Abstract
Introduction:
Social smoking is an increasingly common pattern among emerging adults. Although distinct patterns have emerged between social smokers and non-social smokers, there is discrepancy about how to define the construct, with inconsistencies between self-identified social smoking and behavioral social smoking. We report prevalence and correlates of young adult smokers who self-identify and behave as social smokers (SELF + BEH), self-identified non-behavioral social smokers (SELF-ONLY), and non-social smokers (NON-SOCIAL).
Methods:
Young adults age 18–25 years who have smoked at least 1 cigarette in the past 30 days (N = 1,811) were recruited through Facebook for a national anonymous, online survey of tobacco and other substance use. Three social smoking items were used to categorize respondents into 1 of 3 smoking groups. Groups were examined for prevalence and differences on demographics, substance use, motivation to quit smoking and thoughts about tobacco abstinence.
Results:
SELF-ONLY (46%) was the largest group, followed by SELF + BEH (27%) and NON-SOCIAL (27%). SELF + BEH smoke less frequently, smoke fewer cigarettes per day, are less addicted to cigarettes, have a higher desire to quit, and perceive a lower quitting difficulty compared with SELF-ONLY. SELF + BEH and SELF-ONLY were more likely to be male, be marijuana users, and be addicted to marijuana than NON-SOCIAL. SELF + BEH exhibited a lower frequency of smoking, less cigarettes per day, were less addicted, and had more days co-using alcohol and cigarettes than NON-SOCIAL.
Conclusion:
Identifying social smokers based on self-identification in addition to behavioral components appears to be important for designing smoking cessation interventions for emerging adults.
Introduction
Despite significant declines in regular smoking in the United States in the past 30 years to 18% in 2012,1 non-daily smoking continues to increase.2 It remains unclear whether non-daily smoking is a transitional stage between daily smoking and quitting, a transition towards heavier smoking, or if it a stage in which individuals might remain indefinitely.3 “Social smoking” is a pattern of smoking typically defined as smoking primarily in social contexts where others are smoking and is often characterized as a subtype of non-daily or light smoking. Given that emerging adulthood is a vulnerable period for smoking initiation4 and transition to heavier smoking,5 it is important to understand patterns of less heavy smoking, including social smoking, in this population that may be less susceptible to public health or cessation messages.
Non-daily smoking is an increasingly common pattern among emerging adults who may be initiating smoking6 and has been known to persist throughout young adulthood for some smokers.5 Social smokers tend not to smoke alone7–10 and restrict their use to social situations such as parties, bars, or nightclubs.8,9,11 Social smokers tend not to identify as “smokers” and report that they are not fearful of becoming addicted.12 Social smoking is common among emerging adults when smoking in groups is widely accepted, whereas smoking alone is seen as an unacceptable behavior indicative of a need for a cigarette.12
Social smokers may fail to recognize the health risks associated with their tobacco use,8,9 making intervention with this group a particular challenge. Although the health consequences of social smoking have not been specifically studied, non-daily smokers suffer from significant smoking-related morbidity and mortality compared with never-smokers13,14 and light smoking (<10 cigarettes/day) is associated with cardiovascular risk comparable with daily smoking.15,16 Thus, promoting cessation among intermittent smokers, including social smokers, is critical.
The social smoking literature has been complicated by inconsistent operationalization of social smoking. Social smoking has been defined as follows: (a) smoking that is non-daily and predominantly takes place in bars, restaurants, and nightclubs17—this definition focuses on the location in which the smoking occurs, rather than who the individual is smoking with or how they view themselves; (b) smoking that is non-daily but only occurs when other smokers are present7—this definition expands upon the social component by including with whom an individual smokes, but fails to include how the individual views themselves; (c) smoking most commonly while partying or socializing18—this definition fails to include information on whether others are smoking or self-identification as a social smoker; or (d) self-identification as a social smoker8,19—this definition does not include information on actual social smoking behaviors. These definitions can vary widely in smoking patterns included in each (e.g., a self-identified social smoker could also be a daily smoker while some exclude daily smokers), with implications for understanding patterns of social smoking and cessation efforts with this population. A main distinguishing factor among definitions used is whether social smoking is only a behavioral concept, whether it is only a self-identified concept, or some combination of the two.
Defined behaviorally, social smoking has been associated with lower intensity and frequency of cigarette use, less dependence, lower intentions to quit, and fewer past year 24-hr quit attempts than regular smoking.9 Social smokers also spent more time socializing with friends, were binge drinkers, valued the arts, and were more likely to be African American than non-Hispanic White.9 Social smoking may also relate to use of other substances such as alcohol and marijuana differently than other smoking patterns. Social smoking has consistently been correlated with alcohol use, given that it often takes place in the context of drinking.10 In addition, non-daily smoking is associated with binge drinking, particularly on U.S. college campuses20. Social smokers have been found to desire smoking more when drinking compared with non-social smokers8 and are more likely to be binge drinkers.9 A review21 of light and intermittent smoking indicated that the light/intermittent smoking pattern is more driven by alcohol use than daily/heavy smoking. The National Epidemiological Survey on Alcohol and Related Conditions found that hazardous drinking was 3 times more likely for daily smokers, but 5 times more likely for non-daily smokers compared with non-smokers.22 There is also some evidence that alcohol increases risk for cigarette craving,23,24 and tobacco companies have actively co-marketed with alcohol companies.25
There is a lack of data on the relationship between social smoking and marijuana use; however, strong relationships exist between tobacco and marijuana in adolescents and young adults.26 Recent findings suggest that marijuana use among non-smokers increases future vulnerability to tobacco dependence.27,28 Given the common patterns of tobacco and marijuana use and social context in which these substance are often used among emerging adults,12,29 there is a need to examine whether marijuana use is heavier among social smokers than non-social smokers and whether this varies by definition of social smoking.
