Abstract
Objective Family rituals are associated with adaptive functioning in pediatric illness, including quality of life (QoL). This article explores the role of family cohesion and hope as mediators of this association in children with cancer and their parents. Methods Portuguese children with cancer (N = 389), on- and off-treatment, and one of their parents completed self-report measures. Structural equation modeling was used to examine direct and indirect links between family rituals and QoL. Results When children and parents reported higher levels of family rituals, they also reported more family cohesion and hope, which were linked to better QoL. At the dyadic level, children’s QoL was related to parents’ family rituals through the child’s family cohesion. This model was valid across child’s age-group, treatment status, and socioeconomic status. Conclusions Family rituals are important in promoting QoL in pediatric cancer via family cohesion and hope individually and via family cohesion in terms of parent–child interactions.
Keywords: families, hope, parents, pediatric cancer, quality of life
Quality of life (QoL) is a widely accepted outcome in pediatric cancer that is helpful in understanding the impact of these illnesses and treatments on children and families. Decreased QoL is understandable and even expected, particularly during treatment, and may persist after treatment ends (Klassen, Anthony, Khan, Sung, & Klaassen, 2011; Klassen et al., 2007). An understanding of QoL can be enhanced by examining child adjustment in the context of social-ecological (Kazak, 1989) and transactional models (Fiese & Sameroff, 1989) of development, frameworks that highlight the contextual (e.g., family environment) and dynamic mutual effects between children and parents that take place across time.
Family rituals are special events, such as celebrations, traditions, and patterned family interactions, with a symbolic meaning shared by the whole family; these events are examples of family functioning that may be associated with QoL (Fiese et al., 2002). Family rituals have been linked with positive outcomes, such as psychological functioning, adherence to treatment, and health-related behaviors (Crespo et al., 2013; Fiese, 2006; Fiese et al., 2002). Studies in community samples found that family ritual meaning was positively associated with adolescents’ identity, feelings of security (Fiese, 2006), and predicted well-being over 1 year (Crespo, Kielpikowski, Pryor, & Jose, 2011). In pediatric asthma, mothers’ family ritual meaning was associated with less anxiety in the child (Markson & Fiese, 2000). Although positive links between family rituals and children’s health outcomes have been consistently supported, the underlying pathways for these associations are not known.
One possible pathway is family cohesion, a characteristic of families known to be associated with positive child outcomes. Fiese et al. (2002) concluded that when family rituals are interrupted, family cohesion is threatened. In addition, research suggested that children with cancer undergoing treatment with positive family functioning (e.g., high cohesion) were more likely to report better psychological adjustment and QoL (Barakat, Marmer, & Schwartz, 2010; Klassen et al., 2007). Family rituals can provide organization and increase cohesion by strengthening family ties (Crespo et al., 2013; Fiese, 2006; Fiese et al., 2002) that can be important resources to manage the disease, encourage adherence to treatment, and promote adaptive parenting. Parents’ family ritual meaning was connected to adolescents’ well-being through both adolescents’ and parents’ perceptions of family cohesion in a community sample in New Zealand (Crespo et al., 2011). Additionally, Santos, Crespo, Silva, and Canavarro (2012) have demonstrated that family ritual meaning reported by children with asthma was linked to better QoL and to less emotional and behavioral problems, via less conflictual and more cohesive family environments. Together, these data suggest that family ritual meaning promotes better adaptation, and that family cohesion can be a possible path via which this positive influence takes place.
A second possible pathway involves hope. Hope is an overall perception that one’s goals can be met (Snyder et al., 1997), a characteristic that is particularly salient in the face of obstacles or impediments. Family integration can foster optimism (Blotcky, Raczynski, Gurwitch, & Smith, 1985) and hope (Shorey, Snyder, Yang, & Lewin, 2003). According to Snyder (2002), a family environment that lacks boundaries, support, and consistency jeopardizes the development of hopeful thinking. Family ritual meaning may be one way to provide family members the necessary structure and support to develop goal-directed actions. Family rituals allow recognizing past legacies, interpreting the present, and looking to the future for hope (Fiese, 2006). Positive expectations and hope promote adaption to diagnosis and treatment in adolescents (Hinds et al., 1999). Another study of youth with cancer found a positive relationship between hope and satisfaction with life (Hexdall & Huebner, 2007). Hope can buffer the relationship between disability-related stress and adjustment in mothers of children with chronic physical condition (Horton & Wallander, 2001). A more hopeful family might perceive cancer, its treatment, and long-term consequences as challenges to overcome rather than a threat/fatality (Irving, Snyder, & Crowson, 1998). Hence, the family might generate more diverse or helpful coping strategies (Irving et al., 1998) that can translate into better adaptation.
