Abstract
Introduction:
Drug users have high rates of tobacco use and tobacco-related disease. Telephone quitlines promote smoking cessation, but their reach among drug users is unknown. We thus aimed to assess utilization of and barriers to telephone quitlines among methadone-maintained smokers.
Methods:
Subjects were opioid-dependent smokers in Bronx, New York, methadone treatment programs who were enrolled in a clinical trial of varenicline. All subjects were offered referral to a free, proactive quitline. We examined quitline records, surveyed barriers to quitline use, and queried reasons for declining referral.
Results:
Of the 112 subjects enrolled, 47% were male, 54% were Hispanic, and 28% were Black. All subjects were offered referral, and 25 (22% of study participants) utilized the quitline. Quitline utilizers (vs. nonutilizers) were significantly more likely to have landline phone service (72 vs. 42%, p = .01), interest in quitline participation (92 vs. 62%, p < .01), and willingness to receive calls (96 vs. 76%, p = .02). Nonutilizers were significantly more likely to report cell phone service lapse (38 vs. 14%, p = .04), and difficulty charging cell phones (19 vs. 0%, p = .02). Reasons for quitline refusal included: (a) skepticism of quitline efficacy; (b) aversion to telephone communication; (c) competing life demands (e.g., drug treatment, shelter); and (d) problems with cell phone service or minutes.
Conclusions:
Despite several limitations to quitline access among methadone-maintained smokers, routine quitline referral was associated with 22% utilization. To expand provision of smoking cessation treatment to opioid-dependent smokers, interventions to promote routine quitline referral in substance abuse treatment programs warrant investigation.
Introduction
Despite successes in tobacco control, significant disparities have emerged as the burden of tobacco use concentrates within specific groups. Among individuals with opioid use disorders in methadone maintenance treatment, an estimated 77%–83% smoke cigarettes.1,2 This has associated health consequences, with tobacco use responsible for over 50% of deaths among substance abuse treatment patients.3,4 National guidelines have called for research on tobacco use treatment in groups that disproportionately suffer from tobacco-related disease, including drug users.5,6
Quitlines are telephone-based programs that provide treatment resources to smokers. Free quitlines are available in all 50 states. Quitline services may include telephone counseling, mailed educational materials, cessation medication, and information about local treatment resources. The effectiveness of quitlines has been documented in the general population,7,8 and among minority smokers.9,10
Despite the need, there is limited provision of smoking cessation services in drug treatment programs.11,12 Telephone quitlines have a decentralized and flexible structure, and broad population reach. Quitlines may reduce treatment barriers, including transportation and cost, and have the potential to address the limited smoking cessation treatment capacity in substance abuse treatment systems.
Our objectives were to describe telephone quitline utilization and explore barriers to quitline utilization among methadone-maintained smokers.
Methods
Setting and Participants
This analysis of telephone quitline utilization includes all participants enrolled in a randomized, placebo-controlled trial of varenicline for smoking cessation among smokers in methadone maintenance treatment. Study methods of the parent trial have been previously described.13 Briefly, participants were recruited at three urban methadone maintenance clinics in Bronx, NY. Participants were eligible if they were: (a) stable in methadone maintenance treatment; (b) at least 18 years old; (c) currently smoking 5 or more cigarettes per day; (d) interested in quitting tobacco use; (e) without varenicline use in the past 30 days; and (f) proficient in English. Participants with unstable medical or psychiatric illness were excluded.
In the parent trial, participants were randomized to receive 12 weeks of varenicline (n = 57) or placebo (n = 55), and were offered structured, brief (≤10min), individual, in-person counseling, and faxed quitline referral. At 12 weeks, cessation was 10.5% and 0% in the varenicline and placebo groups, respectively. Protocols were approved by the Einstein Institutional Review Board.
Study Interventions
Quitline Referral
The NY State Smokers’ Quitline is a free service in which smokers are proactively called by quitline staff and provided with telephone counseling and mailed educational materials. Given that facilitated referral by providers may increase quitline utilization and tobacco cessation compared to self-referral,14 all participants were offered facilitated quitline referral. Participants were informed that a quitline counselor could call them to provide smoking cessation support and materials; participants were not given written quitline materials or instructions for self-referral.