Definitions of social smoking may also impact smoking cessation intention and behavior. Song and Ling30 found that young adults who met a behavioral definition of social smoking (smoke mainly or only with others) were more likely than those who self-identified as social smokers to have cessation intentions and previous cessation attempts. Consistent with the behavioral definition of social smoking, intermittent and non-daily smokers appear to have greater intentions to quit than regular smokers.3,18,21 Social smoking (characterized as smoking while partying or socializing) was not found to be related to motivation to quit, but was related to higher confidence to quit compared with more regular smoking.18 There are some key differences between social smoking defined behaviorally and that defined through self-identification. A greater understanding of differences between those young people who identify as social smokers and also behave as such (smoking mainly or only with others) and those who only identify as social smokers but may smoke alone sometimes will help to guide the definitions researchers use and aid in cessation attempts with these groups.
This study used data from a national sample of young adult recent smokers recruited online to examine patterns and correlates of social smoking. Specifically, we aimed to (a) identify primary patterns of social smoking among young adults by examining prevalence of self-identified and behavioral social smokers (SELF + BEH), self-identified non-behavioral social smokers (SELF-ONLY), and non-social smokers (NON-SOCIAL); (b) examine differences in demographic, substance use, and smoking-related correlates between self-identified social smokers who also behave that way (SELF + BEH) and those who self-identify but do not behave (SELF-ONLY). We hypothesized that SELF + BEH would look more like non-daily smokers in patterns of smoking and intentions to quit than SELF-ONLY. Specifically, SELF + BEH were expected to smoke fewer cigarettes and less often, have a longer time to first cigarette upon waking, be less likely to have made a recent quit attempt, be less motivated to quit, have lower desire to quit, and be less likely to endorse a goal of abstinence than SELF-ONLY. In contrast, given a connection between social smoking identity and substance use in social contexts, the groups were expected to have few differences on alcohol or marijuana use. (c) Examine differences in demographic, substance use, and smoking-related correlates between social smokers (SELF + BEH and SELF-ONLY) and NON-SOCIAL.
Materials and Methods
Participants and Procedure
Data were taken from an anonymous, national cross-sectional survey convenience sample of young adult smokers. Recruitment and survey design are described in more detail elsewhere.31 Between April 2009 and December 2010, emerging adults aged 18–25 who had smoked at least one cigarette in the past month were recruited online using a paid advertisement campaign through Facebook described previously.32 Briefly, 20 advertisements were run through Facebook’s Ads Manager program >13 months. Ads targeted Facebook users in our target age-range (18–25) and location (United States), with some targeting using tobacco- or marijuana-related keywords. All ads were approved by Facebook according to the company’s guidelines at the time of recruitment.33 Possible participants completed a consent form (approved by the University’s Institutional Review Board), were screened for eligibility, and were sent to a secure online survey (encrypted for additional security) lasting ~20min. IP addresses from computers were tracked so that only one entry from each computer was allowed (to avoid multiple entries from the same individual); however, multiple records were allowed from the same Internet connection (e.g., dormitories, apartment buildings). Eligibility checks for age and smoking were embedded throughout the survey for additional evaluation and respondent with inconsistent data were not used in the present analysis. All eligible respondents who completed the survey were entered into a drawing for a prize of U.S. $25 or $400. At least 6,532 clicks were made to the survey’s first page from one of the study’s advertisements; 3,457 were eligible participants, while 3,075 were excluded for various reasons (did not sign consent [n = 212]; did not complete eligibility screen [n = 1,444]; did not meet inclusion criteria on an eligibility screener [n = 982]; provided clearly invalid data [e.g., data were inconsistent across multiple measures of age or smoking, indicating inclusion criteria were not met; multiple entries were made from the same computer IP address in short succession with early entries not meeting criteria and later entries meeting criteria; n = 437]). Of the n =3,457 eligible, valid cases, n = 1,646 did not complete smoking measures needed for the present analysis (either social smoking or quantity/frequency of smoking), leaving N =1,811 valid, completed surveys (used in this analysis). The final response rate for the survey was 52%, consistent with other online surveys of substance abuse.34
Measures
Social Smoking
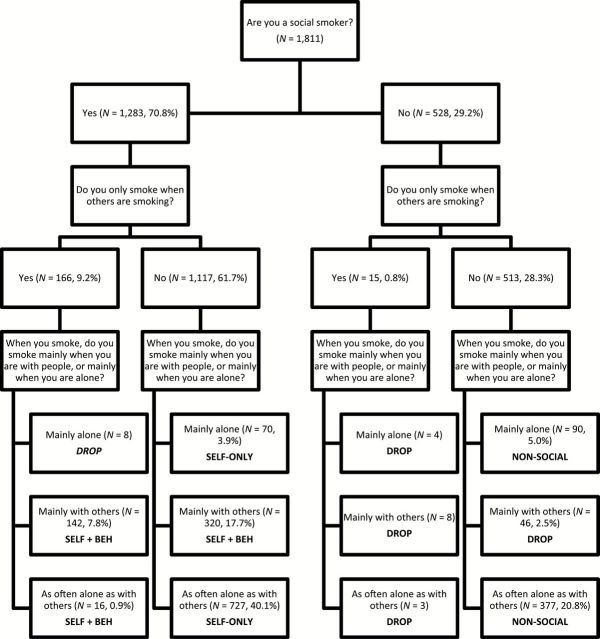
Social smoking was examined using three questions: “Are you a social smoker?” (yes, no; self-identification), “Do you ONLY smoke when others are smoking?” (yes, no; strict behavioral definition), and “When you smoke, do you smoke mainly when you are with people, or mainly when you are alone?” (mainly alone, mainly with others, or as often alone as with others; lenient behavioral definition, more likely to capture non-daily smokers).30 Three mutually exclusive categories of social smoker were created using these questions: (a) Those who self-identified as social smokers and behave accordingly (SELF + BEH); (b) Self-identified, but not behavioral social smokers (SELF-ONLY); and (c) Those who did not self-identify as social smokers, and also did not exhibit social smoking behaviors, not social smokers (NON-SOCIAL). Cases with conflicting responses (e.g., no to social smoker, but said smoke only when others are smoking; n = 69, 3.8%) were also dropped. Figure 1 describes how each group was categorized. When responses did not match up exactly, a judgment call was made by all three authors based on our definitions. For example, those who responded “no” to “Do you smoke only when others are smoking” but responded “mainly with others” to “When you do smoke do you smoke mainly when you are with people, or mainly when you are alone?” were categorized as SELF-BEH, as they mostly smoked with others even if it was not all the time.