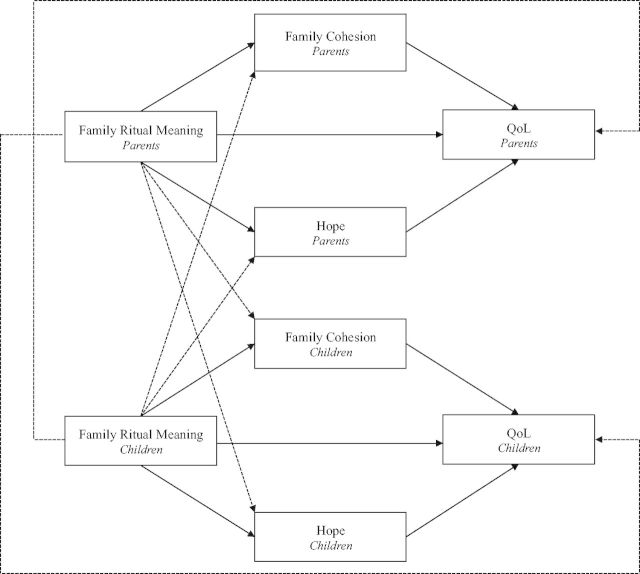
The interdependence of the members of family dyads has been increasingly acknowledged in literature (Kenny, Kashy, & Cook, 2006). Nonetheless, research generally focuses on individuals (parents or children) and less frequently on mutual dyadic influences, or how perceptions of one (e.g., parents) influence the other (e.g., children), and vice versa. The purpose of this study was to analyze the associations between family ritual meaning and QoL, and specifically examine family cohesion and hope as avenues through which family ritual meaning was linked to QoL in children with cancer and their parents. It is also likely that these pathways may differ in parents and children. Children’s QoL is hypothesized to be related to parents’ family ritual meaning directly and through the child’s perception of family cohesion and hope. Parents’ QoL is hypothesized to be related to children’s family ritual meaning directly and through parents’ perception of cohesion and hope (see Figure 1). Finally, as exploratory aims, differences of strengths of significant indirect effects linking each pair of independent and dependent variables through different mediators, and the invariance of the model across child's age-group (child vs. adolescents), treatment status (on- vs. off-treatment), and socioeconomic status (SES; low vs. medium/high).
Figure 1.
Proposed mediation model (individual pathways are solid lines and dyadic pathways are dashed lines). The dashed lines behind the boxes represent direct dyadic effects of parents’ family ritual meaning to children’s quality of life and children’s family ritual meaning to parents’ quality of life.
Method
Participants and Procedures
This study was approved by the ethics committees of three Portuguese public hospitals: Portuguese Institute of Oncology and São João Hospital, both in Porto, and Pediatric Department—Centro Hospitalar e Universitário de Coimbra in Coimbra. Between June 2012 and February 2014, all participants who met inclusion criteria were invited to participate, using a consecutive sampling approach. Inclusion criteria consisted of a diagnosis of cancer at least 3 months ago, aged 8–20 years, receiving treatment for primary diagnosed/relapsed cancer (on-treatment) or had finished antineoplastic treatments for primary diagnosed/relapsed cancer within the past 60 months (off-treatment). Exclusion criteria were comorbidity with other chronic illness (e.g., diabetes), major developmental disorders (e.g., down syndrome), or end-of-life care. Of the 391 parent–child dyads approached to participate, nearly all (N = 389) provided data (99.49%). The two families that declined participation indicated that they were too busy or not interested.
A pediatric oncologist identified the eligible families according to the inclusion/exclusion criteria. The study aims were explained to all eligible participants, and informed consent was obtained from all parents and from children aged ≥13 years; assent was obtained from the younger children. The children and parents were asked to individually complete self-report measures in a paper-and-pencil version. The protocol was administered in a separate room in either the inpatient or outpatient setting in the presence of a research assistant who assured that children and parents were unaware of each other’s responses.
Participants were 389 Portuguese children with cancer and one of their parents1 (85.30% female). Children and parents ranged in age from 8 to 20 years (M = 13.25; SD = 3.45) and 22 to 68 years, respectively. Sociodemographic and clinical characteristics of the sample are provided in Table I. The children were 3 months to 11 years after primary diagnosis and roughly half of the sample was on-treatment (48.80%).
Table I.
Sociodemographic and Clinical Characteristics of the Sample (N = 389 Dyads)
| M/n | SD/% | |
| Parents | ||
| Age, M SD | 42.31 | 6.60 |
| Sex, n% | ||
| Male | 57 | 14.70 |
| Female | 332 | 85.30 |
| Marital status, n% | ||
| Single/separated/divorced/widowed | 60 | 15.42 |
| Married/partnered | 329 | 84.58 |
| SES, n% | ||
| Low | 213 | 54.80 |
| Medium | 139 | 35.70 |
| High | 37 | 9.50 |
| Children | ||
| Age-group, n% | ||
| Children (8–12 years) | 165 | 42.40 |
| Adolescents (13–20 years) | 224 | 57.60 |
| Sex, n% | ||
| Male | 208 | 53.50 |
| Female | 181 | 46.50 |
| Treatment status, n% | ||
| On-treatment | 190 | 48.80 |
| Off-treatment | 199 | 51.20 |
| Time since diagnosis in months, M SD | 28.15 | 27.02 |
| Relapse status, n% | ||
| Nonrelapse | 340 | 87.40 |
| Relapse | 49 | 12.60 |
| Malignancy, n% | ||
| Leukemias | 141 | 36.25 |
| Lymphomas | 97 | 24.94 |
| Langerhans cell histiocytosis | 9 | 2.31 |
| Solid tumor (extra central nervous system) | 104 | 26.74 |
| Central nervous system tumor | 38 | 9.77 |
| Intensity of treatment, n% | ||
| Least intensive | 12 | 3.10 |
| Moderately intensive | 141 | 36.20 |
| Very intensive | 173 | 44.50 |
| Most intensive | 63 | 16.20 |
Note. M = mean; SD = standard deviation.
