Although vancomycin may commonly be used to treat methicillin-sensitive Staphylococcus aureus bacteremia in patients with reported penicillin (PCN) allergies, clinical outcomes are improved if the PCN allergy is addressed, either by taking an allergy history or performing skin testing.
Keywords: decision analysis, vancomycin, allergy, penicillin, Staphylococcus aureus
Abstract
Background. Methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia is a morbid infection. First-line MSSA therapies (nafcillin, oxacillin, cefazolin) are generally avoided in the 10% of patients reporting penicillin (PCN) allergy, but most of these patients are not truly allergic. We used a decision tree with sensitivity analyses to determine the optimal evaluation and treatment for patients with MSSA bacteremia and reported PCN allergy.
Methods. Our model simulates 3 strategies: (1) no allergy evaluation, give vancomycin (Vanc); (2) allergy history–guided treatment: if history excludes anaphylactic features, give cefazolin (Hx-Cefaz); and (3) complete allergy evaluation with history-appropriate PCN skin testing: if skin test negative, give cefazolin (ST-Cefaz). Model outcomes included 12-week MSSA cure, recurrence, and death; allergic reactions including major, minor, and potentially iatrogenic; and adverse drug reactions.
Results. Vanc results in the fewest patients achieving MSSA cure and the highest rate of recurrence (67.3%/14.8% vs 83.4%/9.3% for Hx-Cefaz and 84.5%/8.9% for ST-Cefaz) as well as the greatest frequency of allergic reactions (3.0% vs 2.4% for Hx-Cefaz and 1.7% for ST-Cefaz) and highest rates of adverse drug reactions (5.2% vs 4.6% for Hx-Cefaz and 4.7% for ST-Cefaz). Even in a “best case for Vanc” scenario, Vanc yields the poorest outcomes. ST-Cefaz is preferred to Hx-Cefaz although sensitive to input variations.
Conclusions. Patients with MSSA bacteremia and a reported PCN allergy should have the allergy addressed for optimal treatment. Full allergy evaluation with skin testing seems to be preferred, although more data are needed.
Staphylococcus aureus is a leading cause of bacteremia, with two-thirds being methicillin-sensitive (MSSA) [1–4]. Patients with MSSA bacteremia can develop complications, such as endocarditis or osteomyelitis [5, 6]. Mortality rates in MSSA bacteremia range from 9% to 50% [1, 2, 5–10].
Prolonged courses of the β-lactam antibiotics—nafcillin, oxacillin, and cefazolin—provide the greatest chance of MSSA bacteremia cure [7–11]. Vancomycin is a second-line agent because of its slower microbicidal activity, higher failure rates, and higher associated morbidity and mortality [9, 12, 13]. Guidelines indicate that vancomycin is inferior to β-lactams for MSSA bacteremia [14–16].
The reported prevalence of penicillin (PCN) allergy is 10%–15% among inpatients [17–22]. Once reported, nafcillin, oxacillin, and cefazolin are generally avoided, even in infections such as MSSA where they are clearly superior [11, 17–19, 23]. However, 90%–99% of patients with a reported PCN allergy are not allergic [21, 24–27]. This large discrepancy between reported allergy and true allergy is attributable both to the waning natural history of PCN allergy and misclassification of the original reaction [17, 28].
Infectious disease experts recommend cefazolin for MSSA treatment in patients with PCN allergy unless the reaction to PCN is anaphylactic [5, 14]. However, patients without an anaphylactic allergy history can have future anaphylactic reactions to PCN [29–31]. Because there is 2%–4% cross-reactivity between PCN and first-generation cephalosporins [32–35], allergy practice advises PCN skin testing prior to cefazolin administration, or if skin testing is not available, administration of cefazolin only in patients without symptoms of an immunoglobulin E–mediated reaction by an observed graded challenge [17, 29, 30, 36, 37]. To determine the optimal treatment for patients with MSSA bacteremia and reported PCN allergy, we synthesized the most relevant data from the primary literature, using a decision analysis model.
METHODS
Analytic Overview
The decision analysis model compares 3 treatment strategies for patients with MSSA bacteremia and reported PCN allergy: (1) no allergy evaluation, give vancomycin (Vanc); (2) allergy history-guided treatment: if detailed history excludes anaphylactic features, give cefazolin (Hx-Cefaz); and (3) complete allergy evaluation with history-appropriate PCN skin testing: if skin test (ST) negative, give cefazolin (ST-Cefaz).