Referral was offered at the baseline research visit for the parent trial after surveys were completed. If the participant was initially undecided, the study coordinator readdressed quitline referral at their subsequent research visit. If the participant declined to consent at either visit, referral to the quitline was no longer offered. If a participant consented to quitline referral, study staff faxed a referral form, with the participant’s contact information, to the quitline.
Data Collection
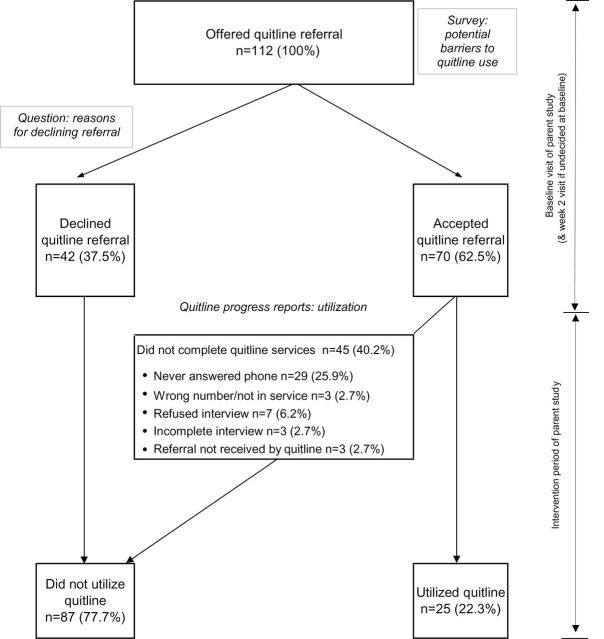
We collected data from three sources: quitline records, quantitative surveys, and open-ended questions (Figure 1).
Figure 1.
Flowchart of quitline utilization and data collection elements. Italicized text denotes data collection elements.
Quitline Utilization
Study coordinators documented whether participants accepted or declined quitline referral. The quitline records documented whether quitline staff successfully contacted participants. If the quitline did not provide services to the participant, staff documented the reason. In some cases, information on the quitline service offered, such as counseling or medication, was recorded.
We extracted the following data from quitline reports: whether (a) participants completed any encounters with quitline staff; (b) quitline staff were unable to reach the participant; or (c) participants were contacted but refused quitline services.
Barriers to Quitline Utilization
All participants completed a survey on potential barriers to quitline use adapted from Lazev et al.15 at the baseline visit before quitline referral was offered. The survey included questions on: (a) cell phone or landline ownership; (b) phone service interruption in the last year; and (c) interest in and willingness to receive quitline calls. Participants who owned cell phones were asked about: (a) problems charging their cell phone; and (b) running out of cell phone service minutes. Response options ranged from 0–3; those ≥1 were considered positive.
Open-Ended Question on Reason for Declining Quitline Referral
At the time of quitline referral, if a participant declined referral, the study coordinator asked a single open-ended question on the reason for declining, without follow-up questions, and recorded the reason in the participant’s own words.
Baseline Measures
Sociodemographic Characteristics
Study staff collected demographic data at the baseline visit.
Tobacco Use Characteristics
Baseline measures of tobacco use included: (a) median number of cigarettes per day; (b) Fagerström Test for Nicotine Dependence; (c) the contemplation ladder, a measure of interest in quitting; (d) quit importance; and (e) quit confidence, each using a 10-point scale.
Psychiatric Comorbidities
Psychiatric measures at baseline included: (a) psychiatric symptoms measured by the Brief Symptom Inventory; (b) Diagnostic and Statistical Manual-IV psychiatric diagnoses measured by the Mini-International Neuropsychiatric Interview; and (c) current psychiatric treatment.
Substance Use Characteristics
We measured median duration in methadone maintenance treatment and used the Alcohol Use Disorder Identification Test to measure hazardous alcohol use.
Data Analysis
Quitline Utilization
We defined quitline utilizers as those who: consented to the referral, were successfully contacted by quitline staff, and completed one or more quitline encounters. Participants were classified as nonutilizers if: they declined referral to the quitline; they initially accepted the referral but did not complete any quitline encounters; their interviews were incomplete; or their referral was not received by the quitline.