Measures
Family Ritual Meaning
Family ritual meaning was assessed with the Portuguese version of the Family Ritual Questionnaire (FRQ; Fiese & Kline, 1993). Children and parents answered 15 forced-choice items covering family ritual meaning in three settings: dinnertime, weekend, and annual celebrations (five items for each). Example items are “In some families dinnertime is just for getting food/In other families dinnertime is more than just a meal it has special meaning”; “In some families there are strong feelings at birthdays and other celebrations/In other families annual celebrations are more casual; people aren’t emotionally involved.” Participants first chose the description that best represented their family, and then decided whether that description was really true or sort of true. The four possible answers were scored using a 4-point Likert scale. A total score was computed by taking the average of the item scores, and higher scores indicate perceptions of stronger family ritual meaning. Test–retest reliability of the FRQ over 4 weeks was r = .88 (Fiese & Kline, 1993). Internal consistency in this study was .81 for parents and .80 for children.
Family Cohesion
The children’s and parents’ perceptions of family cohesion were measured with the 9-item Family cohesion subscale from the Portuguese version of the Family Environment Scale (Moos & Moos, 1986). The scale assessed the degree of commitment, help, and support that family members provided to each other (e.g., “Family members help and support one another”; “Family members spend a lot of time together and pay attention to each other”). The participants responded using a 6-point Likert scale. Mean ratings were calculated with higher scores indicating higher levels of family cohesion. Subscale’s reliability was considered adequate with Cronbach’s α .78 and test–retest of r = .86 (Moos & Moos, 1986). Internal consistency on the current sample for parents was .86 and for the children was .77.
Hope
Parents’ hope was measured by the Portuguese version of Adult Hope Scale (AHS; Snyder, Irving, & Anderson, 1991). Participants answered 12 items (e.g., “I can think of many ways to get out of a jam”; “I energetically pursue my goals”) on an 8-point Likert scale; mean ratings were calculated. Children’s hope was measured by the Portuguese version of Children Hope Scale (CHS; Snyder et al., 1997), comprising 6-items (e.g., “I think I am doing pretty well”; “I can think of many ways to get the things in life that are most important to me”). The participants answered the items on a 6-point Likert scale and mean ratings were calculated. In both scales, higher scores denote higher levels of hope. The test–retest reliability of AHS was r = .85 over 3 weeks and r = .71 for CHS over 4 weeks. Internal consistency in this sample was .84 for parents and .80 for children.
Quality of Life
Parents’ QoL was assessed by the Portuguese version of EUROHIS-QOL (Schmidt, Mühlan, & Power, 2006), a self-report variation of the World Health Organization Quality of Life-100 and World Health Organization Quality of Life, abbreviated version. The EUROHIS provided an overall score of physical, psychological, social, and environmental QoL using eight items (e.g., “How satisfied are you with your health”) scored on a 5-point Likert scale. A total score was computed by taking the average of the item scores, with higher scores indicating better QoL. Children’s QoL was measured with the Portuguese version of Pediatric Quality of Life Inventory™ (PedsQL™) 3.0 Cancer Module (Varni, Burwinkle, Katz, Meeske, & Dickinson, 2002), which includes 27 items on eight subscales (Pain and Hurt, Nausea, Procedural Anxiety, Treatment Anxiety, Worry, Cognitive Problems, Perceived Physical Appearance, and Communication). Participants evaluate how frequently a specific problem occurred in the past month (e.g., “I become sick to my stomach when I have medical treatments” or “I worry that my cancer will come back or relapse”), using a 5-point Likert scale. The items were reverse-scored and linearly transformed to fit a 0–100 scale; the total QoL score, with higher scores indicating better QoL, was used. The Cronbach’s α in a sample of 10 countries was .83 for EUROHIS-QOL (Schmidt et al., 2006). The test–retest of PedsQL™ for a part of the sample on-treatment (n = 52) was r = .79 within 1 week. Internal consistency of total score in this study was .83 for parents and .87 for children.
Intensity of Treatment
Intensity of treatment was measured by the Portuguese version of the Intensity of Treatment Rating Scale 3.0 (Kazak et al., 2012). Using data from the medical record, 14 pediatric oncologists, blind to patient identity, classified each child’s treatment into one of four levels of intensity, from level 1 (least intensive treatment) to 4 (most intensive treatment), based on diagnosis, phase of illness (primary diagnosis or relapse), stage/risk level for the patient, and treatment modalities. Interrater reliability for a subset of this sample on- and off-treatment (n = 59) was almost perfect (κ = .97; p < .001) (Santos, Crespo, Canavarro, & Pinto, 2014).
Clinical and Sociodemographic Characteristics
Other relevant clinical information (e.g., time since primary diagnosis) and sociodemographic data were collected from parents. Using data from both parents’ job and educational level, the SES of each family was classified in three levels (low, medium, and high) according to an accepted classification system for the Portuguese context. For analyses purposes, SES was dichotomized into two levels: low (n = 213; 54.80%) and medium/high (n = 176; 45.20%).
