS includes complications of cardiovascular disease, malignancies, suicides, and causes directly attributable to MS, such as severe infections.17 Some studies suggest that women with MS, especially with the primary progressive type, may have a relative survival disadvantage compared with men with primary progressive MS.16
Women with advanced MS in this study were shown to have markedly decreased access to preventive health-care services, falling below CDC targets and below documented screening rates for age-matched healthy adults. Therefore, this group should be considered a vulnerable population for routine preventive health care. This is consistent with other literature identifying many barriers to preventive care among disabled women, most of which are based on challenges associated with accessibility.10,18 For example, a recent study looking at barriers and facilitators related to breast cancer screening in patients with MS reported that more than 80% of women who have not received annual mammograms had mobility impairment.19 These patients were also more likely to report additional barriers to screening, such as transportation issues, inaccessibility within the facility, difficulty with positioning in the mammogram machine, and barriers related to health-care providers, such as negative attitudes and a lack of referrals.
Restricting the analysis to patients 50 years and older, colonoscopy frequency was no longer affected by age. This might suggest that the observed association between younger age and lower colonoscopy frequency in a non–age-restricted cohort merely reflects the lack of recommendation for colonoscopy in younger individuals in the absence of specific risk factors.
We found no correlation between the frequency of PCP visits and screening tests, possibly suggesting that the breakdown in access to care occurs at a point of referral for screening tests by a provider. Alternatively, these results may indicate decreased patient compliance with referrals. Women with disabling MS are generally followed with certain frequency by a neurologist and a PCP. Other specialists, such as urologists, mental health workers, and physical and occupational therapists, may also be involved in the care of these patients. Enhancing collaboration among all health-care providers is important to ensure adherence to recommended screening practices. Furthermore, neurologists often serve as the primary contact for more disabled patients with MS and should also have basic awareness of the age-appropriate health maintenance and screening recommendations.
In contrast to some other studies,20,21 in the present sample, psychotropic medication use showed no association with the preventive care, indicating that the presence or absence of clinically significant psychiatric symptoms requiring treatment may not be an important variable affecting access to care in this patient population.
Obesity was a factor associated with a lower likelihood of colonoscopies and bone density tests and increased hypertension screens. In older healthy adults, BMI is known to have a significant inverse relationship with ambulatory measurements in terms of the distance walked, steps taken, and walking velocity.22 Colonoscopies and bone density scans require certain physical activity either in preparation for the testing (bowel-clearing regimen before colonoscopies) or during the procedure (positioning for bone density screening) and may have been disproportionately affected. Hypertension screening is usually performed in the office, with the patient sitting in a chair or in a wheelchair; thus, no additional physical activity beyond arriving for an appointment is required. It is also reassuring that obesity in a patient seems to prompt a health-care provider to perform hypertension screening with greater frequency.
Patients with MS generally have an increased risk of bone density loss due to recurrent exposure to corticosteroid therapies. Immobility is a further risk factor for osteoporosis.23 All of the present patients had severe mobility limitations, and 61.2% have been treated with either intermittent or long-term corticosteroids over the course of their disease. Therefore, we chose to report bone density screening frequency for all the patients regardless of age.