Figure 1.
Flowchart of social smoking categories. Percentages were calculated based on the full sample (N = 1,811).
Demographics
Gender, age, race/ethnicity (White, African American, Asian/Pacific Islander, Hispanic/Latino, Other/Multiple), and household income ($21,000–$60,000; $61,000–$100,000; >$100,000) were assessed.
Tobacco and Other Substance Use
A smoking questionnaire examined age at first cigarette, frequency of smoking (days/week), average cigarettes per day, time to first cigarette after waking in the morning (> or <30min), and presence of at least one past year quit attempt of 3 days or longer.35 Timeline Followback procedures36,37 assessed past 30-day alcohol and marijuana use, percent of days co-using cigarettes and marijuana, percent of days co-using cigarettes and alcohol, and past 30-day heavy drinking days. Alcohol and marijuana use were dichotomized due to the high percentage of non-users that likely indicated two separate populations. Marijuana-dependence symptoms were assessed initially with the Cannabis Use Disorder Identification Test (CUDIT)38 and then switched after 8 months of recruitment (n = 297) to the recommended Cannabis Use Disorder Identification Test-Revised (CUDIT-R).38 As scale total scores were slightly different for the two measures, CUDIT and CUDIT-R scores were converted to Z-scores and pooled.
Motivation to Quit Smoking and Thoughts About Abstinence
Stage of change for smoking was assessed using the Smoking Stages of Change Questionnaire.39 This allows the categorization of smokers into three pre-action stages of change: Pre-contemplation (i.e., no intention to quit within the next 6 months), Contemplation (i.e., intention to quit within the next 6 months but no 24-hr quit attempt in the past year), and Preparation (i.e., intention to quit within the next month and a 24-hr quit attempt in the past year). Thoughts about abstinence35 were assessed using 3 single-item questions scored on a scale from 1 to 10. Abstinence goal was assessed (0 = non-abstinence, 1 = abstinence).
Statistical Analyses
First, complete surveys were compared with incomplete surveys (e.g., did not complete smoking questionnaire) on demographics characteristics. Demographic measures were chosen based on previous research.9
Second, prevalence was examined for each social smoking definition, and differences were examined on demographic, smoking, and substance use variables using t-tests for continuous variables and chi-square tests for categorical variables. Variables examined included gender, age, household income, ethnicity, age at first cigarette, frequency of smoking, cigarettes per day, time to first cigarette upon waking, past year quit attempt, past month alcohol use (yes/no), past month marijuana use (yes/no), percent days co-using cigarettes and marijuana in the past month, percent days co-using cigarettes and alcohol in the past month, CUDIT, number of past 30-day heavy drinking days, stage of change, abstinence goal, and thoughts about tobacco abstinence.
Third, multivariate logistic regression was used to examine associations between demographic, substance use, motivation to quit, and thoughts about abstinence variables and definitions of social smoking. Predictors included all significant predictors from bivariate analyses. The dependent variable was social smoking (SELF + BEH vs. SELF-ONLY) to distinguish how self-identified social smokers who behave consistency differed from those who do not behave consistently.
Fourth, two additional regressions were modeled in the same fashion as described previously, comparing SELF + BEH to NON-SOCIAL and SELF-ONLY to NON-SOCIAL). All analyses were performed using SAS 9.2.40
Results
Comparison of Completers and Non-Completers
Those who completed the survey (N = 1,811) were more likely to be White (73.6% vs. 71.3%, p < .05), male (64.2% vs. 70.1%, p < .0001) and were older (M = 20.5, SD = 2.0 vs. M = 20.0, SD = 1.8, %, p < .0001) than those who reported demographic data but did not complete the survey (N = 1,646). The groups did not differ in terms of income, region, parents’ highest education, and participant years of education. All variables that differed by group were included in analyses of smoking group differences.
