Abstract
Introduction:
In 2005, the National Cancer Institute funded the Community Networks Program (CNP), which aimed to reduce cancer health disparities in minority racial/ethnic and underserved groups through community-based participatory research, education, and training. The purpose of this study was to describe the CNP model and their tobacco-related work in community-based research, education, and training using a tobacco disparities research framework.
Methods:
We conducted a comprehensive review of the CNP tobacco-related activities including publications, published abstracts, research activities, trainee pilot studies, policy-related activities, educational outreach, and reports produced from 2005–2009. Two authors categorized the tobacco-related activities and publications within the framework.
Results:
Although there was no mandate to address tobacco, the CNPs produced 103 tobacco-related peer-reviewed publications, which reflects the largest proportion (12%) of all CNP cancer-related publications. Selected publications and research activities were most numerous under the framework areas “Psychosocial Research,” “Surveillance,” “Epidemiology,” and “Treatment of Nicotine Addiction.” Thirteen CNPs participated in tobacco control policymaking in mainstream efforts that affected their local community and populations, and 24 CNPs conducted 1147 tobacco-related educational outreach activities. CNP activities that aimed to build research and infrastructure capacity included nine tobacco-related pilot projects representing 16% of all CNP cancer-related pilot projects, and 17 publications acknowledging leveraged partnerships with other organizations, a strategy encouraged by the CNP.
Conclusions:
The CNP is a promising academic-community model for working to eliminate tobacco-related health disparities. Future efforts may address scientific gaps, consider collaboration across groups, assess the extent of operationalizing community-based participatory research, and improve common tracking measures.
Introduction
While cancer morbidity and mortality have generally declined in the United States,1 minority racial/ethnic groups and those with low socioeconomic status continue to suffer disproportionately from cancer morbidity and mortality. Tobacco use and exposure is a major underlying cause of cancer disparities2–4 because 30% of all cancer deaths in the United States are caused by tobacco.5 Tobacco-related disparities have been defined as differences in: overall exposure to tobacco smoke, use initiation, current patterns of use and cessation; the subsequent health consequences among specific population groups; and differences in capacity and infrastructure as well as access to resources.6 For example, the highest cigarette smoking prevalence rates are among certain racial/ethnic groups including the American Indian and Alaskan Native aggregate group (32.1% men, 22.0% women)7 and Native Hawaiians (26.8%).8 People with low socioeconomic status also have high smoking prevalence rates, that is, 29.2% among persons living below the poverty line and 41.4% among persons with a graduation education development certificate.7 Furthermore, some populations have an unexplained burden and suffer differentially from lung cancer compared to other groups. Black men smoke fewer cigarettes per day, have a later age of onset of regular smoking, and have current smoking rates similar to that of whites, yet bear a longstanding history of higher lung cancer incidence and mortality3,9 as well as other cancers of the upper aerodigestive tract.10,11 Addressing tobacco use and exposure among groups who experience disparities may significantly reduce the overall cancer burden among these groups.
The National Cancer Institute (NCI) has played a key role in supporting communities in their efforts to reduce their tobacco-caused cancer burden in minority and underserved communities. In 2005, the NCI’s Center to Reduce Cancer Health Disparities allocated 95 million dollars through cooperative agreements to support 25 networks over 5 years through its Community Networks Program (CNP). With a conceptual framework based on Community-based Participatory Research (CBPR) principles and the Logic Model (which specifies relationships in program objectives, components, activities, and outputs with expected outcomes),12 the CNP networks were charged to engage in efforts that aimed to reduce cancer health disparities among racial/ethnic minorities and underserved populations through community-based participatory research, education, and training. CBPR requires academically trained experts to be engaged with the community in the planning, development, implementation, evaluation, and dissemination of the research. The CNPs mostly incorporated CBPR principles, as reported using a 27-question assessment tool, and varied in the extent to which individual CNPs employed CBPR principles in their work.13 The CNPs selected cancer topics of their choice, which depended on the needs and interests of the specific population represented. An additional objective of the CNP was to train researchers who will continue to reduce disparities in communities; this occurred mainly through the use of pilot project grant awards. The CNP used the Logic Model to help describe linkages among program resources and activities with outcomes, and each center was encouraged to leverage formal and informal partnerships with others interested in accomplishing common objectives of reducing cancer disparities through community education and policy activities.
The purpose of this study was to describe the CNP model and the CNP networks’ tobacco-related work in community-based research, education, and training. Due to the diversity and heterogeneity of the CNP, we use a scientific framework for addressing tobacco disparities research. Based on the synthesis of CNP experiences and current literature, we make recommendations for future directions based on the CNP work to date.
Methods
Framework
To organize and synthesize the description of the CNP experiences, we used a scientific framework (Figure 1) described by Fagan et al.6 that proposed three primary domains to be addressed to eliminate tobacco disparities: (1) understanding tobacco use and related diseases; (2) reducing tobacco use and related diseases; and (3) research capacity and infrastructure. The first two domains identify key scientific areas of focus. To understand tobacco use and related diseases, key areas include: epidemiology, surveillance, psychosocial research, basic biology, marketing, and harm reduction. To reduce tobacco use and related diseases, key areas include: harm reduction, policy, community/state involvement, prevention of tobacco use and nicotine addiction, treatment of nicotine addiction, and counter-marketing. The third domain “research capacity and infrastructure” helps to ensure the availability of necessary resources and mechanisms to provide a strong foundation upon which effective research can be designed and conducted in/with community, clinical, and other settings. For example, this support from national funders has focused on areas such as training programs to increase the skills, competencies, and number of researchers from minority and underrepresented groups and to encourage working with the community to build capacity and conduct research.
Figure 1.
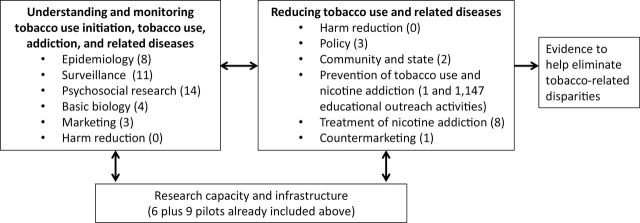
Number of National Cancer Institute’s Community Networks Program publications and activities (2005–2009) within a framework6 for scientific domains and areas to be addressed in efforts to eliminate tobacco-related disparities.
Data Sources
Data were gathered on the CNP tobacco-related activities including peer-reviewed publications, published abstracts, trainee pilot project descriptions, policy-related activities, and educational outreach. The CNP networks (Table 1) were required to report these activities and publications to a national evaluator, Consulting Services & Research, Incorporated, whom we contacted for information synthesized through year 4 of the program (ending August 31, 2009).14 CNP principal investigators also were contacted individually for additional information from their networks. Two authors categorized selected tobacco-related publications and activities within the framework,6 described above, by the designated CNP racial/ethnic or underserved populations (black, American Indian/Alaska Native, Asian American, Latino, Native Hawaiian/Pacific Islander, and Underserved [NCI category used here]). To simplify attribution in the results section, we assigned a number to each of the 25 CNP networks, by population as seen in Table 1.
Table 1.
National Cancer Institute’s CNP by Population
| Number | Population focus | CNP name | Principal investigator |
|---|---|---|---|
| 1 | Black | CNP for Older, Underserved, African-American Adults | Terrance L. Albrecht, PhD |
| 3 | Black | Deep South Network for Cancer Control | Edward E. Partridge, MD |
| 4 | Black | Meharry Medical College-Community Health Centers Network | John E. Maupin, Jr., DDS |
| 5 | Black | National Black Leadership Initiative on Cancer III | David Satcher, MD, PhD |
| 6 | Black | Program for the Elimination of Cancer Disparities | Dione Farria, MD, MPH |
| 7 | Black | South Carolina Cancer Disparities Community Network | James R. Hebert, ScD, MSPH |
| 8 | American Indian/Alaska Native | American Indian/Alaska Native Initiative on Cancer | Judith S. Kaur, MD, MA |
| 9 | American Indian/Alaska Native | Native People for Cancer Control | Dedra Buchwald, MD |
| 10 | American Indian/Alaska Native | Southwest American Indian Collaborative Network | Kathryn Coe, PhD |
| 11 | American Indian/Alaska Native | University of Oklahoma Community Networks Project | Laura Beebe, PhD |
| 12 | Asian American | Asian American Network for Cancer Awareness, Research, and Training | Moon S. Chen, Jr., PhD, MPH |
| 13 | Asian American | ATECAR-Asian Community Cancer Network | Grace X. Ma, PhD |
| 14a | Latino | Colorado Front Range Latino Community Network | Estevan T. Flores, PhD |
| 15 | Latino | Hispanic Community Network to Reduce Cancer Disparities | Beti Thompson, PhD |
| 16 | Latino | Latin American Cancer Research Coalition | Elmer E. Huerta, MD, MPH |
| 17 | Latino | Redes en Acción | Amelie G. Ramirez, DrPH, MPH |
| 18 | Pacific Islander | American Samoa Community Cancer Network | Victor W. Tofaeono, MD, FACS |
| 19 | Native Hawaiian/Pacific Islander | ‘Imi Hale—Native Hawaiian Cancer Network | Clayton Chong, MD |
| 20 | Pacific Islander | Weaving an Islander Network for Cancer Awareness, Research, and Training | Sora P. Tanjasiri, DrPH, MPH |
| 21 | Underserved | Appalachia Community Cancer Network | Mark B. Dignan, PhD, MPH |
| 22 | Underserved | Arkansas Cancer Community Network | Ronda S. Henry-Tillman, MD |
| 23 | Underserved | Maryland Regional Community Network Program to Eliminate Cancer Health Disparities | Claudia Baquet, MD, MPH |
| 24 | Underserved | Massachusetts Community Networks to Eliminate Cancer Disparities through Education, Research, and Training | Howard Koh, MD, MPH |
| 25 | Underserved | Tampa Bay Community Cancer Network | Cathy D. Meade, PhD, RN, FAAN |
CNP = Community Networks Program.
aCNP network #2 (Carolina Community Network) did not conduct tobacco-related activities, but instead focused on other cancer control topics.