The present study did not include direct patient contact; therefore, we were not able to assess whether the availability of a caregiver or appropriate transportation to and from the medical testing or discomfort in positioning or preparations for the examinations, such as precolonoscopy bowel-cleansing regimens, may have been a factor in the overall decreased care. Furthermore, we did not specifically assess factors such as health-care provider attitudes and patient fear of a procedure or of a possible cancer diagnosis. We did not specifically consider disease-modifying therapies in this project, as more than 92% of the patients had progressive MS; patients receiving immunosuppressive or immunomodulating therapies were treated off label. However, medication use was not associated with the screening tests in a univariate analysis (Table 3). We did not address family history of malignancies, other personal cancer risk factors, or personal history of previous cancers in this study owing to the manner of medical record analysis. Moreover, we did not factor in race, socioeconomic status, educational level, or insurance type. In addition, this work would have been enhanced by comparing the group of patients with MS and severely limited mobility with a randomly selected group of individuals without identified chronic disability. All of these factors have been shown to affect health-care access, and the lack of these data is a limitation of this study.9
It is not known whether the decreased rates of preventive screening in severely disabled women with MS do, in fact, lead to poorer health outcomes, measurable in delayed cancer diagnoses that subsequently increase morbidity and mortality. A large recent Canadian study examined cancer risk and tumor size at diagnosis in a cohort of patients with MS compared with the general population.16 Overall cancer risk was lower in patients with MS than in the age-, sex-, and calendar year–matched general population, consistent with previously published studies, but the tumor size at cancer diagnosis was larger than expected in the cohort (P = .04), suggesting diagnostic neglect.16–18 This finding can have major implications for the well-being of patients with MS and may be explained by inadequate access to preventive screening tests.
This study is the first to collect medical record data on severely disabled women with MS from a single center and one health system. This method minimized the patient recall bias that can be a confounder in questionnaire-based studies and ensured data accuracy owing to no “out of network” referrals. However, these results may not be generalizable to a wider and more diverse patient population because they represent a homogeneous patient cohort attending an academic health center. We recognize that this is a limitation of this work. One additional pilot study has previously reported on preventive screening in people with MS. Health-care access was ascertained using patient-reported information through completion of surveys by patients in private and academic MS centers.10 It is reassuring that their observations were generally comparable with the present data.
Future research in this field should focus on larger studies of neurologically vulnerable populations from a variety of health-care systems. Further analyses with expanded patient samples may reveal which additional factors are relevant to care access in this population and whether certain centers have managed to improve screening access through targeted interventions that could be more broadly implemented.
PracticePoints.
Severely disabled women with MS have significantly decreased rates of mammography, Papanicolaou smears, and colonoscopies compared with healthy women and Centers for Disease Control and Prevention target rates.
These women may be at risk for delayed cancer diagnoses, and efforts should be made to improve access to preventive screening in this population.
Footnotes
From the University of California, San Diego, School of Medicine, La Jolla, CA, USA (KD); and Partners MS Center, Harvard Medical School, Boston, MA, USA (BH, MH).
Financial Disclosures: Dr. Houtchens has received research support from Teva Neurosciences, Biogen Idec, Genzyme Sanofi, Questcor, and Novartis. Dr. Healy receives research support from Merck Serono and Novartis. Ms. Dobos has no conflicts of interest to disclose.
Funding/Support: This study was partially funded by a research grant from the Multiple Sclerosis Foundation and by the Center for Neurological Diseases, Harvard Medical School.