Data Analysis
Preliminary descriptive statistics and correlations (Pearson and Spearman) were computed for all outcomes with the Statistical Package for the Social Sciences (SPSS, v. 21; IBM SPSS Inc., Chicago, IL). Structural equation modeling (SEM) was conducted with the Analysis of Moments Structures (AMOS, v. 21; Arbuckle, 2012) to test the direct and indirect pathways. The method of estimation was the maximum likelihood. A model-generation application of SEM (Jöreskog, 1993, as cited in Kline, 2005) was adopted: After examining the results for the full proposed model, we trimmed the model by removing nonsignificant paths using p < .05 as criteria. The model’s goodness of fit was assessed using the reference value for the main fit indexes: chi-square statistic non-significant, comparative fit index (CFI) ≥ .95, and root mean square error of approximation (RMSEA) ≤ .06 (Hu & Bentler, 1999). The significance of indirect paths and differences of strength of significant indirect paths linking each pair of independent and dependent variables through different mediators (Preacher & Hayes, 2008) was evaluated using bootstrap resampling procedures with 5,000 samples (95% bias-corrected bootstrap confidence interval [CI]) (Amos Development Corporation, 2010).
Multigroup analyses were conducted to determine whether the model was valid across the child's age-group (8–12 vs. 13–20 years), treatment status (on- vs. off-treatment), and SES (low vs. medium/high) with structural weights (Byrne, 2010), constrained to be equal across groups, and assessed the difference in model fit using the chi-square difference method (Byrne, 2004).
Results
Preliminary Analyses
Table II presents the means, standard deviations, and correlations for all outcomes.
Table II.
Descriptive Statistics and Matrix of Intercorrelations Among Study Variables for Parents and Children
| Variable | Parents |
Children |
M | Range | SD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||
| Parents | |||||||||||||||
| 1. Family ritual meaning (P) | 3.34 | 1–4 | 0.50 | ||||||||||||
| 2. Family cohesion (P) | .47** | 4.93 | 1–6 | 0.77 | |||||||||||
| 3. Hope (P) | .13** | .31** | 5.83 | 1–8 | 1.13 | ||||||||||
| 4. QoL (P) | .20** | .35** | .36** | 3.53 | 1–5 | 0.53 | |||||||||
| 5. Age (P) | −.07 | .01 | .08 | −.04 | 42.31 | – | 6.60 | ||||||||
| 6. Sex (P; male/female) | −.04 | −.09 | −.08 | −.12* | −.06 | – | – | – | |||||||
| Children | |||||||||||||||
| 7. Family ritual meaning (C) | .35** | .23** | .04 | .12* | −.15** | −.00 | 3.28 | 1–4 | 0.50 | ||||||
| 8. Family cohesion (C) | .27** | .38** | .09 | .18** | −.12* | −.08 | .49** | 5.10 | 1–6 | 0.61 | |||||
| 9. Hope (C) | .13** | .15** | .17** | .08 | .11* | .03 | .13** | .31** | 4.53 | 1–6 | 0.82 | ||||
| 10. QoL (C) | −.02 | .04 | .13** | .11* | .06 | −.01 | .09 | .19** | .28** | 75.18 | 0–100 | 13.58 | |||
| 11. Age (C) | −.07 | .01 | .09 | −.05 | .43** | −.01 | −.22** | −.05 | .12* | −.08 | 13.25 | – | 3.45 | ||
| 12. Sex (C; male/female) | −.05 | −.03 | −.02 | −.03 | .04 | −.08 | −.02 | .08 | −.01 | −.13* | .09 | – | – | – | |
| 13. SES (low/medium-high) | .13* | .15** | .12* | .20** | .07 | −.12* | .08 | .09 | .09 | .02 | −.09 | .04 | – | – | – |
Note. M = mean; SD = standard deviation.
*p < .05; **p < .01.
SEM Test of the Mediation
A path model was constructed to examine the direct and indirect links between family ritual meaning and QoL for parents and children. First, we tested a full model, present in Figure 1, that showed a good fit χ2(4, N = 389) = 5.13, p = .28; CFI = 1; RMSEA = .03. Next, we trimmed this model, by removing the nonsignificant paths. Figure 2 and Table III depict the final trimmed model that presented a good fit χ2(11, N = 389) = 15.87, p = .15; CFI = .99; RMSEA = .03.
Figure 2.
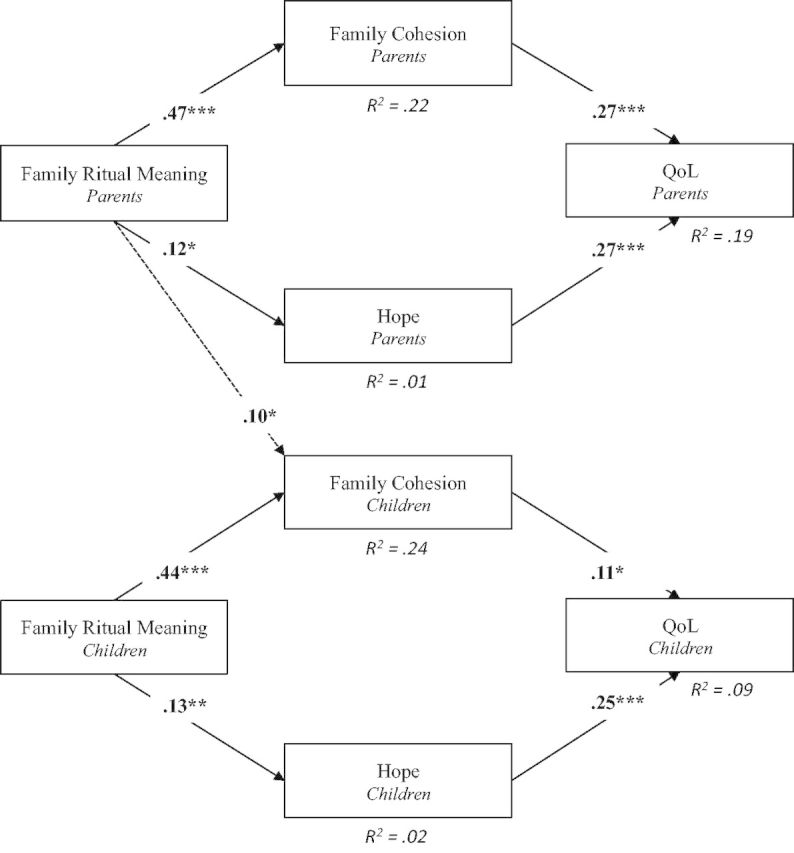
Trimmed model (nonsignificant paths are not represented). The path model shows the indirect effects of family ritual meaning on parents’ and children’s QoL via family cohesion and hope.