We include activities that have not been published in the peer-review literature. Education/outreach activities were categorized under the scientific framework area of “Prevention of Tobacco Use.” Because CNP members were encouraged to leverage partnerships, we also included publications from studies that were not necessarily funded by the CNP, but included a CNP member as a co-author. We did not include tobacco-related activities and articles that were not related to CNP populations.
Results
Overview of CNP Activities From Years 1–4
The majority of the 25 CNP networks (96%) either reported conducting tobacco-related activities or published tobacco-related articles since 2005. From 2005–2009, the CNP networks published over 103 articles related to tobacco, which constitute the largest proportion (12%) of the CNP cancer-related publications, and conducted 1147 tobacco-related education/outreach activities.14 Under our review, the greatest number of selected contributions categorized here under the framework (Figure 1) as key scientific areas was for “Psychosocial Research,” “Surveillance,” “Epidemiology,” and “Treatment of Nicotine Addiction.” We did not find any activities or publications under the framework area of “Harm Reduction.” To address the objective to develop and implement CBPR and train young investigators, there were nine tobacco-related pilot projects, representing 16% of all CNP cancer-related pilot projects.14 Tables 2 and 3 describe the CNP activities by each minority racial/ethnic group under each of three framework domains and their corresponding key scientific areas. Table 4 summarizes the overall CNP policy-related activities and educational outreach for each CNP.
Table 2.
Summary of Findings by Scientific Area6 From CNP Tobacco Control Publications (2005–2009): Understanding Tobacco Use and Related Diseases (Domain 1)
| Population | CNP number and authors, study design and information | Findings |
|---|---|---|
| Understanding tobacco use and related diseases: epidemiology | ||
| Black | 415 , leveraged partnership, cross-sectional survey | Participants with diabetes, but no additional chronic conditions, were more likely to report being former smokers. |
| Black | 716 , longitudinal study | Blacks in South Carolina have elevated rates of lung cancer compared with European Americans and in relation to what would be predicted based on their tobacco use. |
| Black | 711 , longitudinal study | Blacks in South Carolina have elevated rates of esophageal cancer compared with European Americans and in relation to what would be predicted based on their tobacco use. |
| Black | 717 , longitudinal study | Blacks in South Carolina have elevated rates of oral cavity cancer compared with European Americans and in relation to what would be predicted based on their tobacco use. |
| Black | 718 , longitudinal study | Blacks have nearly twice the mortality-to-incidence rate ratio (a population measure of survival) than European Americans in South Carolina for female breast, prostate, and oral cancer. |
| Black | 619 , cohort study | Current smoking increased the risk of pancreatic cancer in both blacks and whites, but blacks smoked fewer cigarettes per day and yet had similar risks in developing pancreatic cancer and higher risk for mortality. |
| Asian American | 1220 , cross-sectional survey | Vietnamese women have high rates of cervical cancer, which is causally linked to tobacco. Almost half of Vietnamese American women living in Seattle lived with a smoker, but Pap testing behavior did not differ among women who lived with or without a smoker in the home. |
| Asian American | 1221 , cross-sectional survey | Chinese American smokers reported higher depressive symptoms among current smokers compared with former smokers. Women smokers had higher depression symptoms, even after adjusting for acculturation and social support. |
| Understanding tobacco use and related diseases: surveillance | ||
| Black | 422 , cross-sectional survey; leveraged partnership | Smoking prevalence rates among blacks were highest among single men, the lowest socioeconomic level, the unemployed, and those aged 40–50 years. |
| Black | 323 , cross-sectional survey; pilot | Smoking prevalence rates are highest for cigarettes, marijuana and blunts respectively among young adult black men in five counties of rural Alabama’s Black Belt region. Mini-cigar use was lower than expected. |
| American Indian/ Alaska Native | 824 , cross-sectional survey | Physicians attending American Indian and Alaska Native health care conferences were surveyed about tobacco behavior. The majority of physicians were lifelong nonsmokers, and nearly all reported asking and advising smokers to quit. |
| American Indian/ Alaska Native | 825 , cross-sectional survey | Pregnant Alaska Natives from western Alaska have extremely high tobacco use rates (79%) with the majority using tobacco during pregnancy and postpartum. |
| American Indian/ Alaska Native | 926 , cohort study; leveraged partnership | Two American Indian tribes, which were culturally and regionally distinct, showed that the Northern Plains group had a higher cumulative incidence of smoking initiation by age 18 and earlier ages of initiation in more recent birth cohorts than the Southwest group. |
| Asian American | 1227 , cross-sectional survey | California Asian Americans are lighter smokers than the general population, with these smokers more likely to be women, not Koreans, higher educated, and bilingual with high English proficiency. |
| Asian American | 1228 , cross-sectional survey, leveraged partnership | California Vietnamese men smoked at higher rates than the general population, with associated risk factors including Vietnamese-specific experiences (eg, military service, refugee camp) and higher depression symptoms. |
| Asian American | 1229 , cross-sectional survey | Vietnamese in Seattle, Washington have high smoking prevalence rates compared to the general population. |
| Asian American | 1230 , leveraged partnership, qualitative | The results of focus groups conducted among three South Asian enclaves showed that cultural context and a lack of knowledge influenced high rates of using cultural tobacco products, such as paan, paan masala, and hookah. |
| Asian American | 1331 , cross-sectional survey | Asian Americans in Pennsylvania and New Jersey and reported smoking prevalence rates higher than the general population, with differences by ethnic subgroup and gender. They were also frequently exposed to secondhand smoke exposure in the home, work, and in restaurants. |
| Asian American | 1332 , cross-sectional survey | The majority of Korean American smokers in Philadelphia reported ever attempting to quit, but over half had not in the past year. |
| Understanding tobacco use and related diseases: psychosocial research | ||
| Black | 533 , qualitative, leveraged partnerships | Primary care providers for underserved patients in metro Atlanta and rural Georgia reported that barriers for smoking cessation included patients presenting in “crisis” rather than by appointment and inability to pay. |
| American Indian/ Alaska Native | 834 , qualitative | Focus groups showed that Alaska Native adolescent tobacco users reported that they preferred cessation interventions that included location that were accessible to them, a group-based format, inclusion of medication, and personal stories. Motivators to quit included adverse health effects, improved self-image and appearance, and being a future role model. |
| Asian American | 1235 , qualitative | Chinese and Vietnamese American men reported they smoked to be sociable or to alleviate stress. Barriers to quitting smoking included low health knowledge and will-power. |
| Asian American | 1236 , qualitative | Chinese American men who were current smoking reported that culturally-specific beliefs about tobacco use included giving tobacco as gifts and they believed that quitting smoking abruptly will lead to physical imbalance. |
| Asian American | 1237 , cross-sectional survey | Chinese and Vietnamese American current and former smokers reported that in addition to will-power and self- determination, family encouragement and physician recommendations were significant facilitators of cessation. |
| Asian American | 1238 , qualitative, pilot | Chinese current, former, and passive smokers indicated how smoking cessation is facilitated by secondhand smoke concerns: (1) understanding secondhand smoke harms, (2) smoker empathy for the nonsmoker, (3) smoking-related interpersonal conflict, and (4) social environment restrictions. |
| Asian American | 1239 , longitudinal study, leveraged partnership | California Chinese and Vietnamese American adolescents had higher susceptibility to smoking at baseline and the influence of friends were predictors of smoking at follow-up. |
| Asian American | 1240 , cross-sectional survey | Among Vietnamese American young people, four psychographic segments were identified with “risk seekers” and “stressed pessimists” reporting higher likelihood of trying smoking. |
| Asian American | 1241 , qualitative, pilot | Filipina high school girls in Hawaii identified factors facilitating smoking: relationship stress with family, being popular, academic stress, and getting cigarettes from family and friends. Top protective factors for smoking were being involved with sports and having family responsibilities. |
| Latino | 14 and 1742 , qualitative | Barriers to using medications for smoking cessation among Colorado Latino smokers included perceptions that smoking is a weakness rather than an illness and that medications are mistrusted. |
| Latino | 1643 , observational study; pilot | Proactive recruitment (face-to-face contact by research staff) was comparable in efficiency and had lower incremental costs per additional enrollee compared to reactive recruitment (mass media and flyers) in enrolling Latino men (Central and South American) for a telephone-based tobacco survey in the DC metropolitan area. |
| Latino | 1744 , observational study; pilot | Spanish-speaking immigrant smokers from the Houston area were intensively assessed around a quit date to examine mechanisms underlying the process of smoking cessation. The majority of participants were able to comply with this intensive assessment, and participants received behavior counseling and nicotine patches with half quitting at 4 weeks. |
| Native Hawaiian and Pacific Islander | 1945 , qualitative | Rural Native Hawaiian men and women to examine perceived supports and barriers for smoking cessation strategies. Compared to current smokers, former smokers found social (especially family), psychological, and physical factors helpful in quitting, and reported using more behavioral and religious/spiritual strategies to quit. |
| Native Hawaiian and Pacific Islander | 1946 , qualitative | Intervention preferences were examined among rural Native Hawaiian adolescent current and former smokers. Participants expressed that smoking was a small part of youth concerns, and preferable to using harder drugs, which were perceived as more dangerous to health and leading to family and community disintegration. |
| Understanding tobacco use and related diseases: basic biology | ||
| Black | 747 , qualitative | The investigation by CNP #7 into the biological role of menthol cigarettes and carcinogenesis in blacks arose from community discussions about alcohol as a co-factor that enhances carcinogenesis. |
| Black | 710 , experimental | Menthol, especially in the synergistic presence of ethanol, increases permeation and reservoir formation of two known tobacco carcinogens, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone and benzo(a)pyrene, findings that could help to explain anomalously high rates of cancers of the upper aerodigestive tract in blacks. |
| Alaska Native | 848 , experimental, leveraged partnership | Alaska Native adult users and nonusers were compared for nicotine exposure and metabolism of cigarettes, commercial chew tobacco, or Iqmik (homemade mixture of chew tobacco and ash). Users with slower CYP2A6 activity have lower tobacco consumption and lower tobacco-specific nitrosamine exposure and bioactivation. |
| Native Hawaiian | 1949 , experimental, pilot | Hawaiians have higher lung cancer incidence even after controlling for smoking, but while the ciliary function of whites had higher mean velocities than Hawaiians this was not statistically significant. |
| Understanding tobacco use and related diseases: marketing | ||
| Asian American and Native Hawaiian/ Pacific Islander | 2050 , intervention, leveraged partnership | Southeast Asian, Chinese, Filipino, and Pacific Islander (Chamorro) youth recruited from community agencies in three cities used Photovoice to demonstrate the influence of environmental factors. Three themes identified included advertisements targeting teens, cigarette ads and sales in the community, and negative appearance of the community environment. |
| Underserved | 2451 , observational study, leveraged partnership | Data collected by youths on tobacco advertisements in their neighborhood stores demonstrated that (1) communities where more residents spoke a language other than English at home were over twice as likely to have a high level of tobacco advertising in their local stores and (2) a low socioeconomic position. Communities of blacks with low socioeconomic position had more advertisements (including near schools) than those communities with few minorities and high socioeconomic position, despite being in close geographic proximity to each other. |
| Underserved | 11, 17, 2452 , qualitative, leveraged partnerships | The Tobacco-Related Messages and Media (TeRMM) project purpose is to develop and validate a set of “media/message” exposure measures that can be used widely. With recruitment support from community coalitions, focus groups were conducted among blacks, American Indians, and Latinos for eliciting themes used towards developing exposure measures. |
CNP = Community Networks Program.
