Abstract
This report describes a young pregnant woman who presented to a rural emergency department with vaginal bleeding at 7 weeks of gestation. Initially, the patient was stable; however, within 8 h the patient deteriorated into fulminant septic shock. She required aggressive resuscitation and surgical management of a septic abortion. The patient's condition improved rapidly following surgical evacuation of the uterus with dilatation and curettage. She has had no long-term sequelae. Blood and tissue cultures returned positive for Clostridium septicum. To the best of our knowledge, this is the only reported case of survival from C septicum infection in a pregnant woman and highlights the importance of improved awareness and management of such infections by the medical community so that future cases can achieve similarly successful outcomes.
Background
To date, there have been no reports of survival in the literature describing Clostridium septicum sepsis in pregnant women. C septicum sepsis is rare but associated with an extremely high death rate of at least 80% without appropriate treatment.1 2 Reports suggest an occurrence rate of 0.5–2.0% in overall blood culture isolates, with Clostridium perfringens being the most commonly isolated species.3 C septicum is even less commonly isolated but should be known to the medical community caring for susceptible individuals, including pregnant women. The incubation period is rapid (<24 h), necessitating prudent identification of the early signs of infection so that life-saving treatment can be provided.1 Immediate treatment with broad-based, intravenous antibiotics and removal of the nidus of infection is considered to be most effective in managing morbidity and preventing death in patients with C septicum infections.
Case presentation
A 21-year-old Gravida 1 Para 0 female patient presented to a rural emergency department with abdominal pain and heavy bleeding at 7 weeks of gestation. Her medical history was significant for asthma and possible IgA deficiency. On initial presentation, the patient was presyncopal, hypotensive (90/58 mm Hg) and mildly tachycardic (90 bpm). Her haematological profile was normal (haemoglobin 146 g/l, platelets 170 × 109/l, international normalised ratio 1.1) except for her leuoccyte count, which was mildly elevated (13.6 × 109/l). The patient was administered a fluid bolus and transferred to our regional hospital for a gynaecological consultation. A diagnosis of a spontaneous abortion versus ectopic pregnancy was entertained.
On arrival at our centre, the patient's haemoglobin dropped to 135 g/l. Physical examination revealed a closed external os, no active bleeding, no marked cervical motion tenderness or peritoneal irritation. A bedside abdominal and pelvic ultrasound demonstrated a single intrauterine pregnancy measuring with a gestational size of 7 weeks with a fetal pole and heart motion. No obvious subchorionic haemorrhage or other cause for antepartum bleeding was identified. Her abdominal pain improved after catheterisation. The patient was admitted for observation with a diagnosis of a threatened abortion.
The patient was closely monitored and 8 h after admission the patient became febrile (39.4 °C), profoundly hypotensive (70/44 mm Hg) and tachycardic (110 bpm). On examination, the patient had complaints of severe generalised abdominal and joint pain although there was no rebound tenderness, guarding, ascites or skin change. She had minimal vaginal bleeding.
Investigations
Urine cultures were drawn and sent for analysis.
Differential diagnosis
The patient's rapid deterioration was consistent with systemic shock, with haemorrhagic or septic shock being the most likely precipitant. Incomplete abortion and aberrant pregnancy, such as a ruptured cornual pregnancy, are possible causes of haemorrhagic shock in pregnant women; however, the abdominal and pelvic ultrasound performed on initial presentation did not reveal evidence of such abnormalities. Septic abortion due to septic shock was more likely, given her vital signs, elevated leucocyte count and no obvious source of bleeding. A non-pregnancy-related cause such as urosepsis was considered; however, the clinical context was most suggestive of a gynaecological source of infection. Preparations for surgical evacuation of the uterus were therefore made.
Treatment
Management of sepsis and septic shock was initiated and this was in accordance with the 2008 International Guidelines for Management of Severe Sepsis and Septic Shock.4 The patient was promptly given 4 litres of crystalloid and blood and intravenous clindamycin 900 mg and gentamicin 5 mg/kg. On consultation with an intensivist, broader coverage with intravenous pipercillin–tazobactam 4 g/0.5 g was subsequently administered for management of septic shock secondary to a septic abortion. The decision was made to proceed with emergency dilatation and curettage (D&C) to remove the nidus of infection and the patient's condition improved following surgery.
Intravenous antibiotics were stopped after the patient was afebrile for 48 h and she was discharged with recommended treatment of oral amoxil–clavulanic acid 875 mg/125 mg for 10 days.
Outcome and follow-up
Blood and tissue cultures from the D&C returned positive for C septicum. On histopathology, groups of rod-like bacteria could be seen intermixed with chorionic villi and decidua (figure 1).
Figure 1.