Note. Fit indices for the model were as follows: χ2(11, N = 389) = 15.87, p = .15; CFI = .99; RMSEA = .03. Bold figures represent standardized coefficients. For simplicity, covariances (found in Table III) are not depicted; ***p < .001; **p < .01; *p < .05.
Table III.
The Unstandardized Coefficients and Standard Errors for all Parameters, and the Bias-Corrected Bootstrap Confidence Intervals for the Indirect Effects
| Estimated parameters | Unstandardized coefficients | SE | p | BC bootstrap, 95% CIs for indirect effects |
|---|---|---|---|---|
| Direct effects (individual level) | ||||
| Rituals P → Cohesion P | 0.72 | 0.07 | <.001 | |
| Rituals P → Hope P | 0.27 | 0.11 | .016 | |
| Cohesion P → QoL P | 0.18 | 0.03 | <.001 | |
| Hope P → QoL P | 0.13 | 0.02 | <.001 | |
| Rituals C → Cohesion C | 0.54 | 0.06 | <.001 | |
| Rituals C → Hope C | 0.22 | 0.08 | .009 | |
| Cohesion C → QoL C | 2.38 | 1.14 | .036 | |
| Hope C → QoL C | 4.11 | 0.84 | <.001 | |
| Direct effects (dyadic level) | ||||
| Rituals P → Cohesion C | 0.12 | 0.06 | .033 | |
| Covariances | ||||
| Rituals P ↔ Rituals C | 0.09 | 0.01 | <.001 | |
| e (Cohesion P) ↔ e (Hope P) | 0.21 | 0.04 | <.001 | |
| e (Cohesion C) ↔ e (Hope C) | 0.12 | 0.02 | <.001 | |
| e (Cohesion P) ↔ e (Cohesion C) | 0.11 | 0.02 | <.001 | |
| e (Hope P) ↔ e (Hope C) | 0.15 | 0.05 | .002 | |
| e (Cohesion P) ↔ e (Hope C) | 0.05 | 0.03 | .084 | |
| e (Hope P) ↔ e (Cohesion C) | 0.04 | 0.03 | .190 | |
| e (QoL P) ↔ e (QoL C) | 0.41 | 0.32 | .190 | |
| Indirect effects (individual level | ||||
| Rituals P → QoL P (via Cohesion P) | 0.13 | 0.03 | <.001 | [0.08, 0.19] |
| Rituals P → QoL P (via Hope P) | 0.03 | 0.02 | .011 | [0.01, 0.07] |
| Rituals C → QoL C (via Cohesion C) | 0.30 | 0.62 | .028 | [0.15, 2.61] |
| Rituals C → QoL C (via Hope C) | 0.89 | 0.40 | .006 | [0.25, 1.81] |
| Indirect effects (dyadic level) | ||||
| Rituals P → QoL C (via Cohesion C) | 0.28 | 0.19 | .031 | [0.02, 0.81] |
| Differences of strength of indirect effects (individual level) | ||||
| Rituals P → QoL P (via Cohesion P) ≠ | 0.10 | 0.03 | .004 | [0.04, 0.16] |
| Rituals P → QoL P (via Hope P) | ||||
| Rituals C → HRQoL C (via Cohesion C) ≠ | 0.40 | 0.77 | .632 | [−1.22, 1.83] |
| Rituals C → HRQoL C (via Hope C) |
Note. BC = bias-corrected bootstrap; CIs = confidence intervals.
Table III showed that at the individual level, family ritual meaning was associated with QoL, via family cohesion (95% CIs, [0.08, 0.19] and [0.15, 2.61]) and hope (95% CIs, [0.01, 0.07] and [0.25, 1.81]) for both parents and children, respectively. At the dyadic level, children’s QoL was linked to parents’ family ritual meaning through the child’s perception of family cohesion (95% CI, [0.02, 0.81]).
A comparison of the strength of significant indirect effects was calculated. For parents, but not for children, the indirect path from family ritual meaning to QoL via family cohesion was stronger than the one via hope (95% CI, [0.04, 0.16]). Multigroup analyses confirmed that the model was valid across child's age-group Δχ2(9) = 12.96, p = .16, treatment status Δχ2(9) = 14.03, p = .12, and SES Δχ2(9) = 15.78, p = .07.
Discussion
The findings of the current study are congruent with prominent goals of improving the QoL of children with cancer and their parents, providing family support, and developing empirically supported interventions. Family rituals are important components of family functioning but have been underexplored in the pediatric cancer literature.