Social Smoking Categories
The majority of the sample self-identified as social smokers but did not follow the behavioral definition (SELF-ONLY; n = 797, 45.8%), followed by SELF + BEH (n = 478, 27.4%), and NON-SOCIAL (n = 467, 26.8%), Table 1.
Table 1.
Demographic Characteristics and Pairwise Comparisons
| Self-identified and behavioral | Self-identified and not behavioral | Not social smokers | ||
|---|---|---|---|---|
| Overall | (N = 478, 27.4%) | (N = 797, 45.8%) | (N = 467, 26.8%) | |
| Male (%) | 64.19 | 65.13a | 67.46a | 57.88b |
| Age (M, SD) | 20.50, 2.05 | 20.31, 1.92a | 20.45, 2.02ab | 20.67, 2.14b |
| Household income | ||||
| <$20,000 | 26.95 | 23.43 | 27.60 | 29.12 |
| $21,000–$60,000 | 36.28 | 34.10 | 35.51 | 40.26 |
| $61,000–$100,000 | 19.27 | 21.76 | 20.45 | 14.78 |
| >$100,000 | 17.5 | 20.71a | 16.44ab | 15.85b |
| Ethnicity | ||||
| African American | 2.98 | 3.35 | 2.51 | 3.00 |
| Asian, Pacific Islander | 3.64 | 3.14 | 4.02 | 3.21 |
| White | 71.34 | 70.71 | 70.64 | 74.09 |
| Hispanic | 6.29 | 7.53 | 6.15 | 5.14 |
| Other/Multiple | 15.74 | 15.27a | 16.69a | 14.56a |
| Age at first cigarette (M, SD) | 14.47, 3.06 | 15.07, 2.90a | 14.32, 3.15b | 14.05, 2.99b |
| Frequency of smoking (days/week) (M, SD) | 5.82, 2.16 | 4.47, 2.58a | 6.34, 1.59b | 6.39, 1.58b |
| Cigarettes per day (M, SD) | 8.87, 7.60 | 4.31, 5.09a | 10.22, 7.94b | 11.50, 7.23c |
| Time to first cigarette (% cigarette <30min) | 36.33 | 13.18a | 42.16b | 50.32c |
| Past year quit attempt (% yes) | 61.73 | 68.49a | 62.48b | 53.00c |
| TLFB alcohol user (%) | 78.08 | 85.98a | 77.42b | 72.38c |
| TLFB marijuana user (%) | 54.67 | 60.46a | 56.34a | 45.82b |
| Percent days co-using cigarettes and marijuana (M, SD) | 27.07, 36.76 | 23.93, 33.41a | 29.98, 37.75b | 25.79, 38.23ab |
| Percent days co-using cigarettes and alcohol (M, SD) | 22.59, 26.94 | 27.21, 27.23a | 21.88, 26.50b | 19.28, 26.57b |
| CuditZ (M, SD) | 0.02, 0.77 | 0.01, 0.71ab | 0.07, 0.82a | -0.06, 0.75b |
| 30-Day heavy drinking days (M, SD) | 2.86, 4.62 | 3.22, 4.44a | 3.02, 4.90a | 2.24, 4.25b |
| Stage of change (%) | ||||
| Pre-contemplation | 47.79 | 45.49 | 46.55 | 52.03 |
| Contemplation | 30.17 | 25.37 | 32.25 | 31.69 |
| Preparation | 22.04 | 29.14a | 21.20b | 16.27b |
| Abstinence goal (% with abstinence goal) | 10.44 | 10.46ab | 8.78a | 12.42b |
| Desire to quit (M, SD) | 5.26, 3.03 | 5.71, 2.98a | 5.14, 2.99b | 4.93, 3.09b |
| Self-efficacy (M, SD) | 5.90, 2.89 | 7.00, 2.67a | 5.57, 2.82b | 5.26. 2.89b |
| Difficulty (M, SD) | 6.53, 2.82 | 5.38, 2.86a | 6.69, 2.62b | 6.98, 2.78b |
Note. CUDIT = Cannabis Use Disorder Identification Test; TLFB = timeline followback.
Difference within each social smoking category using t-tests or chi-squares. Categories that share superscripts refer to comparisons that are not statistically different. Categories that do not share subscripts refer to statistically significant difference, p < .05. For all hypotheses tests, the alpha was set to 0.05.
Demographics, Substance Use, Motivation to Quit, and Thoughts About Abstinence by Definition of Social Smoking
Overall, the sample was predominantly male (64%), White (71%), smoked 5.8 days a week (SD = 3.1), and 8.9 cigarettes/day (SD = 7.6) on average, over three quarters consumed alcohol and more than half (55%) used marijuana in the past month (Table 1).
Differences were found by definition (Table 1). Compared with SELF-ONLY and NON-SOCIAL, SELF + BEH were older when having first cigarette, smoked fewer days per week, spent more days co-using cigarettes and alcohol, were more ready to quit smoking, and had higher desire to quit, higher self-efficacy for quitting, and lower perceived quitting difficulty. SELF-BEH smoked the most cigarettes per day on average, had the lowest percent smoking within 30min of waking, highest percent with a past year quit attempt, and highest percent with past month alcohol use of all three groups, followed by SELF-ONLY and NON-SOCIAL. Compared with NON-SOCIAL, SELF + BEH was slightly younger and had higher income. Compared with SELF-ONLY, SELF + BEH had a lower percentage of days co-using cigarettes and marijuana. Compared with NON-SOCIAL, SELF-ONLY had more marijuana-dependence symptoms (CUDIT total score) and fewer members of this group had a smoking abstinence goal. Compared with the other two groups, NON-SOCIAL had fewer past month heavy drinking days. No differences were found between groups on ethnicity.