Barriers to Quitline Utilization
We compared baseline demographic characteristics, tobacco use characteristics, psychiatric symptoms, substance use, and barriers to quitline utilization between utilizers and nonutilizers. We compared the two groups using chi-square or Fisher exact tests for dichotomous variables, and t tests or Wilcoxon rank-sum tests for continuous variables.
Reasons for Declining Quitline Referral
The investigators reviewed participants’ responses on reasons for declining quitline referral. The investigators collaboratively identified common themes, independently classified the quotes into categories (initial Kappa = 0.84), resolved discrepancies by consensus, then selected representative quotes for each category.
Results
Participant Characteristics
The mean age of participants was 48 years, 47% were male, 54% were Hispanic and 28% were non-Hispanic Black. Participants smoked a median of 15 cigarettes per day and were motivated to quit: the median ladder of change score was 7, which indicates plans to quit in the next 30 days. Median scores for the importance of and confidence in quitting were 10 and 8, respectively.
Quitline Utilization
All 112 participants were offered referral to the telephone quitline (Figure 1). Forty-two participants (37.5%) declined quitline referral and seventy participants (62.5%) accepted quitline referral. Twenty-five participants (22% of study population) utilized the telephone quitline.
Differences Between Quitline Utilizers and Nonutilizers
There were no significant differences in sociodemographic characteristics, tobacco use, psychiatric comorbidities, or varenicline versus placebo group assignment between quitline utilizers and nonutilizers (Table 1).
Table 1.
Baseline Characteristics of Quitline Utilizers and Nonutilizers
| Quitline utilizer (n = 25) | Quitline nonutilizer (n = 87) | p* | |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age, mean (SD) | 47.3 (8.9) | 48.7 (8.7) | .48 |
| Male sex, n (%) | 9 (36) | 44 (51) | .26 |
| Race/ethnicity, n (%) | |||
| Hispanic | 15 (60) | 45 (52) | .32 |
| Black | 5 (20) | 26 (30) | |
| Non-Hispanic White | 4 (16) | 6 (7) | |
| ≤ High school education, n (%) | 19 (76) | 68 (78) | .79 |
| Employed, n (%) | 6 (24) | 26 (30) | .63 |
| Tobacco use characteristics | |||
| Cigarettes/day, median (interquartile range [IQR]) | 15 (10,20) | 15 (10,20) | .49 |
| Fagerström Test of Nicotine Dependence score, median (IQR) | 5 (3,6) | 4 (2,5) | .33 |
| Ladder of change score, median (IQR) | 8 (6,8) | 7 (6,8) | .86 |
| Quit importance, median (IQR) | 10 (9,10) | 10 (8,10) | .74 |
| Quit confidence, median (IQR) | 8 (5,10) | 8 (5,10) | .43 |
| Varenicline treatment group, n (%) | 13 (52) | 44 (51) | 1 |
| Any past quit attempts, n (%) | 20 (80) | 62 (71) | .45 |
| Ever used telephone quitline, n (%), n = 111a | 4 (16) | 7 (8) | .26 |
| Psychiatric comorbidity | |||
| Brief Symptom Inventory Global Severity Index T ≥ 63, n (%) | 3 (12) | 18 (21) | .4 |
| Trauma history, n (%)b | 7 (28) | 32 (37) | .48 |
| Currently receiving psychiatric treatment, n (%) | 14 (56) | 36 (41) | .25 |
| Median duration methadone maintenance, years (IQR) | 4 (2,13) | 7 (2,11) | .67 |
| Hazardous alcohol use, n (%)c | 1 (4) | 12 (14) | .29 |
| Telephone access, n (%) | |||
| Does not own a cell phone, n = 111a | 3 (12) | 12 (14) | 1 |
| Cell phone service lapse, n = 96a,e | 3 (14) | 28 (38) | .04 |
| Problems charging cell phone, n = 103a,f | 0 (0) | 15 (19) | .02 |
| Running out of cell phone service minutes, n = 102a,f | 3 (14) | 25 (31) | .12 |
| Cell phone service lapse, problems charging, or running out of minutes, n = 95g | 6 (29) | 42 (57) | .03 |
| Does not have a landline, n = 111a | 7 (28) | 50 (58) | .01 |
| Landline service lapse, n = 54d,h | 1 (6) | 3 (8) | 1 |
| Interest and willingness to use quitline, n (%) | |||
| Interested in quitlinef | 23 (92) | 54 (62) | .003 |
| Willing to receive calls from quitlinef | 24 (96) | 66 (76) | .02 |
a n < 112 due to missing data if participant refused to answer or answered not applicable.