Table 3.
Summary of Findings by Scientific Area6 from CNP Tobacco Control Publications (2005–2009): Reducing Tobacco Use and Related Diseases (Domain 2) and Research Capacity and Infrastructure (Domain 3)
| Population | CNP number and authors, study design and information | Findings |
|---|---|---|
| Reducing tobacco use and related diseases: policy | ||
| Asian American | 1253 , cross-sectional survey | Smoke-free home rules were associated with California Asian Americans being a former smoker, particularly among recent immigrants, and also lighter smoking. |
| Asian American | 1254 , cross-sectional survey | California Chinese and Korean American lower-educated women were more likely to report greater exposure at home or work than higher-educated women, despite similar proportions of smoke-free rules at home, indoor work policies, and health knowledge. |
| Asian American | 1355 , cross-sectional survey | Chinatown businesses about Philadelphia’s smoking ordinance and determined high general awareness but less knowledge about relevant details. Retail businesses had greater difficulty than restaurants with implementation and enforcement. |
| Reducing tobacco use and related diseases: community/state involvement | ||
| Black | 456 , longitudinal study, leveraged partnership | The Nashville REACH project demonstrated that community partnerships and strategies, including policy change in a majority black community was associated with decreasing trends in daily smoking and smoking uptake, but not for quitting. |
| Asian American | 1257 , longitudinal study, leveraged partnership | A community-level education strategy that included tobacco decreased smoking prevalence and increased quit ratios among Asian American/Pacific Islander (Vietnamese, Cambodian, mixed) men in three states. |
| Reducing tobacco use and related diseases: prevention of tobacco use | ||
| American Indian | 958 , program development, pilot | An innovative and interactive supplemental tobacco curriculum was developed for Native American youth, who have high prevalence rates despite required tobacco education in Washington schools. This project incorporated social development models and skill-based approaches. |
| Reducing tobacco use and related diseases: treatment of nicotine addiction | ||
| Black | 559 , randomized trial | A provider training intervention was conducted with black physicians on national guidelines for treating tobacco. Medical charts were abstracted pre- and post-intervention, demonstrating significant improvement in asking, advising, assessing, assisting, and arranging follow-up on smoking cessation. |
| American Indian/ Alaska Native | 814 , program development | As part of community programming, a youth retreat was conducted to decrease tobacco use, a culturally tailored video was developed to inform pregnant women of tobacco health risks, and Tobacco Treatment Specialists were trained and certified. |
| Asian American | 1360 , randomized trial | Chinese and Korean American smokers who participated in a brief, culturally-adapted smoking cessation intervention versus general health counseling had higher quit rates at 1 month but not 3 months. |
| Asian American | 1361 , randomized trial, Pilot | A culturally-sensitive smoking intervention program for low-income Chinese American smokers in New York City demonstrated higher quit rates at 6 months than the control. |
| Latino | 1562 , program development | Three “Quit & Win” contests funded by American Lung Association in Washington were determined to be a relatively inexpensive activity and aroused interest, involved families, and helped smokers to quit with high cessation rates at 1 month. |
| Latino | 1763 , randomized trial, leveraged partnership | Smokers in a Spanish/English Internet smoking cessation trial across 68 countries were randomized to four conditions, from a basic guide to additional components (e-mail reminders, mood management lessons, an asynchronous bulletin board group), but there were no significant differences in treatments at 12 months. |
| Native Hawaiian/ Pacific Islander | 1964 , quasi-experimental | A random review of charts in five operationally-independent Native Hawaiian Health Care Systems demonstrated improved documentation about tobacco use (almost all) and intervention (over half to all) with linkage of smokers to quit line, medication, and/or intensive treatment. |
| Underserved | 2165 , quasi-experimental, pilot, leveraged partnership | A smokeless tobacco cessation program, entitled “Enough Snuff,” was adapted and implemented in rural Pennsylvania. Through targeted print and broadcast media, 25 people called to inquire about the program and eight completed the program. Quit rates were high for both smokeless tobacco and all tobacco. |
| Reducing tobacco use and related diseases: countermarketing | ||
| Native Hawaiian/ Pacific Islander | 198 , program development | “REAL”, Hawaii’s youth-led movement with more than 4000 young people members, aims to increase youth advocacy and reduce the industry’s influence over youth. One example of a countermarketing campaign reversed the messaging of a “Share the Love” free cigarette coupon from American Spirit to encourage youth instead to educate the community about the tobacco industry’s tactics and support quitting. |
| Research capacity and infrastructure (pilots repeated from tables above) | ||
| American Indian and Latino | 11 and 1766 , case study | The study examined the development of community-specific conceptual frameworks for building capacity for tobacco control with case studies of two ethnic communities: an American Indian community in Oklahoma and the Hispanic/Latino Tobacco Education Partnership organizations in California. Capacity is contingent upon the presence of leadership, collaboration, programs, distribution of funds and resources, development of policies and an underlying understanding of community strengths, history, values and participation. |
| Native Hawaiian | 198,67–70 , case study, leveraged partnerships | CNP #19’s socio-ecological approach to tobacco control for Native Hawaiians have been highlighted as a national example of sustainability using a dynamic and multifaceted approach: (1) a program based on findings from research focused on indigenous communities, (2) defining tobacco use and addiction in a social and cultural perspective, (3) understanding cultural background and traditions of the target communities for a sustainable program, and (4) working towards sustainability in an indigenous health setting.68 CNP #19 has been an active participant in two 5-year strategic plans (2005–201070 , 2011–20168 ) for tobacco prevention and control in Hawaii that were developed through an intensive community process involving over 250 individuals and organizations and culminated in the drafting of principles and priorities by over 100 stakeholders across the State of Hawaii. CNP #19 used the APPEAL Community Readiness Model67 to assess each Native Hawaiian Health Care System and demonstrate gaps, which led to the collaboration for systems change in addressing tobacco cessation. Infrastructure development to include Native Hawaiian data and engagement include the (1) Native Hawaiian Smokers’ Survey, conducted in 1999 and 2005 and then incorporated into Hawaii’s Behavioral Risk Factor Surveillance Survey8 and (2) a Native Hawaiian Institutional Review Board administered by CNP #19’s parent organization.69 |
| Black | 323 , cross-sectional survey, pilot | Smoking prevalence rates are highest for cigarettes, marijuana and blunts respectively among young adult black men in five counties of rural Alabama’s Black Belt region. Mini-cigar use was lower than expected. |
| Asian American | 1238 , qualitative, pilot | Chinese current, former, and passive smokers described how smoking cessation relates to secondhand smoke concerns: (1) understanding secondhand smoke harms, (2) smoker empathy for the nonsmoker, (3) smoking- related interpersonal conflict, and (4) social environment restrictions. |
| Asian American | 1241 , qualitative, pilot | Filipina high school girls in Hawaii identified factors facilitating smoking: relationship stress with family, being popular, academic stress, and getting cigarettes from family and friends. Top protective factors for smoking were being involved with sports and having family responsibilities. |
| Latino | 1643 , observational study, pilot | Proactive recruitment (face-to-face contact by research staff) was comparable in efficiency and had lower incremental costs per additional enrollee compared to reactive recruitment (mass media and flyers) in enrolling Latino men (Central and South American) for a telephone-based tobacco survey in the DC metropolitan area. |
| Latino | 1744 , observational study, pilot | Spanish-speaking immigrant smokers from the Houston area were intensively assessed around a quit date to examine mechanisms underlying the process of smoking cessation. The majority of participants were able to comply with this intensive assessment, and participants received behavior counseling and nicotine patches with half quitting at 4 weeks. |
| Native Hawaiian | 1949 , experimental, pilot | Hawaiians have higher lung cancer incidence even after controlling for smoking, but while the ciliary function of Caucasians had higher mean velocities than Hawaiians this was not statistically significant. |
| American Indian | 958 , program development, pilot | An innovative and interactive supplemental tobacco curriculum was developed for Native American youth, who have high prevalence rates despite required tobacco education in Washington schools. This project incorporated social development models and skill-based approaches. |
| Asian American | 1361 , randomized trial, pilot | A culturally-sensitive smoking intervention program for low-income Chinese American smokers in New York City demonstrated higher quit rates at 6 months than the control. |
| Underserved | 2165 , quasi-experimental, pilot, leveraged partnership | A smokeless tobacco cessation program, entitled “Enough Snuff,” was adapted and implemented in rural Pennsylvania. Through targeted print and broadcast media, 25 people called to inquire about the program and 8 completed the program; quit rates were high for both smokeless tobacco and all tobacco. |
CNP = Community Networks Program.