Multivariate Regression Comparing SELF + BEH and SELF-ONLY
Compared with SELF-ONLY, SELF+BEH had lower frequency of smoking, smoked fewer cigarettes per day, had a longer time to first cigarette, higher desire to quit, and lower difficulty in remaining quit (Table 2).
Table 2.
Multivariate Association Between Predictors Assessed and Type of Social Smoker
| Predictors | SELF + BEH vs. SELF-ONLY (REF) | ||
|---|---|---|---|
| Odds ratio | 95% Confidence interval | p | |
| Male | 0.94 | 0.70, 1.25 | .651 |
| Age | 0.97 | 0.91, 1.04 | .451 |
| Income (ref: >$100,000) | |||
| <$20,000 | 0.94 | 0.62, 1.41 | .756 |
| $21,000–$60,000 | 0.89 | 0.61, 1.23 | .541 |
| $61,000–$100,000 | 0.91 | 0.60, 1.38 | .656 |
| Age at first cigarette | 1.02 | 0.99, 1.06 | .494 |
| Frequency of smoking | 0.82 | 0.76, 0.89 | <.0001 |
| Cigarettes per day | 0.48 | 0.90, 0.95 | <.0001 |
| Time to first cigarette (ref: cigarette <30min) | 0.54 | 0.38, 0.78 | .001 |
| Past year quit attempt | 1.25 | 0.98, 1.72 | .170 |
| TLFB alcohol user | 1.01 | 0.68, 1.50 | .965 |
| TLFB marijuana user | 1.05 | 0.73, 1.53 | .786 |
| Percent days co-using cigarettes and marijuana | 0.99 | 0.99, 1.00 | .417 |
| Percent days co-using cigarettes and alcohol | 1.01 | 1.00, 1.01 | .126 |
| CuditZ | 0.97 | 0.81, 1.16 | .748 |
| 30-Day heavy drinking days | 1.02 | 0.99, 1.05 | .315 |
| Stage of change (ref: preparation) | |||
| Pre-contemplation | 1.22 | 0.75, 2.00 | .439 |
| Contemplation | 1.02 | 0.68, 1.49 | .929 |
| Abstinence goal (ref: goal) | 1.51 | 0.94, 2.43 | .089 |
| Desire to quit | 1.07 | 1.01, 1.15 | .048 |
| Self-efficacy | 1.03 | 1.03, 1.08 | .375 |
| Difficulty | 0.91 | 0.85, 0.95 | .001 |
Note. CUDIT = Cannabis Use Disorder Identification Test; TLFB = timeline followback.
Categories that share superscripts refer to comparisons that are not statistically different. Categories that do not share subscripts refer to statistically significant difference.
Multivariate Regression Comparing SELF + BEH and SELF-ONLY to NON-SOCIAL
In the model comparing SELF + BEH to NON-SOCIAL, SELF + BEH were more likely to be male, had lower frequency of smoking, smoked fewer cigarettes per day, had longer time to first cigarette, were more likely to be marijuana users, had a higher percentage of days co-using cigarettes and alcohol, and were more likely to be addicted to marijuana. In the model comparing SELF-ONLY to NON-SOCIAL, SELF-ONLY were more likely to be male, had a higher income, more likely to have a past year quit attempt, more likely to be marijuana users, had higher CUDIT scores, had more heavy drinking days, and were more likely to have an abstinence goal (Table 3).
Table 3.
Multivariate Association Between Predictors Assessed and Type of Smoker (Social vs. Non-social)
| SELF + BEH vs. NON-SOCIAL (ref) | SELF-ONLY vs. NON-SOCIAL (ref) | |||||
|---|---|---|---|---|---|---|
| Predictors | Odds ratio | 95% Confidence interval | p | Odds ratio | 95% Confidence interval | p |
| Male | 1.01 | 0.72,1.14 | .98 | 1.39 | 1.09, 1.79 | .01 |
| Age | 0.98 | 0.75,1.06 | .61 | 0.98 | 0.97, 1.04 | .45 |
| Income (ref: >$100,000) | ||||||
| <$20,000 | 0.88 | 0.52, 1.32 | .61 | 0.88 | 0.60, 1.29 | .52 |
| $21,000–$60,000 | 0.83 | 0.52, 1.32 | .44 | 0.99 | 0.70, 1.41 | .93 |
| $61,000–$100,000 | 0.60 | 0.35, 1.01 | .06 | 0.66 | 0.43, 0.99 | .05 |
| Age at first cigarette | 1.02 | 0.95, 1.07 | .66 | 1.01 | 0.97, 1.05 | .67 |
| Frequency of smoking | 0.88 | 0.86, 0.99 | .03 | 1.04 | 0.95, 1.13 | .42 |
| Cigarettes per day | 0.89 | 0.86, 0.92 | <.0001 | 0.98 | 0.96, 1.01 | .06 |
| Time to first cigarette (ref: cigarette <30min) | 0.47 | 0.31, 0.71 | .00 | 0.82 | 0.62, 1.08 | .16 |
| Past year quit attempt | 1.37 | 0.93, 1.99 | .11 | 1.31 | 0.99, 1.72 | .05 |
| TLFB alcohol user | 1.15 | 0.73, 1.80 | .55 | 1.03 | 0.75, 1.41 | .85 |
| TLFB marijuana user | 1.80 | 1.14, 2.82 | .01 | 1.54 | 1.08, 2.20 | .01 |
| Percent days co-using cigarettes and marijuana | 1.00 | 1.00, 1.01 | .27 | 1.00 | 1.00, 1.01 | .42 |
| Percent days co-using cigarettes and alcohol | 1.01 | 1.00, 1.01 | .05 | 1.00 | 1.00, 1.01 | .55 |
| CuditZ | 1.25 | 0.611.00 | .05 | 1.23 | 1.05, 1.42 | .01 |
| 30-Day heavy drinking days | 1.03 | 0.09, 0.99 | .13 | 1.04 | 1.01, 1.07 | .04 |
| Stage of change (ref: preparation) | ||||||
| Pre-contemplation | 0.74 | 0.40, 1.35 | .31 | 0.66 | 0.44, 1.07 | .09 |
| Contemplation | 0.86 | 0.52, 1.41 | .54 | 0.83 | 0.55, 1.22 | .33 |
| Abstinence goal (ref: goal) | 1.11 | 0.66, 1.85 | .70 | 1.58 | 1.05, 2.43 | .02 |
| Desire to quit | 1.04 | 0.95, 1.12 | .39 | 0.98 | 0.97, 1.08 | .42 |
| Self-efficacy | 1.04 | 0.97, 1.11 | .25 | 1.02 | 7, 1.08 | .38 |
| Difficulty | 0.94 | 0.88, 1.01, | .11 | 1.02 | 0.96, 1.06 | .55 |
Note. CUDIT = Cannabis Use Disorder Identification Test; TLFB = timeline followback.