References
- 1.Gans BM, Mann NR, Becker BE. Delivery of primary care to the physically challenged. Arch Phys Med Rehabil. 1993;74:15–19. [PubMed] [Google Scholar]
- 2.Becker H, Stuifbergen A, Tinkle M. Reproductive health care experiences of women with physical disabilities: a qualitative study. Arch Phys Med Rehabil. 1997;78(suppl 5):S26–S33. doi: 10.1016/s0003-9993(97)90218-5. [DOI] [PubMed] [Google Scholar]
- 3.Bockenek WL, Mann N, Lanig IS, DeJong G, Beatty LA. Primary care for persons with disabilities. In: DeLisa JA, Gans BM, editors. Rehabilitation Medicine: Principles and Practice. Philadelphia, PA: Lippincott-Raven; 1998. pp. 905–928. [Google Scholar]
- 4.Burns TJ, Batavia AI, Smith QW, DeJong G. Primary health care needs of persons with physical disabilities: what are the research and service priorities? Arch Phys Med Rehabil. 1990;71:138–143. [PubMed] [Google Scholar]
- 5.Stuifbergen AK, Becker H, Sands D. Barriers to health promotion for individuals with disabilities. Fam Community Health. 1990;13:11–22. [Google Scholar]
- 6.Stuifbergen AK, Becker HA, Ingalsbe K, Sands D. Perceptions of health among adults with disabilities. Health Values. 1990;14:18–26. [Google Scholar]
- 7.Cheng E, Myers L, Wolf S et al. Mobility impairments and use of preventive services in women with multiple sclerosis: observational study. BMJ. 2001;323:968–969. doi: 10.1136/bmj.323.7319.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. Am J Public Health. 2000;90:955–961. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nosek MA, Howland CA. Breast and cervical cancer screening among women with physical disabilities. Arch Phys Med Rehabil. 1997;78(suppl 5):S39–S44. doi: 10.1016/s0003-9993(97)90220-3. [DOI] [PubMed] [Google Scholar]
- 10.Barrett MW, Roberts B. Preventive screening in people with multiple sclerosis. Int J MS Care. 2010;12:168–176. [Google Scholar]
- 11.US Preventive Services Task Force, US Department of Health and Human Services. http://www.uspreventiveservicestaskforce.org/recommendations.htm. Accessed June 10, 2012.
- 12.Office on Women's Health, US Department of Health and Human Services. Womenshealth.gov website. http://www.womenshealth.gov. Accessed June 10, 2012.
- 13.Agency for Healthcare Research and Quality. Clinicians and providers. http://www.ahrq.gov/clinic. Accessed June 10, 2012. [DOI] [PubMed]
- 14.Mayo Clinic. Patient care and health information. http://www.mayoclinic.com/health-information. Accessed October 21, 2014.
- 15.Healthy People 2020. How to use DATA2020. http://www.healthypeople.gov/2020/data/default.aspx. Accessed June 10, 2012.
- 16.Kinwell E, van der Kop M, Zhao Y et al. Relative mortality and survival in multiple sclerosis: findings from British Columbia, Canada. J Neurol Neurosurg Psychiatry. 2012;83:61–66. doi: 10.1136/jnnp-2011-300616. [DOI] [PubMed] [Google Scholar]
- 17.Sadovnick AD, Eisen K, Ebers GC, Paty DW. Cause of death in patients attending multiple sclerosis clinics. Neurology. 1991;41:1193–1196. doi: 10.1212/wnl.41.8.1193. [DOI] [PubMed] [Google Scholar]
- 18.Tabares-Seisdedos R, Dumont N, Baudot A et al. No paradox, no progress: inverse cancer comorbidity in people with other complex diseases. Lancet Oncol. 2011;12:604–608. doi: 10.1016/S1470-2045(11)70041-9. [DOI] [PubMed] [Google Scholar]
- 19.Todd A, Stuifbergen A. Barriers and facilitators related to breast cancer screening: a qualitative study of women with multiple sclerosis. Int J MS Care. 2011;13:49–56. doi: 10.7224/1537-2073-13.2.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thorpe JM, Thorpe CT, Kennelty KA, Chewning BA. Depressive symptoms and reduced preventive care use in older adults: the mediating role of perceived access. Med Care. 2012;50:302–310. doi: 10.1097/MLR.0b013e31821a933f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care and health care access among women with disabilities in the 1994–1995 National Interview Survey, Supplement on Disability. Womens Health Issues. 2006;16:297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Yamakawa K, Tsai CK, Haig AJ, Miner JA, Harris MJ. Relationship between ambulation and obesity in older persons with and without low back pain. Int J Obes Relat Metab Disord. 2004;28:137–143. doi: 10.1038/sj.ijo.0802478. [DOI] [PubMed] [Google Scholar]
- 23.Picardo C, Luengo M. Corticosteroid-induced bone loss: prevention and management. Drug Saf. 1996;15:347–359. doi: 10.2165/00002018-199615050-00005. [DOI] [PubMed] [Google Scholar]