Table 4.
National Cancer Institute’s Community Network Program: Tobacco-Related Policy and Educational Outreach Activities (2005–2009)
| Network number | Policy activities | Educational outreach activities (selected examples) |
|---|---|---|
| 1 | Supported American Cancer Society proposed smokefree workplace legislation | Community health forum presentation, tobacco awareness program, Michigan Cancer Consortium meeting |
| 3 | — | Tobacco workshop for teens, city council meeting, health fair |
| 4 | Supported health center smokefree environmental policy | NAACP Great American Smoke-Out event, Martin Luther King health fair, Death of nicotine skit, high school health and wellness event |
| 5 | — | Freedom from Smoking clinic, Great American Smokeout Day, The 100 Black Men Health Challenge, Health & Wellness Summit |
| 6 | Worked with local and statewide tobacco coalitions, including disparities strategic planning committee. Worked with American Cancer Society to secure $1.5 million to fund youth tobacco control programs. | Kick Butts Day at middle schools, tobacco advocacy training, smoke-free indoor air policy training, Keep Kids Tobacco Free, Hip Hop for Kick Butts Day, Tobacco Free Missouri St Louis annual trivia night |
| 7 | Worked with the South Carolina Cancer Alliance as a partner charged with helping to enact tobacco-free policies | Tobacco education for youth, health fair, cancer education training |
| 8 | — | Native Americans and tobacco use, Cancer 101, Tulalip Tribal health fair and screening |
| 9 | — | Tribal Tobacco Policy Change Summit, Impact of Commercial Tobacco among the Navajos, Urban Indian Tobacco Coalition meeting, “Octopus and Crow” tobacco play at Seattle Folk Life Festival |
| 10 | — | WIC tobacco education program, Great American Smoke Out, American Indian Tobacco Cessation & Health Conference |
| 11 | Supported Cherokee Nation adopting a tobacco-free policy on all tribal properties, except gaming facilities. | Tobacco education class, Students Working Against Tobacco conference, health fairs, Great American Smokeout, World No Tobacco Day in Oklahoma City, quitline marketing |
| 12 | Publication53 showing that smoke-free home rules were associated with California Asian Americans being a former smoker, particularly among recent immigrants, and also lighter smoking. | Smoking and lung cancer awareness among College-aged Filipino students, roundtable on cessation for Chinese and Vietnamese men, Hawaii tobacco summit meeting |
| Publication54 showing that California Chinese and Korean American women with lower education report greater exposure at home or work, despite similar proportions of smoke- free rules at home and work | ||
| 13 | Publication55 showing Chinatown businesses about Philadelphia’s smoking ordinance and determined high general awareness but less knowledge about relevant details. Retail businesses had greater difficulty than restaurants with implementation and enforcement. | Smoking cessation for Chinese, Vietnamese, and Korean smokers; smoking prevention in Chinese, Vietnamese, Korean, and Cambodian community setting (health fairs, organizational gatherings, Smokefree day); tobacco conferences and summit; Smoke-free Asian Youth program (SAY) |
| Worked with City Health Department of Philadelphia and Chinese merchants to adopt No-Smoking Policy at Chinese Business settings | ||
| 14a | — | Dia de la Mujer Latina health fair, Low SES Adult Tobacco Cessation, CO-CNP Latino Cancer Summit |
| 15 | — | Zillah health fair, home health parties, Fiesta Mexicana, community display booths |
| 16 | Supported”Smoke-Free DC” legislation | Ama Tu Vida health fair, Fiesta DC, educational workshop for cancer prevention, radio program |
| 17 | — | Dia de la Mujer Latina Health Festival, Clinical La Raza health fair, senior health fair, Cinco de Mayo fair, cancer education workshop |
| 18 | Collaborated with cancer coalition to pass American Samoa’s first smoke-free law in public and indoor work. | “Men’s Health Awareness Workshop,” community health forum, cancer symposium, advocacy training |
| 19 | Served on Board of Directors and Policy Workgroup for statewide coalition, having previously chaired. Helped state coalition pass smoke-free workplace law, increase state tax on tobacco products, and protect tobacco settlement funds. Authored resolution for a Smoke-free Pacific passed in 2008. Serve on Hawai’i Tobacco Quit Line Advisory Board. | Development and dissemination of materials to promote cessation and support quitting, for example, Internet—www.nativehabit.org, PSA, poster/bus ad, Quit Kit, brochures—“Why You Should Quit Smoking, Medicines to Help You Quit.” Kaua’i Great Smoke Out, tobacco education for youths at risk, Papakolea Community Health Fair. See publication in Results. |
| 20 | — | Aloha Music Series, 17th Ohana Retreat, Marshallese Women’s Group, Chamorro Men’s Outreach, Pacific Islander festival |
| 21 | Developed 4-page policy brief for legislators and community partners describing lung cancer disparities across seven Appalachian states and calling for comprehensive tobacco control. | Smoke-free home and vehicle pledge promotion at Title I Parent Conference, Smoke-free Family days, Smoke-free Baby Bib Project, Smoke-free Restaurant Recognition, Joe Too Cool to Smoke Day in Ohio County, Clean Indoor Air Placemat promotion |
| 22 | — | Clearing the Air for Communities of Color/Cancer Coalition meeting, first anniversary of Smoke-free Workplaces press conference, cancer educational presentation |
| 23 | Supported use of State Cigarette Restitution Fund to implement community- based research on tobacco-related cancers and supporting other organizations addressing health disparities | Tobacco Use Prevention Community Cessation, oral cancer and tobacco presentation to high school students, Symposium for community “Tobacco— The Rest of the Story” |
| 24 | Collaborated with health coalition to develop a city ordinance around tobacco advertisement | Free health clinic, youth disparities initiative, STOMP Out Tobacco Massachusetts People, Fiesta de Salud |
| 25 | — | Black Heritage Festival, Latinos and Cancer Symposium, Health fair |
CNP = Community Networks Program.
aCNP network #2 (Carolina Community Network) did not conduct tobacco-related activities, but instead focused on other cancer control topics. A “—” reflects no reported policy activities.
Domain 1: Understanding Tobacco Use and Related Diseases
Epidemiology
Epidemiology assesses the relationships between tobacco use, behavioral factors, biological/genetic factors, the environment, and disease outcomes in populations.6 Table 2 shows that three CNP networks (#4, 7, 12) had eight publications related to epidemiology in black and Asian American populations. Two of these studies were leveraged partnerships in a statewide and nationwide study.
Several publications demonstrated that blacks had higher tobacco-related cancer and mortality than whites, greater than what would be predicted. CNP #7 led a special journal issue devoted entirely to cancer disparities in South Carolina,71 which demonstrated blacks had higher rates for three tobacco-related malignancies: lung,16 esophagus,11 and oral cavity.17 CNP #718 also showed that the difference between these populations were even greater for cancer mortality than simply incidence. CNP #619 demonstrated higher rates for developing pancreatic cancer and higher risk for mortality.
Three publications showed how concurrent medical conditions and screening were or were not associated with tobacco use and exposure. CNP #4 demonstrated that multiple comorbidities among blacks may not be associated with greater likelihood of quitting, inconsistent with prior literature.15 For Asian Americans, CNP #12 demonstrated that Vietnamese women (who have high rates of cervical cancer, a tobacco-related cancer) did not have higher cervical cancer screening rates for those with home smoke exposure,20 and depressive symptoms were associated with Chinese–American smoking and showed a significant difference by gender.21
Surveillance
While national surveys help monitor trends in tobacco use, they may not report on important intra-ethnic, nativity, and regional variations, especially on smaller population groups.6 Table 2 shows that six CNP networks (#3, 4, 8, 9, 12, 13) had 11 publications related to surveillance for black, American Indian/Alaska Native, and Asian American populations. Three of these studies were leveraged partnerships for regional, statewide, and cross-tribal studies, and two were pilots that examined tobacco use other than cigarettes.
Results from several CNP studies showed high prevalence rates of tobacco use across their populations, particularly lower socioeconomic populations, and within certain subgroups compared with the majority population.22,23,25,28–31 For example, pregnant Alaska Natives had a very high smoking prevalence rate (79%) during and after pregnancy.25
Tobacco use behavior also varied within populations suggesting the interplay of biological and cultural factors. One study of two American Indian tribes, which were culturally and regionally distinct, showed the Northern Plains group had higher cumulative incidence of smoking initiation and earlier ages of initiation than the Southwest group.26 California Asian Americans are lighter smokers than the general population, with these smokers more likely to be women, not Koreans, higher educated, and bilingual with high English proficiency.27 One study described how the South Asian community uses cultural tobacco products (eg, paan, paan masala) but have little knowledge about their health harms.30 Korean smokers in Pennsylvania had few past-year quit attempts despite most having ever tried to quit,32 suggesting they have extenuating barriers. A survey of providers attending a conference on American Indian/Alaska Native health reported mostly asking and assisting about tobacco use,24 which suggests strategies beyond the clinical setting are needed.