Categories that share superscripts refer to comparisons that are not statistically different.
Discussion
We compared two definitions of social smoking to one another and then each to non-social smoking. We found notable inconsistencies between identity as a social smoker and reports of behaving as a social smoker (smoking only or primarily when others are present). At close to half the sample, the most prevalent group was made up of young adults who self-identify as social smokers but do not behave as social smokers (by smoking mainly or only with others, SELF-ONLY), with about a quarter (27%) of young adult cigarette smokers both identifying and behaving as social smokers (SELF + BEH), and another quarter (27%) not identifying as social smokers. The large discrepancy in prevalence and numerous differences in smoking and other substance use found here between definitions of social smoking suggest researchers should incorporate measures of both identity and behavior constructs in studies of social smoking. Further, using two items to assess behavioral social smoking (i.e., smoking “mainly” and “only” with others) appears to fully capture the range of behavioral patterns of social smoking among young adults.
Consistent with our hypotheses, SELF + BEH were lighter smokers (lower frequency of smoking, fewer cigarettes per day, less dependence) and had a lower perceived difficulty with quitting smoking than SELF-ONLY. SELF + BEH is a measure that is more consistent with social smoking defined as a subset of light or intermittent smoking, whereas SELF-ONLY do not appear to necessarily be “light” smokers. However, we did not find differences in number of recent quit attempts, motivation to quit, or abstinence goals for SELF + BEH compared with SELF-ONLY, suggesting that efforts to increase motivation for quitting should be strong for all those who identify as social smokers, not just those who smoke mainly with others.
Although SELF + BEH smoke less frequently and fewer cigarettes per day than NON-SOCIAL, their quitting behaviors did not differ from non-social smokers. Classic cessation messages that are directed at smokers might not resonate to social smokers if they do not believe they are “real” smokers. However, if smoking patterns are consistent with non-social smokers, health risks of smoking are still high. SELF + BEH may be more ready to quit than SELF-ONLY, given greater likelihood of past year quit attempts and goals of complete abstinence. Intervention programming targeted to social smokers through language and assessment would likely work best with this more motivated group. Identification as a “social smoker” may also act as a transitional step between being a daily smoker and quitting entirely7 further indicating that this group would be receptive to target cessation efforts. Perhaps, assessing previous daily smoking status (e.g., “Have you ever been a daily smoker?”) would add value to this line of research.
Differences were also found when the two types of self-identified social smokers were compared with non-social smokers. Both social smoking groups were more likely to be male, marijuana users, and had more marijuana-dependence symptoms than NON-SOCIAL. Marijuana use during emerging adulthood is often a social phenomenon,41 and co-use may be a function of identity at this age, rather than related to behavioral phenomena. All those who identified as social smokers should be screened for marijuana use and co-use considered into a plan for smoking cessation.
Correlations between social smoking and alcohol use have been found consistently in the research,10 likely because social smoking often occurs during social drinking occasions. Consistent with this, we found that SELF + BEH had a higher percentage of days co-using cigarettes and alcohol than NON-SOCIAL and that SELF-ONLY had more heavy drinking days than NON-SOCIAL. There is some evidence that social smokers (both behaviorally and not) are more likely than non-social smokers to consume alcohol. This finding is supported both because it appears that cigarette craving increases with alcohol use23,24 and because social smoking often occurs during social occasions which in young people, often include alcohol.10
Social smoking motivations likely vary greatly across smokers, but social smokers may believe that by limiting smoking to social environments they are preventing addiction and/or the negative health consequences of smoking. Social smokers may also be less inclined to report smoking for reasons such as stress reduction, the feeling of the actual smoke, or because of the addiction as most regular smokers state as primary reasons. Better defining the motivations that underlie social smoking and using this information in future cessation programming is critical.