In line with the social-ecological and transactional models’ assumptions about the mutual influences between parents and children (Fiese & Sameroff, 1989; Kazak, 1989), family ritual meaning was positively associated with better QoL through family cohesion and hope in a large Portuguese sample of patients and parents. In addition, parents’ family ritual meaning was positively associated with children’s family cohesion, which, in turn, was linked to better children’s QoL.
Consistent with prior research showing associations between meaningful family rituals and adaptive family functioning (Fiese, 2006; Imber-Black, 2014), and between positive family functioning and psychological adaptation (Barakat et al., 2010; Litzelman et al., 2013), parents and children who endorsed more family ritual meaning perceived their families as more cohesive and experienced better QoL. It is possible that a family that has frequent and meaningful interactions, perceives their family as closer and interdependent (Crespo et al., 2011). A more cohesive family might be more inclined to share responsibilities (e.g., medication tasks, monitoring of symptoms), decision-making, and offer support—“being there”—which might contribute to better QoL.
The association of family ritual meaning and hope is another new finding in pediatric cancer. When parents and children endorse more family ritual meaning, they have more hope. The data underscore the rationale that family rituals act as an anchor, providing security in times of change (Fiese, 2006; Imber-Black & Roberts, 1998). Families that have a more secure base may feel more hopeful to deal more flexibly with their disease- and treatment-related challenges. They might, for example, engage in more adaptive coping behaviors (e.g., treatment adherence, prevention behaviors). When the families have more hope, they perceive better QoL (Hexdall & Huebner, 2007; Horton & Wallander, 2001). Families who are more hopeful may also be less hypervigilant and/or worry or ruminate less about symptoms, leading to better QoL. However, in the absence of previous empirical evidence and given that the association between family ritual meaning and hope was small, this result must be interpreted with caution.
Similar to the findings of Crespo and colleagues (2011), when parents ascribed more meaning to family rituals, children reported a stronger sense of family cohesion, which, in turn, was linked to better QoL. Although children and adolescents are active participants in daily living routines and cocreators of meaningful rituals, adults play the role of “kinkeepers” and have a stronger say in how family rituals are organized (Fiese, 2006). This may explain why family ritual meaning perceived by parents was associated with children’s QoL, via children’s cohesion, but not the reverse.
The comparison of the strength of pathways of children and adults is novel. For children, both family cohesion and hope are important mediators between family ritual meaning and QoL. However, for parents, family ritual meaning promoted QoL mainly via family cohesion. This suggests that family ritual meaning has a more important role in fostering family integration and closeness, than on promoting an optimistic outlook. Fostering family cohesion through family rituals (e.g., eating meals together imbued with a special meaning shared by family members) may be easier and more tangible than changing attitudes (e.g., hopefulness) and can provide a structure to enhance family well-being. In addition, a cohesive family can lighten the burden of the caregiver by the sharing of responsibilities (Klassen et al., 2007). This may explain why family ritual meaning promotes QoL mainly via family cohesion for the parents, but not for the children.
The associations tested did not differ by child’s age-group, treatment status, or SES. Although the nature of family rituals will naturally differ in families of younger versus older children, the commitment to initiate and maintain rituals may be consistent. Similarly, although being off-treatment differs in major ways from being on-treatment, family rituals, cohesion, and hope seemed to be equally important in both conditions. Moreover, although lower SES may entail increased challenges, this does not seem to compromise the influence of family rituals. It is worth noting that more than half of this sample was composed of low SES families. SES is associated with lower QoL in pediatric cancer in general (Litzelman et al., 2013). This is particularly timely because Portugal is experiencing an economic crisis with increased rates of unemployment and fewer financial supports for families in the health-care system (e.g., less reimbursement of transportation and medicine and increased user fees associated with care, even in a system with National Health System). Although SES obviously is not easy to change, these data suggest that enhancing family ritual meaning can be important even in the presence of financial distress.
Of course, the findings must be considered within the scope of some limitations. First, this is a Portuguese sample and may not be fully generalizable to other cultures. While research in other cultural contexts will help clarify this point, family cohesion and hope are rather universal concepts as are family rituals (e.g., family celebrations, meals). Second, given the cross-sectional research design, it is not possible to establish causality among the variables. Although most literature endorses the role of rituals as promoters of family belonging and cohesion (e.g., Crespo et al., 2011; Fiese et al., 2002; Santos et al., 2012), more longitudinal studies are needed to test the direction of these effects and how family rituals, family cohesion may influence each other over time. An alternative model where hope was the independent variable and family cohesion and ritual meaning were the mediators had a poor fit. Third, although QoL is a widely accepted relevant outcome that covers multiple domains, testing these associations with respect to other outcomes (e.g., anxiety, depression, well-being) will be important. Fourth, because most parents were mothers, caution must be taken when generalizing results; fathers’ perceptions of family ritual meaning and whether fathers’ family ritual meaning holds a similar relation with QoL are not known. Fifth, it is possible there are other clinical important variables not addressed in this study (e.g., treatment adherence, diagnosis, time since diagnosis, intensity of treatment) that might explain more of the variance of the children’s QoL. Sixth, in addition to family rituals, it would be valuable to examine whether family cohesion is also linked to hope. Finally, cancer-specific family rituals may also be meaningful (e.g., marking the end of a chemo cycle) and should be investigated as strategies to promote well-being.