Psychosocial Research
Psychosocial research identifies the behavioral, cultural, psychological, and social factors that influence tobacco use behaviors.6 Table 2 shows that seven CNPs (#5, 8, 12, 14, 16, 17, 19) had 14 publications and research activities, over half which were qualitative and conducted among black, American Indian/Alaska Native, Asian American, Latino, and Native Hawaiian and Pacific Islander populations. Three of these studies were leveraged partnerships, and two of these studies were pilot studies examining ethnic subgroups.
Barriers and facilitators of tobacco cessation were similar to previous reports in the general population but also highlighted the population’s perspectives. Providers reported barriers for underserved populations that precluded comprehensive service in clinic.33 Chinese and Vietnamese American men reported stress, low health knowledge, and lack of will-power as barriers,35,37 but support from family and others were facilitators for quitting.35,38 Stress was also associated with smoking initiation among Vietnamese and Filipina American young people.40,41 Rural Native Hawaiian adolescents expressed that smoking was preferable to harder drugs; the latter was perceived as worse for health and society.46
The influence of social networks was a common theme across the CNPs for using tobacco and even conducting research. Friends, family, and community35,38,39,41,45 were important positive and negative influences on initiation, maintenance, and quitting smoking. Alaska Native adolescent tobacco users reported preferences for interventions tailored to their group.34 Social and community networks also facilitated the conduct of research in the community: one pilot found in-person contact was more cost-effective than media to recruit for a tobacco survey,43 and highly mobile Spanish-speaking immigrant smokers were able to participate in intensive assessments and receive tobacco cessation assistance.44
Community-specific beliefs impeding or facilitating cessation are distinct and varied. Chinese smokers believed that giving tobacco as gifts was appropriate and quitting smoking abruptly would lead to new health problems.36 Latino smokers expressed mistrust of pharmacotherapy for cessation.42 Native Hawaiian smokers described religious or spiritual strategies as being helpful for cessation.45
Basic Biology
Basic biology assesses the effects of tobacco and its products on cell biology and cellular mechanisms of action, including the role of initiation and promotion of disease and health effects of exposure to tobacco.6 Table 2 shows that three CNPs had publications and research activities related to black, Alaska Native, and Native Hawaiian populations. One of these studies was a leveraged partnership.
Each CNP demonstrated different novel mechanisms for how tobacco use and disease may be worse for their population. One CNP (#7) helped define a potential mechanism by which mentholated cigarettes, used by many blacks, might lead to higher cancer rates than would be predicted.10,47 Another CNP (#8)48 helped to characterize nicotine addiction and tobacco use in Alaskan Natives, who have high prevalence rates and also use Iqmik an indigenous product. One CNP (#19)49 conducted a pilot study to compare ciliary function between Hawaiians and whites.
Marketing
Marketing examines audience segmentation, distribution patterns, brands, advertisements, promotion, and production of tobacco products.6 Table 2 shows how four CNP (#20, 24, 11, 17) have produced three publications or research activities on marketing for Asian American, Pacific Islander, and underserved populations. All of these were leveraged partnerships.
Two CNPs (#20, 24)50,51 found high rates of tobacco advertising in neighborhoods in two different states. Youth were involved in data collection that used advertisements and one project used Photovoice as a tool. Having youth document the marketing influences in the community environment simultaneously empowered youth to participate in research and incorporated their perspectives.
In a novel collaborative effort, three CNP networks have worked on a large-scale media project (the Tobacco-Related Messages and Media project) to develop tobacco-related messages and exposure measures.52 The development process involved incorporating focus groups perspectives from blacks, American Indians, and Latinos.
Domain 2: Reducing Tobacco Use and Related Diseases
Policy
Policy as a scientific area assesses the effects of policies on tobacco use behaviors and related consequences, tobacco industry practices, tobacco marketing and promotion practices, and initiation.6 We expand the definition here to include CNP participation in the policymaking process, which was encouraged by the CNP model. Table 3 shows that two CNPs (#12, 13) published three papers on policy for the Asian American population.
About half of the CNPs participated in tobacco control policymaking in mainstream efforts that affected their local community and populations. Table 4 shows that 13 CNP networks (#1, 4, 6, 7, 11, 12, 13, 16, 18, 19, 21, 23, 24) reported that their education and information policy activities, often in conjunction with a broader coalition, resulted in decision-makers either changing policies or affecting a change in the policy agenda. Eight CNPs worked on smoke-free policies (#1, 4, 7, 11, 13, 16, 18, 19), three CNPs worked on allocation of funds for tobacco control programs and research (#6, 19, 23), four CNPs educated policymakers on implementing comprehensive tobacco control (#11, 18, 19, 21), and one CNP (#24) worked on a city ordinance for storefront advertising.
Smoke-free policies at home and work were important for Asian American populations, but were challenging to implement and enforce equitably. Smoke-free home rules were associated with quitting, especially for recent immigrants, and lighter smoking.53 However, enforcement may differ among Asian American communities. For example, lower-educated California Chinese and Korean American women reported greater exposure than higher-educated women.54 Chinatown businesses in Philadelphia had a general awareness but difficulty in implementation and enforcement of a smoking ordinance especially for retail businesses.55
Community/State Involvement
This scientific area focuses on the impact and dissemination of single and multiple interventions on the prevention and cessation of tobacco use at the community and state levels.6 Table 3 shows two CNPs (#4, 12)56,57 had leveraged partnerships with the Centers for Disease Control’s Racial and Ethnic Approaches to Community Health projects for black and Asian American and Pacific Islander populations. Each project allowed communities to design strategies based on their identified needs, and promotes capacity building, targeted actions, and community and systems change. Community-based partnerships and strategies were components of these two Racial and Ethnic Approaches to Community Health projects, which were successful in decreasing consumption and uptake in one community,56 and increasing quitting in the other.57
Prevention of Tobacco Use
Prevention of tobacco use identifies and tests interventions designed to prevent the initiation of tobacco use and nicotine addiction.6 We expand the definition here to include tobacco-related education activities in the community, which almost all CNP networks (96%) reported conducting. Table 3 shows one CNP (#9) conducted a pilot study for prevention in the Native American population.58
Educational outreach at community events and schools were important venues for the CNP networks. The CNP conducted a total of 1147 tobacco-related education activities (Year 1: 125, Year 2: 309, Year 3: 429, Year 4: 284).14 Examples of activities that had direct educational involvement with the community (eg, not just media coverage) are featured by CNP in Table 4. Each activity differs broadly in that they may have had a total audience from a few to thousands. The majority of these activities involved outreach at community events like health fairs, and presentations to schools or professional groups. Other activities involve materials distribution and training and technical assistance.
The CNP pilot study58 developed an innovative and interactive supplemental tobacco curriculum for Native American youth in Washington, which already requires tobacco education in schools. The curriculum was developed specifically for Native American youth since prevalence rates remain high, which suggests novel approaches are needed for this population.
Treatment of Nicotine Addiction
Treatment of nicotine dependence identifies, tests, and effectively disseminates interventions to treat tobacco users.6 Table 3 shows how seven CNPs (#5, 8, 13, 15, 17, 19, 21) produced eight publications or research activities on treatment of nicotine addiction for black, American Indian/Alaska Native, Asian American, Latino, Native Hawaiian, and Underserved populations. Two of the interventions were leveraged partnerships and two were pilot studies.
The CNP networks’ tobacco cessation interventions were diverse in how they were culturally and linguistically targeted to the CNP populations, partnered with other organizations, and also how they targeted different levels of health—from the smoker to provider to health systems. Cultural and linguistic tailoring was described at least for interventions targeting American Indian/Alaska Natives,14 Asian Americans,60,61 Latinos,63 and Native Hawaiians.64 Three CNPs partnered with other organizations to promote tobacco treatment within their communities: American Indian/Alaska Native, Latinos, and Underserved in rural Pennsylvania.14,62,65 Four CNPs published evaluations of tobacco treatment interventions: two focused on intervening at the provider/health system level,59,64 one implemented a large internet trial,63 and one created culturally adapted community-based cessation programs.60,61
Countermarketing
Countermarketing reflects the opposing efforts (eg, campaigns) against tobacco industry marketing influence that may involve audience segmentation, distribution patterns, brands, advertisements, promotion, and production of tobacco products.6 Table 3 shows one of CNP 19’s community partners has been the lead in counter-marketing efforts in Hawaii: “REAL,” Hawaii’s youth-led movement with more than 4000 young people members, aims to increase youth advocacy and reduce the industry’s influence over youth.8 One example of REAL’s countermarketing campaign reversed the messaging of a “Share the Love” free cigarette coupon, by instead encouraging youth to use the message to educate the community about the tobacco industry’s tactics and support quitting.
Domain 3: Research Capacity and Infrastructure
This overarching domain ensures the availability of necessary human, financial, and technological resources; systems for collaboration; and mechanisms for information dissemination feedback to provide a strong foundation for research and public health initiatives.6 We describe the CNP pilots here, because training of junior investigators from minority and underrepresented groups are considered important human resources for future research. We also describe the leveraged partnerships, which were encouraged by the CNP model, as important sources for collaboration, shared resources, sustainability.
Table 3 shows one publication66 from two CNP (#11, 17) that developed a community-specific conceptual framework for building capacity for tobacco control with case studies of two ethnic communities. The two communities were American Indians in Oklahoma and the Hispanic/Latino Tobacco Education Partnership organizations in California. Capacity building not only required resources, infrastructure, and development, but also an underlying understanding of community strengths, history, values, and participation.