Limitations
The sample used was a convenience sample and thus the results are not nationally generalizable. Numerous statistical tests were performed without any alpha correction; as such Type I error might be a concern. Self-report data can also be a concern, but previous studies found good reliability and validity for both tobacco and marijuana reports.26,42 In addition, only 52% of the entire eligible sample completed the survey. However, this completion rate is consistent with other online smoking studies,43–45 and methods of tracking participants beyond what were employed here would have compromised a goal of the research to maintain participant anonymity. Online strategies for survey recruitment (including social media) can reach large, diverse, hard-to-reach groups32; however, Internet surveys often draw interest among those outside inclusion criteria and drop-off tends to be high. In addition, representativeness is often impossible to determine with online recruitment. In this study, our sample was 64% male and 71% White, consistent with 2010 census data (75% White),46 and national data from the Pew Internet and American Life Project showing that 62% of Facebook users were male in 2012.47 Although promising, representativeness of smoking young adults is not possible to discern from these data. Finally, overall, the effect sizes were small so the results should be interpreted with caution.
Conclusion
The majority of the emerging adult sample identified themselves as social smokers, but the largest majority did not fit the behavioral definition of social smoking. The striking percentage of self-identified social smokers found here suggests that self-identification as a social smoker will classify the broadest group of individuals as social smokers. It appears that self-identified social smokers as a group are more likely to be male, marijuana users, addicted to marijuana, and might be more at risk for alcohol-related problems. As such, this might be a group that needs to be targeted for anti-marijuana and alcohol efforts to prevent addiction. SELF + BEH exhibit behaviors consistent with the definition, as they smoke less frequently, smoke fewer cigarettes per day, and are less addicted; however, they do not seem to differ on quitting behaviors and ease of quitting compared with NON-SOCIAL. Although we hypothesized that SELF-ONLY might be way that young people avoid thinking about themselves as smokers, and that they might be less likely to want or need to quit, we did not find this relationship. Young adult social smokers, both self-identified and behavioral, might be prime candidates for selective smoking interventions. Future studies might look at how recruitment source (e.g., Facebook) predicts social smoking and how those who fit into more than one social smoking category differ from those who fall into one single category.
Funding
This study was supported by an institutional training grant (T32 DA007250; PI, J. Sorensen), a center grant from the National Institute on Drug Abuse (NIDA; P50 DA09253; PI, J. Guydish), and an individual Postdoctoral Fellowship Award from the California Tobacco-Related Diseases Research Program (TRDRP; 18FT-0055; PI, D. Ramo). The preparation of this manuscript was supported in part by NIDA (K23 DA032578; PI, D. Ramo) and the National Cancer Institute (U01-154240; PI, P. Ling)
Declaration of Interests
None declared.
Acknowledgments
We acknowledge Judith J. Prochaska, PhD, MPH, for comments on an earlier draft of this manuscript.
References
- 1. Agaku IT, King BA, Dube S. Current cigarette smoking among adults aged-United States, 2005–2012. MMWR Morb Mortal Wkly Rep. 2014;63:29–34. [PMC free article] [PubMed] [Google Scholar]
- 2. Dey M, Gmel G, Studer J, Mohler-Kuo M. Health-risk behaviors and quality of life among young men. Qual Life Res. 2014;23:1009–1017. [DOI] [PubMed] [Google Scholar]
- 3. Berg CJ, Ling PM, Hayes RB, et al. Smoking frequency among current college student smokers: distinguishing characteristics and factors related to readiness to quit smoking. Health Educ Res. 2012;27:141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen X, Jacques-Tiura AJ. Smoking initiation associated with specific periods in the life course from birth to young adulthood: data from the National Longitudinal Survey of Youth 1997. Am J Public Health. 2014;104:e119–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Riggs NR, Chou CP, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9:1147–1154. [DOI] [PubMed] [Google Scholar]
- 6. Schane RE, Glantz SA, Ling PM. Nondaily and social smoking: an increasingly prevalent pattern. Arch Intern Med. 2009;169:1742–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gilpin EA, White VM, Pierce JP. How effective are tobacco industry bar and club marketing efforts in reaching young adults? Tob Control. 2005;14:186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Levinson AH, Campo S, Gascoigne J, Jolly O, Zakharyan A, Tran ZV. Smoking, but not smokers: identity among college students who smoke cigarettes. Nicotine Tob Res. 2007;9:845–852. [DOI] [PubMed] [Google Scholar]
- 9. Moran S, Wechsler H, Rigotti NA. Social smoking among US college students. Pediatrics. 2004;114:1028–1034. [DOI] [PubMed] [Google Scholar]
- 10. White HR, Bray BC, Fleming CB, Catalano RF. Transitions into and out of light and intermittent smoking during emerging adulthood. Nicotine Tob Res. 2009;11:211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kenford SL, Wetter DW, Welsch SK, Smith SS, Fiore MC, Baker TB. Progression of college-age cigarette samplers: what influences outcome. Addict Behav. 2005;30:285–294. [DOI] [PubMed] [Google Scholar]
- 12. Nichter M, Lloyd-Richardson EE, Flaherty B, Carkoglu A, Taylor N. Gendered dimensions of smoking among college students. J Adolescent Res. 2006;21:215–243. [Google Scholar]
- 13. Garfinkel L, Stellman SD. Smoking and lung cancer in women: findings in a prospective study. Cancer Res. 1988;48:6951–6955. [PubMed] [Google Scholar]