The results provided empirical evidence for the relevance of incorporating an adaptive focus on family rituals in interventions in pediatric cancer, comparable with the family interventions developed for other health problems (Fiese, 2006). In the face of serious illness, meaningful family rituals may contract, disappear, or be put aside (Imber-Black, 2014). Moreover, some families, under specific circumstances, may find it difficult to carry out flexible and meaningful rituals; when family rituals are insufficient or too rigid (Roberts, 2003), the benefits of these family events may be weakened or disappear altogether. The data in this report suggest that, to the extent possible, helping families recognize, preserve, adapt, and develop new healthy family rituals across the course of treatment may help foster QoL by improving family cohesion and hope.
In conclusion, understanding the factors and the mechanisms that link family rituals and functioning can inform the development of interventions. The current study showed that family ritual meaning predicted QoL via family cohesion and hope, at the individual level, and that children’s QoL was influenced by parent’ family ritual meaning, but only via children’s family cohesion, and that these associations are similar across child's age-group, treatment status, and SES. Our findings contribute to the literature that suggests the relevance of interventions that can create, activate, or adapt family rituals, as naturally existing family resources, to address the psychosocial needs of children with cancer and their parents during this adverse period of the family’s life.
Funding
This research was supported by a PhD fellowship from the Portuguese Foundation for Science and Technology (SFRH/BD/80777/2011) to Susana Santos. Additional support for the preparation of this manuscript was provided from K05CA128805 (Kazak) and the Nemours Center for Healthcare Delivery Science.
Conflicts of interest: None declared.
Footnotes
1 The term “parent” is used to denote the main caregiver; however 2.10% of those were grandparents, with whom the children lived.
References
- Amos Development Corporation (Producer). (2010). User-defined estimand: Multiple estimands [DVD]. Retrieved from http://amosdevelopment.com/video [Google Scholar]
- Barakat L. P., Marmer P. L., Schwartz L. A. (2010). Quality of life of adolescents with cancer: Family risks and resources. Health and Quality of Life Outcomes, 8, 63 doi:10.1186/1477-7525-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blotcky A. D., Raczynski J. M., Gurwitch R., Smith K. (1985). Family influences on hopelessness among children early in the cancer experience. Journal of Pediatric Psychology, 10, 479–493. doi:10.1093/jpepsy/10.4.479 [DOI] [PubMed] [Google Scholar]
- Byrne B. M. (2004). Testing for multigroup invariance using AMOS graphics: A road less traveled. Structural Equation Modeling: A Multidisciplinary Journal, 11, 272–300. doi:10.1207/s15328007sem1102_8 [Google Scholar]
- Byrne B. M. (2010). Structural equation modeling with AMOS: Basic concepts applications and programming (2nd ed.). New York, NY: Routledge. [Google Scholar]
- Crespo C., Kielpikowski M., Pryor J., Jose P. E. (2011). Family rituals in New Zealand families: Links to family cohesion and adolescents' well-being. Journal of Family Psychology, 25, 184–193. doi:10.1037/a0023113 [DOI] [PubMed] [Google Scholar]
- Crespo C., Santos S., Canavarro M. C., Kielpikowski M., Pryor J., Feres-Carneiro T. (2013). Family routines and rituals in the context of chronic conditions: A review. International Journal of Psychology, 48, 729–746. doi:10.1080/00207594.2013.806811 [DOI] [PubMed] [Google Scholar]
- Fiese B. H. (2006). Family routines and rituals. New Haven, CT: Yale University Press. [Google Scholar]
- Fiese B. H., Kline C. A. (1993). Development of Family Ritual Questionnaire: Initial reliability and validation studies. Journal of Family Psychology, 6, 290–299. doi:10.1037/0893-3200.6.3.290 [Google Scholar]
- Fiese B. H., Sameroff A. J. (1989). Family context in pediatric psychology: A transactional perspective. Journal of Pediatric Psychology, 14, 293–314. [DOI] [PubMed] [Google Scholar]
- Fiese B. H., Tomcho T. J., Douglas M., Josephs K., Poltrock S., Baker T. (2002). A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? Journal of Family Psychology, 16, 381–390. doi:10.1037//0893-3200.16.4.381 [DOI] [PubMed] [Google Scholar]
- Hexdall C. M., Huebner E. S. (2007). Subjective well-being in pediatric oncology patients. Applied Research in Quality of Life, 2, 189–208. doi:10.1007/s11482-008-9037-7 [Google Scholar]
- Hinds P. S., Quargnenti A., Fairclough D., Bush A. J., Betcher D., Rissmiller G., Pratt C. B., Gilchrist G. S. (1999). Hopefulness and its characteristics in adolescents with cancer. Western Journal of Nursing Research, 21, 600–620. doi:10.1177/01939459922044072 [DOI] [PubMed] [Google Scholar]
- Horton T. V., Wallander J. L. (2001). Hope and social support as resilience factors against psychological distress of mothers who care for children with chronic physical conditions. Rehabilitation Psychology, 46, 382–399. doi:10.1037/0090-5550.46.4.382 [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. doi:10.1080/10705519909540118 [Google Scholar]