Table 3 shows five publications8,67–70 demonstrating how CNP #19 has been involved over many years with building research capacity and infrastructure for Native Hawaiians. A socioecological approach incorporates Native Hawaiian data, culture, and institutions for a sustainable program.68 Two 5-year strategic plans (2005–201070, 2011–20168) for tobacco prevention and control in Hawaii were developed through an intensive community process involving hundreds of individuals and organizations. A Community Readiness Model67 helped assess and demonstrate gaps for each Native Hawaiian Health Care System, which led to the collaboration with CNP #19 for systems change in addressing tobacco cessation. Other infrastructure developments include statewide survey data incorporating Native Hawaiian data8 and a Native Hawaiian Institutional Review Board administered by CNP #19’s parent organization.69
Pilots
As described above, the CNPs were encouraged to develop and implement pilot studies of community-based participatory research and train young investigators. The nine tobacco-related pilot projects 23,38,41,43,44,49,58,61,63 (Table 3) interestingly reflected each CNP population groups among eight different CNPs, with three pilots that targeted Asian Americans and two pilots that targeted Latinos. Under the domain of understanding tobacco use and related diseases, there were pilots that addressed Surveillance (1), Psychosocial Research (4), and Basic Biology (1). Under the domain of reducing tobacco use and related diseases, there were pilots that addressed Prevention of Tobacco Use (1) and Treatment of Nicotine Addiction (2). Common themes included targeting monolingual immigrants (4), youth and young adult populations (3), tailored curriculum or program development (3), and tobacco products other than cigarettes (2). Novel themes included addressing secondhand smoke concerns for cessation, cost-effectiveness for proactive versus reactive recruitment strategies, intensive assessment of behavior around a quit date, and comparing ciliary function as a risk factor for differences in lung cancer incidence.
Leveraged Partnerships
Leveraged partnerships noted in Tables 2 and 3 reflect statewide and nationwide funding organizations and/or data sources for projects in which CNP authors collaborated. Nationwide resources include Racial and Ethnic Approaches to Community Health projects funded by the Centers for Disease Control and Prevention,15,22,56,57 American Cancer Society’s Cancer Prevention Study II,19 tribal sources,26 American Legacy Foundation,52,68 Asian Pacific Partners for Empowerment Advocacy and Leadership,67 NCI’s Cancer Information Service Partnership Program,65 and other National Institutes of Health funding organizations.48 Statewide resources include the California Tobacco Control Program’s ethnic surveys,28 the California Tobacco-Related Disease Research Program,30,50,63 and the Massachusetts Tobacco Control Program.51
This list of partnerships is not comprehensive as other types of partnerships with resources other than acknowledged funding may not be reflected. Such partnerships may include community coalitions and clinical partnerships. For example, CNP #7 determined alcohol as a significant cofactor for carcinogenicity, after community discussions explored the potential etiologies for the disproportionately higher rates of tobacco-related cancer within blacks.47 CNP #21 collaborated with a cancer coalition, as well as the NCI Cancer Information Service, to develop their smokeless tobacco cessation program for rural Pennsylvanians.65 CNP #19 collaborated with five operationally-independent Native Hawaiian Health Care Systems on a systemwide intervention on tobacco cessation.64 Such partnerships with community members and resources may facilitate generation of ideas, recruitment, participation, and dissemination.
Discussion
The purpose of this study was to describe the CNP model and the CNP networks’ tobacco-related work in community-based research, education, and training using a tobacco disparities research framework. Our review of documents from the NCI’s CNP shows that the CNP is a promising model for engaging the community on tobacco-related health disparities. The flexibility of the CNP model allowed networks to design and implement strategies to reflect the specific context and conditions of the targeted communities. Even though tobacco as a topic was not mandated by the CNP, almost all CNP networks conducted tobacco-related activities and contributed to a diverse range of scientific areas identified in the tobacco disparities framework. Publications on tobacco reflect the highest proportion of CNP cancer-related publications. Almost all CNP networks conducted educational outreach within their community, and about half were engaged in policy-related activities. Pilot studies helped train new investigators on CBPR from networks representing each of the CNP populations. Leveraged partnerships reflect a broad range of local, state, and national partners and funders.
Using the scientific tobacco disparities framework, the CNP network activities were the most numerous and representative of the CNP populations in four scientific areas: “Psychosocial Research,” “Surveillance,” “Epidemiology,” and “Treatment of Nicotine Addiction.” The significance of this must be viewed with caution since the contribution of the CNP cannot be evaluated traditionally, such as with a systematic review, due to the diversity of causes and circumstances related to cancer health disparities across population groups. Furthermore, the CNP selected cancer topics based on the needs and interests of their population group, and it is difficult to rate the impact of this work here because there may be different valuations assigned by communities and researchers.
We did not identify CNP activities or publications in the “Harm Reduction” scientific area of the framework. However, we expect that harm reduction may become more relevant as the use of electronic cigarettes, flavored tobacco products, including menthol, increases in minorities and underserved communities. Smokeless tobacco products, which have been examined by CNP 8,48 and the harm of menthol, as demonstrated by CNP 7,10 have been topics of debate about harm reduction.
The need for addressing novel lines of investigation in other scientific areas of the tobacco disparities framework with more CNP networks, population subgroups, and communities is important. For example in “Epidemiology”, with the human genome available for analysis, there has been a rise in publications on genetic differences in relation to tobacco dependence.72 Fernander73 states it is critical that investigators proceed with caution in examining the association between genetics and tobacco-related health disparities, and that it is critical to use trans-disciplinary approaches, particularly because groups classified by race, a social construct, may need special interpretations. CNP 8 could be considered a model for CBPR by having the community participate at all phases of the research on nicotine metabolism in Alaska Natives and also ensuring that the work will benefit the community.74 For “Basic Biology,” there may be important mechanisms underlying differences in how populations express different risk profiles. Also, differences in effect per unit exposure calls into question the possibility of intrinsic (ie, biological) disparities in response75–78 and that other factors, such as diet and type of alcoholic beverages consumed, may influence risk.79,80
In the future, CNPs might be encouraged to collaborate more on common projects and topics. Two current examples include the Tobacco-Related Media and Messages project that includes perspectives across three CNPs52 and the community-specific conceptual framework for building capacity for tobacco control that had case studies from two CNPs.66 One such future topic may be on light and intermittent smoking. As demonstrated in the literature27,42 and in national guidelines,81 racial and ethnic minorities are disproportionately represented as light and intermittent smokers. This implies that a greater understanding from a biological and community/cultural perspective will be needed to treat individuals who demonstrate this behavior. Resources are limited and this collaborative approach encourages cross-fertilization, builds research capacity, and maximizes synergy without creating competing agendas.
While beneficial in many ways, the diversity of the CNPs also poses a limitation in evaluating its collective contribution. The CNP networks have collected a wide range of tobacco-related data and information, with varying conceptual frameworks, operational definitions, and end points. Tobacco-related scientific activities that involved, or were influenced by, the CNPs may not have been included or measured here due to the limitations of reporting by number of publications or formal activities. There have not yet been common factors established to measure success across networks, nor can findings be generalized across all networks or outside of the immediate network pool. To address this issue, the CNP leadership is collaborating with a project by the Indian Health Service to develop a set of core variables and measures (eg, tobacco use behavior, health consequences, capacity) that may help assess and evaluate tobacco-related health disparities across racial/ethnic and underserved populations. This is an important first step in tracking progress. In the future, these measures might be enhanced by making them available in an interactive platform in which CNP networks, communities, and other collaborating organizations could share ideas and progress, even across scientific areas or population groups. In the future, CNPs also might consider assessing the extent to which their projects operationalize CBPR principles.
While it is difficult to assess the extent the CNP model actually reduced disparities in communities, we do believe that the findings have implications for reducing disparities. For example, the CNP networks have shown how members of their population groups have higher rates of use and disease than the general population, with variation by gender, socioeconomic status, and acculturation. Thus, aggregate data may not always reflect disparities, and special efforts or surveys may need to continue targeting certain population groups not reflected in the mainstream. The CNP findings from qualitative research among different ethnic groups provide additional information on family, cultural, and psychosocial factors that are barriers and facilitators of tobacco use. For treating tobacco dependence, cultural adaptation may be useful for cessation programs, especially in targeting Asian ethnic groups. Training among providers, youth, and other community members may be helpful for building capacity to conduct evidence-based treatment programs. Similarly, training junior investigators and partnering with other organizations and communities builds capacity and synergy to conduct community-based research. Community and state strategies that focus on specific ethnic groups may be useful for increasing quit rates among Asian ethnic groups, but may need refinement for blacks.
Overall, the CNP has collectively contributed towards building the evidence in many scientific areas critical to eliminating tobacco-related health disparities. While we have made attempts to be comprehensive and systematic in the review of tobacco-related activities within the CNP, it is possible that the team overlooked relevant activities or publications; and many are being expanded and enhanced in the next phase, that is, Community Network Program Centers. The collaborative CNP approach is a promising mechanism, not just for working towards eliminating tobacco-related health disparities, but it also holds promise in the application of CBPR principles to address other health-related disparities and advance our understanding of improving health across disciplines and cultures. As the Healthy People 2020 expands its goal from eliminating disparities to achieving health equity and improving the health for all groups,82 comprehensive interventions to address social and structural inequalities and advancing evaluation methods are needed.83
Funding
This work was supported by the National Cancer Institute’s Center to Reduce Cancer Health Disparities with the Cooperative Agreement, Community Networks To Reduce Cancer Health Disparities (RFA-CA-05-012), including the specific contributions of: U01 CA114601 (South Carolina Cancer Disparities Community Network, PI: JRH); U01 CA114640 (Asian American Network for Cancer Awareness, Research and Training, PI: M. Chen); U01 CA114582 (ATECAR—Asian Community Cancer Network, PI: GXM); U01 CA114630 (‘Imi Hale Native Hawaiian Cancer Network, PI: C. Chong); U01CA86117 (Redes en Acción, PI: A. G. Ramirez); U01CA114619 (Deep South Network for Cancer Control, PI: Edward E. Partridge).