- 14. Luoto R, Uutela A, Puska P. Occasional smoking increases total and cardiovascular mortality among men. Nicotine Tob Res. 2000;2:133–139. [DOI] [PubMed] [Google Scholar]
- 15. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. 2010;121:1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Philpot SJ, Ryan SA, Torre LE, Wilcox HM, Jalleh G, Jamrozik K. Effect of smoke-free policies on the behaviour of social smokers. Tob Control. 1999;8:278–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Waters K, Harris K, Hall S, Nazir N, Waigandt A. Characteristics of social smoking among college students. J Am Coll Health. 2006;55:133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jason LA, Berk M, Schnopp-Wyatt DL, Talbot B. Effects of enforcement of youth access laws on smoking prevalence. Am J Community Psychol. 1999;27:143–160. [DOI] [PubMed] [Google Scholar]
- 20. Harrison EL, Desai RA, McKee SA. Nondaily smoking and alcohol use, hazardous drinking, and alcohol diagnoses among young adults: findings from the NESARC. Alcohol Clin Exp Res. 2008;32:2081–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Coggins CR, Murrelle EL, Carchman RA, Heidbreder C. Light and intermittent cigarette smokers: a review (1989-2009). Psychopharmacology (Berl). 2009;207:343–363. [DOI] [PubMed] [Google Scholar]
- 22. McKee SA, Falba T, O’Malley SS, Sindelar J, O’Connor PG. Smoking status as a clinical indicator for alcohol misuse in US adults. Arch Intern Med. 2007;167:716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Epstein AM, Sher TG, Young MA, King AC. Tobacco chippers show robust increases in smoking urge after alcohol consumption. Psychopharmacology (Berl). 2007;190:321–329. [DOI] [PubMed] [Google Scholar]
- 24. Lisha NE, Carmody TP, Humfleet GL, Delucchi KL. Reciprocal effects of alcohol and nicotine in smoking cessation treatment studies. Addict Behav. 2014;39:637–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jiang N, Ling PM. Reinforcement of smoking and drinking: tobacco marketing strategies linked with alcohol in the United States. Am J Public Health. 2011;101:1942–1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ramo DE, Liu H, Prochaska JJ. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin Psychol Rev. 2011;32:105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Okoli CT, Richardson CG, Ratner PA, Johnson JL. Adolescents’ self-defined tobacco use status, marijuana use, and tobacco dependence. Addict Behav. 2008;33:1491–1499. [DOI] [PubMed] [Google Scholar]
- 28. Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M. Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005;100:1518–1525. [DOI] [PubMed] [Google Scholar]
- 29. Lee CM, Neighbors C, Woods BA. Marijuana motives: young adults’ reasons for using marijuana. Addict Behav. 2007;32:1384–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Song AV, Ling PM. Social smoking among young adults: investigation of intentions and attempts to quit. Am J Public Health. 2011;101:1291–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ramo DE, Delucchi KL, Hall SM, Liu H, Prochaska JJ. Marijuana and tobacco co-use in young adults: patterns and thoughts about use. J Stud Alcohol Drugs. 2013;74:301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ramo DE, Prochaska JJ. Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. J Med Internet Res. 2012;14:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Facebook. Facebook Advertising Guidelines https://www.facebook.com/ad_guidelines.php Accessed April 28, 2011.
- 34. McCabe SE. Misperceptions of non-medical prescription drug use: a web survey of college students. Addict Behav. 2008;33:713–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hall SM, Tsoh JY, Prochaska JJ, et al. Treatment for cigarette smoking among depressed mental health outpatients: a randomized clinical trial. Am J Public Health. 2006;96:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychol Addict Behav. 1998;12:101–112. [Google Scholar]
- 37. Sobell LC, Sobell MB. Timeline Followback: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- 38. Adamson SJ, Kay-Lambkin FJ, Baker AL, et al. An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug Alcohol Depend. 2010;110:137–143. [DOI] [PubMed] [Google Scholar]
- 39. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. [DOI] [PubMed] [Google Scholar]
- 40. SAS. SAS/STAT® 9.2 User’s Guide; 2008.
- 41. Schulenberg JE, Merline AC, Johnston LD, O’Malley PM, Bachman JG, Laetz VB. Trajectories of marijuana use during the transition to adulthood: the big picture based on National Panel Data. J Drug Issues. 2005;35:255–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ramo DE, Hall SM, Prochaska JJ. Reliability and validity of self-reported smoking in an anonymous online survey with young adults. Health Psychol. 2011;30:693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cobb NK, Graham AL, Bock BC, Papandonatos G, Abrams DB. Initial evaluation of a real-world Internet smoking cessation system. Nicotine Tob Res. 2005;7:207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. McCabe SE, Boyd CJ, Couper MP, Crawford S, D’Arcy H. Mode effects for collecting alcohol and other drug use data: web and U.S. mail. J Stud Alcohol. 2002;63,755–761. [DOI] [PubMed] [Google Scholar]
- 45. Swartz LH, Noell JW, Schroeder SW, Ary DV. A randomised control study of a fully automated internet based smoking cessation programme. Tob Control. 2006;15:7–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. deRuiter WK, Cairney J, Leatherdale ST, Faulkner GE. A longitudinal examination of the interrelationship of multiple health behaviors. Am J Prev Med. 2014;47:283–289. [DOI] [PubMed] [Google Scholar]
- 47. Duggan M, Brenner J. The Demographics of Social Media Users - 2012 (P. I. A. L. Project, Trans.). Washington, DC: Pew Research Center; 2012. [Google Scholar]