- Imber-Black E. (2014). Will talking about it make it worse? Facilitating family conversations in the context of chronic and life-shortening illness. Journal of Family Nursing, 20, 151–163. doi:10.1177/1074840714530087 [DOI] [PubMed] [Google Scholar]
- Imber-Black E., Roberts J. (1998). Rituals for our times: Celebrating, healing, and changing our lives and our relationships. Northvale, NJ: Jason Aronson. [Google Scholar]
- Irving L., Snyder C., Crowson J. (1998). Hope and coping with cancer by college women. Journal of Personality , 66, 195–214. [DOI] [PubMed] [Google Scholar]
- Kazak A. E. (1989). Families of chronically ill children: A systems and social-ecological model of adaptation and challenge. Journal of Consulting and Clinical Psychology , 57, 25–30. doi:10.1037/0022-006X.57.1.25 [DOI] [PubMed] [Google Scholar]
- Kazak A. E., Hocking M. C., Ittenbach R. F., Meadows A. T., Hobbie W., DeRosa B. W., Leahey A., Kersun L., Reilly A. (2012). A revision of the intensity of treatment rating scale: Classifying the intensity of pediatric cancer treatment. Pediatric Blood and Cancer, 59, 96–99. doi:10.1002/pbc.23320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny D. A., Kashy D. A., Cook W. L. (2006). Dyadic data analysis. New York, NY: The Guilford Press. [Google Scholar]
- Klassen A. F., Anthony S. J., Khan A., Sung L., Klaassen R. (2011). Identifying determinants of quality of life of children with cancer and childhood cancer survivors: A systematic review. Support Care Cancer, 19, 1275–1287. doi:10.1007/s00520-011-1193-x [DOI] [PubMed] [Google Scholar]
- Klassen A. F., Raina P., Reineking S., Dix D., Pritchard S., O'Donnell M. (2007). Developing a literature base to understand the caregiving experience of parents of children with cancer: A systematic review of factors related to parental health and well-being. Support Care Cancer, 15, 807–818. doi:10.1007/s00520-007-0243-x [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2005). Principles and practice of structural equation modeling (2nd ed.). New York, NY: The Guilford Press. [Google Scholar]
- Litzelman K., Barker E., Catrine K., Puccetti D., Possin P., Witt W. P. (2013). Socioeconomic disparities in the quality of life in children with cancer or brain tumors: The mediating role of family factors. Psychooncology, 22, 1081–1088. doi:10.1002/pon.3113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markson S., Fiese B. H. (2000). Family rituals as a protective factor for children with asthma. Journal of Pediatric Psychology, 25, 471–480. doi:10.1093/jpepsy/25.7.471 [DOI] [PubMed] [Google Scholar]
- Moos R. H., Moos B. S. (1986). Family environment scale manual (2nd ed.). Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Roberts J. (2003). Setting the frame: Definition, functions, and typology of rituals. In Imber-Black E., Roberts J., Whiting R. A. (Eds.), Rituals in families and family therapy (pp. 3–48). New York, NY: W. W. Norton & Company. [Google Scholar]
- Santos S., Crespo C., Canavarro M. C., Pinto A. (2014). Intensidade do tratamento e qualidade de vida relacionada com a saúde no cancro pediátrico: Resultados da versão Portuguesa da Escala de Classificação da Intensidade do Tratamento 3.0 [Intensity of treatment and health-related quality of life in pediatric cancer: Findings from the Portuguese version of Intensity of Treatment Rating Scale 3.0]. Psychology, Community & Health, 3, 158–171. doi:10.5964/pch.v3i3.97 [Google Scholar]
- Santos S., Crespo C., Silva N., Canavarro M. C. (2012). Quality of life and adjustment in youths with asthma: The contributions of family rituals and the family environment. Family Process, 51, 557–569. doi:10.1111/j.1545-5300.2012.01416.x [DOI] [PubMed] [Google Scholar]
- Schmidt S., Mühlan H., Power M. (2006). The EUROHIS-QOL 8-item index: Psychometric results of a cross-cultural field study. European Journal of Public Health, 16, 420–428. doi:10.1093/eurpub/cki155 [DOI] [PubMed] [Google Scholar]
- Shorey H. S., Snyder C. R., Yang X., Lewin M. R. (2003). The role of hope as a mediator in recollected parenting, adult attachment, and mental health. Journal of Social and Clinical Psychology, 22, 685–715. doi:10.1521/jscp.22.6.685.22938 [Google Scholar]
- Snyder C. R. (2002). Hope theory: Rainbows in the mind. Psychology Inquiry, 13, 249–275. [Google Scholar]
- Snyder C. R., Hoza B., Pelham W. E., Rapoff M., Ware L., Danovsky M., Highberger L., Rubinstein H., Stahl K. J. (1997). The development and validation of the Children's Hope Scale. Journal of Pediatric Psychology, 22, 399–421. doi:10.1093/jpepsy/22.3.399 [DOI] [PubMed] [Google Scholar]
- Snyder C. R., Irving L., Anderson J. R. (1991). Hope and health: Measuring the will and the ways. In Snyder C. R., Forsyth D. R. (Eds.), Handbook of social and clinical psychology: The health perspective (pp. 285–305). Elmsford, NY: Pergamon Press. [Google Scholar]
- Varni J. W., Burwinkle T. M., Katz E. R., Meeske K., Dickinson P. (2002). The PedsQL in pediatric cancer: Reliability and validity of the Pediatric Quality of Life Inventory generic core scales, multidimensional fatigue scale, and cancer module. Cancer, 94, 2090–2106. doi:10.1002/cncr.10428 [DOI] [PubMed] [Google Scholar]