bAssessed using the Mini-International Neuropsychiatric Interview 6.0.0.
cAssessed using the Alcohol Use Disorder Identification Test, with hazardous alcohol use defined as a score ≥4 for women and ≥8 for men.
dService lapse if in the past year, service has been cut off, disconnected or stopped working.
e n = 96; only asked of participants with a cell phone.
fMeasured on a scale from 0 (not at all) to 3 (extremely); considered positive if ≥1.
g n = 95; only asked of participants with a cell phone; missing data from 1 participant.
h n = 54; only asked of participants with a landline.
*p < .05 in bold.
Barriers to Quitline Utilization
We identified several logistical barriers to quitline utilization (Table 1). Though 86% of subjects reported owning a cell phone, significantly more quitline nonutilizers than quitline utilizers reported lapses in cell phone service (38% vs. 14%, p = .04) or difficulty charging cell phones (19% vs. 0%, p = .02). Quitline utilizers were more likely than nonutilizers to report having a landline (72% vs. 42%, p = .01). A significantly higher proportion of utilizers than nonutilizers reported interest in the quitline (92% vs. 62%, p = .003), and willingness to receive calls from the quitline (96% vs. 76%, p = .02).
Reasons for Declining Referral
We identified five common themes in participants’ reasons for declining quitline referral: (a) skepticism of the efficacy of quitlines or other evidence-based treatments, and preference for alternative cessation methods (“I just don’t believe in it. I want to do it on my own”), 28.6%; (b) aversion to telephone communication (“…Not good with the phone. I’d rather do it in person”), 26.2%; (c) competing life demands (“I’m hardly home. I’m in the meth program…” and “Shelter is too hectic”), 16.7%; (d) problems with phone service or prepaid cell phone minutes (“If I had more minutes I would, but I can’t”) 16.7%; and (e) not interested, 11.9%.
Discussion
Among methadone-maintained smokers who were motivated to quit and who were routinely referred to a smokers’ quitline, 22% utilized the quitline. Cell phone service lapses and problems charging cell phones were identified as potential barriers to quitline utilization. Participants also reported skepticism of quitline efficacy, an aversion to phone communication, and competing life demands as reasons for declining quitline services.
With routine, facilitated quitline referral, 22% of methadone-maintained smokers utilized telephone quitline services. This represents both a higher rate of smoking cessation treatment provision among methadone-maintained smokers than described in national samples,16 and a higher rate of quitline utilization than population-based estimates wherein 1%–2% of U.S. smokers17,18 and 5% of New York State smokers use quitlines annually.19 Our findings approach the 24%–47% rate of quitline utilization seen in studies of facilitated quitline referral in other ambulatory care settings.20–22 In the Bronx, NY, after implementation of a training program, healthcare providers increased faxed referrals to the quitline from negligible rates to reach approximately 0.5% of Bronx smokers.23 Systems to promote facilitated referrals to telephone quitlines by substance abuse treatment providers could expand the reach of quitlines and increase the provision of needed smoking cessation treatment to methadone-maintained smokers.
Though cell phone ownership was high among participants, cell phone service lapses and problems charging cell phones were identified as potential barriers to quitline utilization. Cell phone ownership alone may be insufficient to reach urban smokers with substance use disorders. Research evaluating interventions that address barriers to quitline use is limited. In one trial of smokers with HIV/AIDS, subjects were given a prepaid cell phone; those randomized to receive a cell phone and proactive quitline calls had three times the cessation rates at 3 months than those receiving usual care.24 Given these findings, provision of cell phones or prepaid minutes cards could lower barriers to telephone quitline services among smokers with substance use disorders.