Declaration of Interests
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health/National Cancer Institute. The authors have no conflicts or disclosures.
Supplementary Material
References
- 1. Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116(3):544–573. 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services. Tobacco Use Among U.S. Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- 3. Fagan P, Moolchan E, Lawrence D, Fernander A, Ponder P. Identifying health disparities across the tobacco continuum. Addiction. 2007;102(suppl 2):5–29. 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- 4. Moolchan ET, Fagan P, Fernander AF, et al. Addressing tobacco-related health disparities. Addiction. 2007;102(suppl 2):30–42. 10.1111/j.1360-0443.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- 5. US Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 6. Fagan P, King G, Lawrence D, et al. Eliminating tobacco-related health disparities: directions for future research. Am J Public Health. 2004;94(2):211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults–United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–1112. [PMC free article] [PubMed] [Google Scholar]
- 8. Hawai’i State Department of Health, Tobacco Prevention and Control Trust Fund Advisory Board, Coalition for a Tobacco-Free Hawai’i. Tobacco Use Prevention & Control in Hawai’i: A Strategic Plan for the State 2011–2016 2011. http://health.hawaii.gov/tobacco/files/2013/06/DOH_TobaccoFull2011.pdf Accessed January 10, 2015.
- 9. Hébert J. Invited commentary: menthol cigarettes and risk of lung cancer. Am J Epidemiol. 2003;158(7):617–620. [DOI] [PubMed] [Google Scholar]
- 10. Azzi C, Zhang J, Purdon CH, et al. Permeation and reservoir formation of 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and benzo[a]pyrene (B[a]P) across porcine esophageal tissue in the presence of ethanol and menthol. Carcinogenesis. 2006;27(1):137–145. [DOI] [PubMed] [Google Scholar]
- 11. Hebert JR, Adams SA, Daguise VG, et al. Esophageal cancer disparities in South Carolina: early detection, special programs, and descriptive epidemiology. J South Carolina Med Assoc. 2006;102(7):201–209. [PubMed] [Google Scholar]
- 12. Center for Program Evaluation and Performance Assessment. Developing and Working with Program Logic Models 2014. www.bja.gov/evaluation/guide/pe4.htm Accessed April 1, 2014.
- 13. Braun KL, Nguyen TT, Tanjasiri SP, et al. Operationalization of community-based participatory research principles: assessment of the national cancer institute’s community network programs. Am J Public Health. 2012;102(6):1195–1203. 10.2105/AJPH.2011.300304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. CSR Incorporated. National Evaluation of the Community Networks Program To Reduce Cancer Health Disparities through Education, Research, and Training: Annual Report for Year 4 (Submitted to National Cancer Institute’s Center for Reducing Cancer Health Disparities.). 2010. [Google Scholar]
- 15. Patel K, Schlundt D, Larson C, Wang H, Brown A, Hargreaves M. Chronic illness and smoking cessation. Nicotine Tob Res. 2009;11(8):933–939. 10.1093/ntr/ntp088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alberg AJ, Horner MJD, Daguise VG, et al. Lung and bronchus cancer disparities in South Carolina: epidemiology and strategies for prevention. J South Carolina Med Assoc. 2006;102(7):183–191. [PubMed] [Google Scholar]
- 17. Yen KL, Horner MJD, Reed SG, et al. Head and neck cancer disparities in South Carolina: descriptive epidemiology, early detection, and special programs. J South Carolina Med Assoc. 2006;102(7):192–200. [PubMed] [Google Scholar]
- 18. Hébert JR, Daguise VG, Hurley DM, et al. Mapping cancer mortality-to-incidence ratios to illustrate racial and sex disparities in a high-risk population. Cancer. 2009;115(11):2539–2552. 10.1002/cncr.24270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Arnold L, Patel A, Yan Y, et al. Are racial disparities in pancreatic cancer explained by smoking and overweight/obesity? Cancer Epidemiol Biomarkers Prev. 2009;18(9):2397–2405. 10.1158/1055–9965.EPI-09-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chan N, Yasui Y, Thompson B, et al. Secondhand smoke in the home and Pap testing among Vietnamese American women. Asian Pac J Cancer Prev. 2007;8(2):178–182. [PubMed] [Google Scholar]
- 21. Luk J, Tsoh J. Moderation of gender on smoking and depression in Chinese Americans. Addict Behav. 2010;35(11)1040–1043. 10.1016/j.addbeh.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schlundt D, Niebler S, Brown A, et al. Disparities in smoking: data from the Nashville REACH 2010 project. J Ambul Care Manage. 2007;30(2):150–158. 10.1097/01.JAC.0000264605.42500.d9. [DOI] [PubMed] [Google Scholar]
- 23. Carroll WR, Foushee HR, Hardy CM, Floyd T, Sinclair CF, Scarinci I. Tobacco use among rural African American young adult males. Otolaryngol Head Neck Surg. 2011;145(2)259–263. 10.1177/0194599811404968. [DOI] [PubMed] [Google Scholar]
- 24. Packer MM, Kaur JS, Hodge FS, Nan B, Trapp MA, Roubidoux MA. A survey of attendees at Native American health care conferences: knowledge, attitudes, and practices about cigarette smoking. J Cancer Educ. 2005;20(2):89–95. 10.1207/s15430154jce2002_9. [DOI] [PubMed] [Google Scholar]
- 25. Patten C, Renner C, Decker P, et al. Tobacco use and cessation among pregnant Alaska Natives from Western Alaska enrolled in the WIC program, 2001–2002. Matern Child Health J. 2008;12(suppl 1):30–36. 10.1007/s10995-008-0331-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nez Henderson P, Kanekar S, Wen Y, et al. Patterns of cigarette smoking initiation in two culturally distinct American Indian tribes. Am J Public Health. 2009;99(11):2020–2025. 10.2105/AJPH.2008.155473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tong E, Nguyen T, Vittinghoff E, Pérez-Stable E. Light and intermittent smoking among California’s Asian Americans. Nicotine Tob Res. 2009;11(2):197–202. 10.1093/ntr/ntp013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tong E, Gildengorin G, Nguyen T, et al. Smoking prevalence and factors associated with smoking status among Vietnamese in California. Nicotine Tob Res. 2010;12(6):613–621. 10.1093/ntr/ntq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chan N, Thompson B, Taylor V, et al. Smoking prevalence, knowledge, and attitudes among a population of Vietnamese American men. Nicotine Tob Res. 2007;9(suppl 3):S475–484. 10.1080/14622200701587086. [DOI] [PubMed] [Google Scholar]
- 30. Mukherjea A, Morgan PA, Snowden LR, Ling PM, Ivey SL. Social and cultural influences on tobacco-related health disparities among South Asians in the USA. Tob Control. 2011;21(4)422–428. 10.1136/tc.2010.042309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ma G, Shive S, Tan Y, Toubbeh J, Fang C, Edwards R. Tobacco use, secondhand smoke exposure and their related knowledge, attitudes and behaviors among Asian Americans. Addict Behav. 2005;30(4):725–740. 10.1016/j.addbeh.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 32. Ma G, Fang C, Knauer C, Tan Y, Shive S. Tobacco dependence, risk perceptions and self-efficacy among Korean American smokers. Addict Behav. 2006;31(10):1776–1784. 10.1016/j.addbeh.2005.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Blumenthal D. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med. 2007;20(3):272–279. 10.3122/jabfm.2007.03.060115. [DOI] [PubMed] [Google Scholar]
- 34. Patten C, Enoch C, Renner C, et al. Focus groups of Alaska Native adolescent tobacco users: preferences for tobacco cessation interventions and barriers to participation. Health Educ Behav. 2009;36(4):711–723. 10.1177/1090198107309456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Spigner C, Shigaki A, Tu SP. Perceptions of Asian American men about tobacco cigarette consumption: a social learning theory framework. J Immigr Health. 2005;7(4):293–303. [DOI] [PubMed] [Google Scholar]
- 36. Hu K, Woodall E, Do H, et al. Tobacco knowledge and beliefs in Chinese American men. Asian Pac J Cancer Prev. 2006;7(3):434–438. [PubMed] [Google Scholar]
- 37. Spigner C, Yip M, Huang B, Tu S. Chinese and Vietnamese adult male smokers’ perspectives regarding facilitators of tobacco cessation behavior. Asian Pac J Cancer Prev. 2007;8(3):429–435. [PubMed] [Google Scholar]
- 38. Tong E, Paterniti D, Fung L, Tsoh J, Chen M. Developing a Secondhand Smoke Counseling Intervention for Chinese Smokers and Nonsmokers. In: National Conference on Tobacco or Health; June 2009; Phoenix, AZ. [Google Scholar]
- 39. Kaplan C, Nguyen T, Weinberg V. Longitudinal study of smoking progression in Chinese and Vietnamese American adolescents. Asian Pac J Cancer Prev. 2008;9(2):335–341. [PubMed] [Google Scholar]
- 40. Ling P, Neilands T, Nguyen T, Kaplan C. Psychographic segments based on attitudes about smoking and lifestyle among Vietnamese-American adolescents. J Adolesc Health. 2007;41(1):51–60. 10.1016/j.jadohealth.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 41. Sy A, Duquez E, Braun K. Using Community-based Research Methods to Explore High Smoking Prevalence in Filipina Girls. American Public Health Association Annual Meeting; 2009; Philadelphia, PA. [Google Scholar]
- 42. Levinson A, Borrayo E, Espinoza P, Flores E, Pérez-Stable E. An exploration of Latino smokers and the use of pharmaceutical aids. Am J Prev Med. 2006;31(2):167–171. S0749379703003222. [DOI] [PubMed] [Google Scholar]