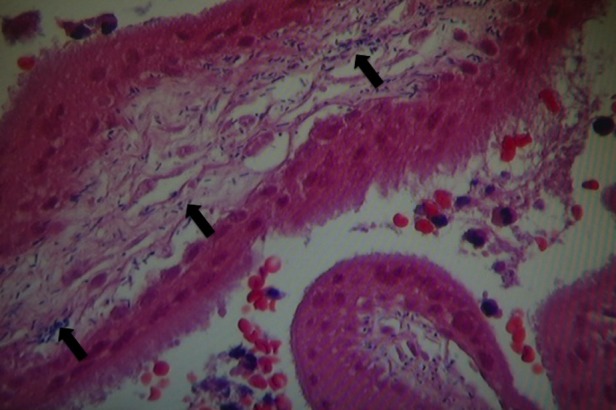
Low power image of gram-stained curettage products showing gram-positive rods of Clostridium septicum (arrows) surrounding chorionic villi.
The patient returned to the emergency department 4 days later with left flank pain, uterine tenderness and cervical motion tenderness. She had been on amoxil–clavulanic acid for 48 h.
Her vitals and temperature were normal, she had no peritoneal or rebound tenderness and the transabdominal and endovaginal scans did not reveal any retained products of conception. The patient spent a night in hospital and was discharged with intravenous pipercillin–tazobactam 4 g/0.5 g for 7 days.
The patient is fortunate to have survived and she remains well with no long-term sequelae 15 months after operation.
Discussion
Clostridial bacteraemia is an unusual but serious condition affecting the general population. C septicum, a rare species, is a gram-positive, gas-forming anaerobic bacterium demonstrating an incubation time of less than 24 h with rapid systemic spread, gas gangrene and an extremely high death rate in humans.1–3 5 Classic signs and symptoms of C septicum sepsis include fever, tachycardia, hypotension and generalised pain.2 6 Severe localised pain, overlying skin changes (erythema, oedema, purple-red pigmentation) and gangrene (subcutaneous emphysema, necrosis) can occur in organs such as the uterus or skeletal muscle as the infection progresses.1 6 It is therefore critical that C septicum infection and its appropriate management are known by the medical community caring for susceptible individuals, especially pregnant women.
The current case is the only documented report of a pregnant woman surviving C septicum sepsis in the literature, to the best of our knowledge. We acknowledge the study by Lee and Hsieh5 as a possible survival case; however, the patient in their report did not have a confirmed intrauterine pregnancy and therefore should not be included in this specific population.
The gastrointestinal and genital tracts appear to be common sources for C septicum infection.3 Clostridial bacteria can be found in up to 10% of vaginal and cervical cultures in asymptomatic women.6 Attenuated immune function by means of a possible IgA deficiency could have rendered our patient more vulnerable to C septicum migration into the upper genital tract and subsequent sepsis. Further, our patient denied use of instrumentation to attempt termination of her pregnancy and thus an inadvertent bowel injury was an unlikely source of infection.
Prudent identification, immediate treatment and removal of the nidus of infection are considered to be most effective in managing sepsis and preventing death in patients with C septicum infections.1 2 4 6 Fortunately, our patient received appropriate antibiotics and a D&C before irreversible C septicum infection developed, preventing the seemingly inevitable fatal outcome. Thus, the virulent but treatable nature of Clostridial infections justifies our recommendation to medical practitioners, particularly those who care for pregnant women, to adhere to the following:
- Be aware of the early signs of Clostridial infection during pregnancy
- Signs of sepsis (fever, tachycardia, hypotension)
- Generalised abdominal pain
- With or without localised pain and tissue necrosis to targeted organs
Administer immediate intravenous antibiotic therapy
Remove the nidus of infection
Manage patients promptly for septic shock
Learning points.
According to prior literature, sepsis due to C septicum in pregnant women is fatal.
The current report provides evidence to support survival in these patients by immediately identifying the problem and strictly adhering to recommended guidelines.
Despite its rarity, rural and urban practitioners involved in the care of pregnant women should be aware of the management of C septicum sepsis because of its potential for cure and devastating consequences of inadequate treatment.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Haas L, Tjan D, van Zanten A. Fatal Clostridium septicum infection in a pregnant woman. Neth J Med 2006;64:254–5. [PubMed] [Google Scholar]
- 2.Koransky J, Stargel M, Dowell V. Clostridium septicum bacteraemia: its clinical significance. Am J Med 1979;66:63–6. [DOI] [PubMed] [Google Scholar]
- 3.Rechner P, Agger W, Mruz K, et al. Clinical features of clostridial bacteraemia: a review from a rural area. Clin Infect Dis 2001;33:349–53. [DOI] [PubMed] [Google Scholar]
- 4.Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296–327. [DOI] [PubMed] [Google Scholar]
- 5.Lee C, Hsieh S. Case report: Clostridium septicum infection presenting as liver abscess in a case of choriocarcinoma with liver metastasis. J Gastroenterol Hepatol 1999;14:227–9. [DOI] [PubMed] [Google Scholar]
- 6.Lichtenberg E, Henning C. Conservative management of clostridial endometritis. Am J Obstet Gynecol 2004;191:266–70. [DOI] [PubMed] [Google Scholar]