Participants reported competing life demands, an aversion to phone communication, and skepticism of quitline efficacy as reasons for declining quitline services. These findings are consistent with cognitive barriers to quitline use that have been previously described, including stigma and the belief that quitline service would not help or were not needed.25,26 Multiple studies have also demonstrated mistrust of and gaps in knowledge about evidence-based smoking cessation treatments more broadly.27,28 Culturally specific campaigns to promote quitline use have been shown to increase quitline utilization in Hispanic smokers,29,30 but have not been evaluated among opioid-dependent smokers. Whether similar interventions targeting opioid-dependent smokers increase knowledge and utilization of quitlines and other evidence-based treatments warrants investigation.
This study has several limitations. The small sample size may have limited our ability to identify significant effects of factors such as psychiatric comorbidity that may impact quitline utilization. Due to low overall rates of smoking cessation in the parent trial, we were not able to describe the relationship between quitline utilization and quit rates. Offering the survey on potential barriers to quitline utilization before offering the referral could have influenced the acceptance of quitline referral. We were unable to assess if participants utilized the quitline independent of study referral. Our understanding of the timing and content of quitline interventions is limited by quitline records. Finally, our study population of urban, racial/ethnic minority, motivated clinical trial participants recruited from methadone clinics may not generalize to other settings.
In sum, we found that routine referral of motivated smokers in methadone maintenance treatment to a quitline resulted in relatively high quitline utilization. Universal, routine facilitated referral of motivated smokers to quitlines by substance abuse treatment providers could significantly increase the provision of smoking cessation treatment and reduce the high burden of tobacco use among substance abuse treatment patients who smoke.
Funding
This work was supported by CTSA grant UL1 TR001073, TL1 TR001072, KL2 TR001071 from the National Center for Advancing Translational Sciences (NCATS) and National Institute on Drug Abuse grants K23 DA025736 and R25 DA023021 to SN.
Declaration of Interests
None declared.
Acknowledgments
The authors thank J. Arnsten, C. Cunningham, A. Lazev, Y. Ning, and the Division of General Internal Medicine Substance Abuse Affinity Group for assistance with survey measures, data management, and manuscript review.
References
- 1. Richter KP, Gibson CA, Ahluwalia JS, Schmelzle KH. Tobacco use and quit attempts among methadone maintenance clients. Am J Public Health. 2001;91:296–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nahvi S, Richter K, Li X, Modali L, Arnsten J. Cigarette smoking and interest in quitting in methadone maintenance patients. Addict Behav. 2006;31:2127–2134. [DOI] [PubMed] [Google Scholar]
- 3. Hurt RD, Offord KP, Croghan IT, et al. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA. 1996;275:1097–1103. [DOI] [PubMed] [Google Scholar]
- 4. Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Prev Med. 1994;23:61–69. [DOI] [PubMed] [Google Scholar]
- 5. NIH State-of-the-Science Panel. National Institutes of Health State-of-the-Science Conference Statement: tobacco use: prevention, cessation, and control. Ann Int Med. 2006;145:839–844. [DOI] [PubMed] [Google Scholar]
- 6. Fagan P. Eliminating tobacco-related health disparities: directions for future research. Am J Public Health (1971). 2004;94:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ossip-Klein DJ, Giovino GA, Megahed N, et al. Effects of a smoker’s hotline: results of a 10-county self-help trial. J Consult Clin Psychol. 1991;59:325–332. [DOI] [PubMed] [Google Scholar]
- 8. Stead L, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;8:1–137. 10.1002/14651858.CD002850.pub3. [DOI] [PubMed] [Google Scholar]
- 9. Zhu SH, Anderson CM, Tedeschi GJ, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347:1087–1093. [DOI] [PubMed] [Google Scholar]