- 43. Graham AL, Lopez-Class M, Mueller NT, Mota G, Mandelblatt J. Efficiency and cost-effectiveness of recruitment methods for male Latino smokers. Health Educ Behav. 2011;38(3):293–300. 10.1177/1090198110372879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Haverlah K. Re: “Ecological Momentary Assessment of Smoking Cessation in Spanish-Speaking Smokers”. Carlos Mazas Pilot Study Ed; 2010. [Google Scholar]
- 45. Kaholokula J, Braun K, Santos J, Chang H. Culturally informed smoking cessation strategies for Native Hawaiians. Nicotine Tob Res. 2008;10(4):671–681. 10.1080114622200801978763. [DOI] [PubMed] [Google Scholar]
- 46. Else I, Goebert D, Nishimura S, Braun K. Smoking is the least of our problems: focus group findings from Native Hawaiian youth. Huili: Multidisciplinary Research on Hawaiian Well-Being. 2008;5:287–314. [Google Scholar]
- 47. Hébert JR, Brandt HM, Armstead CA, Adams SA, Steck SE. Interdisciplinary, translational, and community-based participatory research: finding a common language to improve cancer research. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1213–1217. 10.1158/1055-9965.EPI-08-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhu AZ, Binnington MJ, Renner CC, et al. Alaska Native smokers and smokeless tobacco users with slower CYP2A6 activity have lower tobacco consumption, lower tobacco-specific nitrosamine exposure and lower tobacco-specific nitrosamine bioactivation. Carcinogenesis. 2013;34(1):93–101. 10.1093/carcin/bgs306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gellert KS, Choi D, Coel M, Braun KL. A feasibility study of methodology for recruitment and for comparative testing of ciliary function in Hawaiians and Caucasians. Hawaii Med J. 2008;67(8):209–212. [PubMed] [Google Scholar]
- 50. Tanjasiri SP, Lew R, Kuratani DG, Wong M, Fu L. Using Photovoice to assess and promote environmental approaches to tobacco control in AAPI communities. Health Promot Pract. 2011;12(5):654–665. 10.1080/08858190701821386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Crisostomo J. Re: MassCONECT tobacco-related activities. Electronic mail. 2010. [Google Scholar]
- 52. Vallone D, Beebe L, Wallington S, Viswanath V, Flaherty B, Niederdeppe J. Developing a Tobacco Exposure to Media and Marketing Index (TERMM). Paper presented at: Making the Difference in Tobacco-related Health Disparities Science: TReND Progress, Process, and Opportunities for Future Investment; 2010; Bethesda, MD. [Google Scholar]
- 53. Tong E, Nguyen T, Vittinghoff E, Pérez-Stable E. Smoking behaviors among immigrant Asian Americans: rules for smoke-free homes. Am J Prev Med. 2008;35(1):64–67. 10.1016/j.amepre.2008.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tong E, Tang H, Tsoh J, Wong C, Chen MJ. Smoke-free policies among Asian-American women: comparisons by education status. Am J Prev Med. 2009;37(suppl 2):S144–S150. 10.1016/j.amepre.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ma G, Poon A, Toubbeh J. Diffusion of Philadelphia’s No-Smoking Policy to Chinese Businesses. Am J Health Stud. 2008;23(4):162–172. [PMC free article] [PubMed] [Google Scholar]
- 56. Larson C, Schlundt D, Patel K, Wang H, Beard K, Hargreaves M. Trends in smoking among African-Americans: a description of Nashville’s REACH 2010 initiative. J Community Health. 2009;34(4):311–320. 10.1007/s10900-009-9154-8. [DOI] [PubMed] [Google Scholar]
- 57. Liao Y, Tsoh J, Chen R, et al. Decreases in smoking prevalence in Asian communities served by the Racial and Ethnic Approaches to Community Health (REACH) project. Am J Public Health. 2010;100(5):853–860. 10.2105/AJPH.2009.176834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gibbons R. An innovative and Interactive Supplemental Tobacco Curriculum for Native Youth.
- 59. Caplan L, Stout C, Blumenthal DS. Training physicians to do office-based smoking cessation increases adherence to PHS guidelines. J Community Health. 2011;36(2):238–243. 10.1007/s10900-010-9303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fang C, Ma G, Miller S, Tan Y, Su X, Shive S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43(4):321–324. 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 61. Wu D, Ma G, Zhou K, Zhou D, Liu A, Poon A. The effect of a culturally tailored smoking cessation for Chinese American smokers. Nicotine Tob Res. 2009;11(12):1448–1457. 10.1093/ntr/ntp159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Thompson B. Re: “Quit and Win” contests. Electronic mail. 2010. [Google Scholar]
- 63. Muñoz R, Barrera A, Delucchi K, Penilla C, Torres L, Pérez-Stable E. International Spanish/English Internet smoking cessation trial yields 20% abstinence rates at 1 year. Nicotine Tob Res. 2009;11(9):1025–1034. 10.1093/ntr/ntp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Santos L, Braun K, Ae’a K, Shearer L. Institutionalizing a comprehensive tobacco-cessation protocol in an indigenous health system: lessons learned. Prog Community Health Partnersh. 2008;2(4):279–289. 10.1353/cpr.0.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cushman M. An Adaptation of a Self-Help Smokeless Tobacco Cessation Program. 5th National Summit on Smokeless & Spit Tobacco; September 22, 2009; Madison, WI. [Google Scholar]
- 66. Báezconde-Garbanati L, Beebe L, Pérez-Stable E. Building capacity to address tobacco-related disparities among American Indian and Hispanic/Latino communities: conceptual and systemic considerations. Addiction. 2007;102(suppl 2):112–122. 10.1111/j.1360-0443.2007.01962.x. [DOI] [PubMed] [Google Scholar]
- 67. Asian Pacific Partners for Empowerment Advocacy and Leadership. Implementing a Community Readiness Approach to Tobacco Control Oakland, CA; APPEAL: 2006. www.appealforcommunities.org/wp-content/uploads/2014/06/2198_Casestudyfinal.reviseHI.pdf Accessed January 10, 2015. [Google Scholar]
- 68. American Legacy Foundation. Sustainability Beyond Dollars: Organizations Achieving Long-Term Success in Community-Based Tobacco Control 2008. www.legacyforhealth.org/content/download/713/8126/version/1/file/Sustainability_Beyond_Dollars__Organizations---_Achieving_Long-Term_Success_in_Community-Based_Tobacco_Control.pdf Accessed January 10, 2015.
- 69. ‘Imi Hale Native Hawaiian Cancer Network. ‘Imi Hale: Research. ‘Imi Hale research projects are approved by the appropriate institution IRBs including the Native Hawaiian IRB adminstrated by Papa Ola Lokahi, 894 Queen Street, Honolulu HI 2013. www.imihale.org/research.htm Accessed January 10, 2015.
- 70. Coalition for a Tobacco-Free Hawai’i, Hawai’i State Department of Health, Tobacco Prevention and Control Trust Fund. Tobacco Use Prevention & Control in Hawai’i: A 5 Year Strategic Plan for the State 2006. www.hawaiitobaccocontrol.org/sites/default/files/resource/strategicplanning_hawaii_tobacco.pdf Accessed January 10, 2015.
- 71. Hébert JR, Elder K, Ureda JR. Meeting the challenges of cancer prevention and control in South Carolina: focusing on seven cancer sites, engaging partners. J South Carolina Med Assoc. 2006;102(7):177–182. [PubMed] [Google Scholar]
- 72. Amos C, Spitz M, Cinciripini P. Chipping away at the genetics of smoking behavior. Nat Genet. 2010;42(5):366–368. 10.1038/ng0510-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Fernander A. Racially classified social group tobacco-related health disparities: what is the role of genetics? Addiction. 2007;102(suppl s2):58–64. 10.1111/j.1360-0443.2007.01955.x. [DOI] [PubMed] [Google Scholar]
- 74. Kaur J. Re: Nicotine Exposure and Metabolism study. Electronic mail. 2010. [Google Scholar]
- 75. Hebert JR. Differences in biological responses to cigarette smoking remain unexplained. Am J Public Health. 1991;81(12):1679–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Muscat JE, Djordjevic MV, Colosimo S, Stellman SD, Richie JP. Racial differences in exposure and glucuronidation of the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK). Cancer. 2005;103(7):1420–1426. [DOI] [PubMed] [Google Scholar]
- 77. Richie JP, Carmella SG, Muscat JE, Scott DG, Akerkar SA, Hecht SS. Differences in the urinary metabolites of the tobacco-specific lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in black and white smokers. Cancer Epidemiol Biomarkers Prev. 1997;6(10):783–790. [PubMed] [Google Scholar]
- 78. Brown LM, Hoover RN, Greenberg RS, et al. Are racial differences in squamous cell esophageal cancer explained by alcohol and tobacco use? J Natl Cancer Inst. 1994;86(17):1340–1345. [DOI] [PubMed] [Google Scholar]
- 79. Le Marchand L, Yoshizawa CN, Kolonel LN, Hankin JH, Goodman MT. Vegetable consumption and lung cancer risk: a population-based case-control study in Hawaii. J Natl Cancer Inst. 1989;81(15):1158–1164. [DOI] [PubMed] [Google Scholar]
- 80. Baden E. Prevention of cancer of the oral cavity and pharynx. CA Cancer J Clin. 1987;37(1):49–62. [DOI] [PubMed] [Google Scholar]
- 81. Fiore M, Jaen C, Baker T, et al. Treating Tobacco Use and Dependence: 2008 Update—Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 82. Healthy People 2020. Foundation Health Measures: Disparities www.healthypeople.gov/2020/about/foundation-health-measures/Disparities Accessed January 5, 2015.
- 83. Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32:399–416. 10.1146/annurev-publhealth-031210-101136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