- 10. Zhu SH, Stretch V, Balabanis M, Rosbrook B, Sadler G, Pierce JP. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol. 1996;64:202–211. [DOI] [PubMed] [Google Scholar]
- 11. Hunt JJ, Cupertino AP, Garrett S, Friedmann PD, Richter KP. How is tobacco treatment provided during drug treatment? J Subst Abuse Treat. 2012;42:4–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fuller BE, Guydish J, Tsoh J, et al. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. J Subst Abuse Treat. 2007;32:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nahvi S, Ning Y, Segal K, Richter K, Arnsten J. Varenicline efficacy and safety among methadone maintained smokers: a randomized placebo-controlled trial. Addiction. 2014;109:1554–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pan W. Proactive telephone counseling as an adjunct to minimal intervention for smoking cessation: a meta-analysis. Health Educ Res. 2006;21:416–427. [DOI] [PubMed] [Google Scholar]
- 15. Lazev AB, Vidrine DJ, Arduino RC, Gritz ER. Increasing access to smoking cessation treatment in a low-income, HIV-positive population: the feasibility of using cellular telephones. Nicotine Tob Res. 2004;6:281–286. [DOI] [PubMed] [Google Scholar]
- 16. Richter K, Choi W, McCool R, Harris K, Ahluwalia J. Smoking cessation services in U.S. methadone maintenance facilities. Psychiatr Serv. 2004;55:1258–1264. [DOI] [PubMed] [Google Scholar]
- 17. Cummins SE, Bailey L, Campbell S, Koon-Kirby C, Zhu S-H. Tobacco cessation quitlines in North America: a descriptive study. Tob Control. 2007;16(suppl 1):i9–i15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ossip-Klein DJ, McIntosh S. Quitlines in North America: evidence base and applications. Am J Med Sci. 2003;326:201–205. [DOI] [PubMed] [Google Scholar]
- 19. New York State Department of Health Bureau of Tobacco Control. New York State Smokers’ Quitline Annual Report 2012 2012. http://www.nysmokefree.com/download/AnnualReport2012.pdf Accessed May 1, 2014.
- 20. Bentz C, Bayley K, Bonin K, Fleming L, Hollis J, McAfee T. The feasibility of connecting physician offices to a state-level tobacco quit line. Am J Prev Med. 2006;30:31–37. [DOI] [PubMed] [Google Scholar]
- 21. Wadland WC, Holtrop JS, Weismantel D, Pathak PK, Fadel H, Powell J. Practice-based referrals to a tobacco cessation quit line: assessing the impact of comparative feedback vs general reminders. Ann Fam Med. 2007;5:135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Willett JG, Hood NE, Burns EK, et al. Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics. Am J Prev Med. 2009;36:337–340. [DOI] [PubMed] [Google Scholar]
- 23. Bernstein SL, Jearld S, Prasad D, Bax P, Bauer U. Rapid implementation of a smokers’ quitline fax referral service in an urban area. J Health Care Poor Underserved. 2009;20:55–63. [DOI] [PubMed] [Google Scholar]
- 24. Vidrine DJ, Arduino RC, Lazev AB, Gritz ER. A randomized trial of a proactive cellular telephone intervention for smokers living with HIV/AIDS. AIDS. 2006;20:253–260. [DOI] [PubMed] [Google Scholar]
- 25. Kreuter M, McQueen A, Caburnay C, et al. Understanding reactions to graphic labels on cigarettes in diverse populations of yourth and young adults at increase risk of smoking. Paper presented at: NIH Tobacco Regulatory Science Conference; 2014; Bethesda, MD. [Google Scholar]
- 26. Solomon LJ, Hughes JR, Livingston A, et al. Cognitive barriers to calling a smoking quitline. Nicotine Tob Res. 2009;11:1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Etter J-F, Perneger TV. Attitudes toward nicotine replacement therapy in smokers and ex-smokers in the general public. Clin Pharmacol Ther. 2001;69:175–183. [DOI] [PubMed] [Google Scholar]
- 28. Fu SS, Burgess D, van Ryn M, Hatsukami DK, Solomon J, Joseph AM. Views on smoking cessation methods in ethnic minority communities: a qualitative investigation. Prev Med. 2007;44:235–240. [DOI] [PubMed] [Google Scholar]
- 29. Burns EKaL, Arnold H. Reaching Spanish-speaking smokers: state-level evidence of untapped potential for quitline utilization. Am J Pub Health. 2010;100(S1):S165–S710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wetter DW, Mazas C, Daza P, et al. Reaching and treating Spanish-speaking smokers through the National Cancer Institute’s Cancer Information Service. a randomized controlled trial. Cancer. 2007;109:406–413. [DOI] [PubMed] [Google Scholar]