Model outcomes at 12 weeks include (1) MSSA cure, recurrence, and death; (2) allergic reactions classified as major or minor and, separately, as potentially iatrogenic; and (3) adverse drug reactions (ADRs; drug toxicity or intolerance). We defined “potentially iatrogenic” as all allergic reactions from cefazolin in patients with PCN allergy history [38].
We assessed which strategy is optimal for each individual outcome. We then created a composite outcome where we summed outcomes using the following weights: cure, +50; recurrence of infection, −20; death, −50; major allergic reactions, −10; minor allergic reactions, −2; and ADRs, −6. A composite score of 50 would indicate a strategy where patients are cured without allergic reactions or ADRs. We examined key input parameters in a series of 1-way, multiway, and probabilistic sensitivity analyses (PSA); we also conducted sensitivity analyses on weights for the composite outcome.
Model Description and Strategies
The decision tree (TreeAge Pro 2014, TreeAge Software, Inc, Williamstown, Massachusetts) includes 3 competing strategies for the patient with MSSA bacteremia and reported PCN allergy (Figure 1). Within each strategy, an alternative strategy may be considered, depending on allergic and adverse outcomes. We limited the model so that no patient receives >3 sequential antibiotics. At the end of a patient's course through the decision tree, he or she is treated with vancomycin, cefazolin, nafcillin, or an alternative non–β-lactam drug (eg, daptomycin). Model outcomes are defined after 12 weeks, at the rightmost end of the tree. If a tree course does not have the outcome of interest, the probabilities are multiplied by a payoff value of 0. If the tree course has the outcome of interest, the probabilities are multiplied by a payoff value of 1. This structure allows us to obtain the percentages of patients in each tree strategy who had each outcome.
Figure 1.
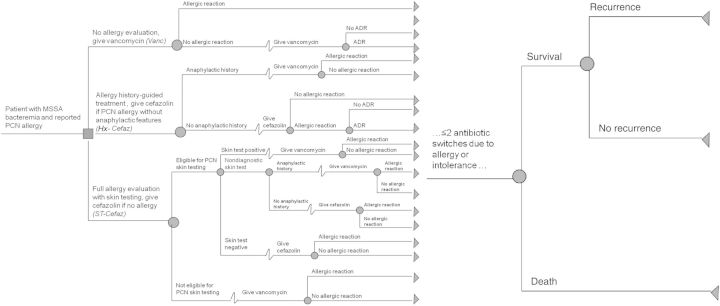
Simplified decision tree for patients with methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia and reported penicillin (PCN) allergy. The decision tree, read from left to right, displays the 12-week course of a patient with MSSA bacteremia and reported PCN allergy. Squares represent decision nodes; circles represent the chance nodes where the probabilities are defined by the input parameters. The tree's 3 prominent branches are the strategies evaluated by the model: (1) no allergy evaluation, give vancomycin (Vanc); (2) allergy history–guided treatment: if history excludes anaphylactic features, give cefazolin (Hx-Cefaz); and (3) complete allergy evaluation with history-appropriate PCN skin testing; if skin test negative, give cefazolin (ST-Cefaz). In each branch, therapy can be altered based on allergic or adverse drug reactions (ADRs); no patient in the tree is treated with >3 drugs in his/her 12-week course. Once a definitive antibiotic course is identified, the patient experiences cure, recurrence, or death, represented by the rightmost part of the figure.
In the Vanc strategy, all patients with MSSA bacteremia and reported PCN allergy receive vancomycin treatment without allergy evaluation. Vancomycin-treated patients may develop an allergic reaction (major or minor) or an ADR. Upon an allergic reaction or ADR to vancomycin, clinicians reconsider therapy options, and the patients have an equal chance of getting (1) an alternative non–β-lactam drug; (2) a history-driven allergy evaluation where cefazolin is given if the PCN allergy history is not anaphylactic; or (3) a full PCN allergy evaluation with history-appropriate skin testing, with cefazolin given if there is no allergy. The latter strategies are similar to the Hx-Cefaz and ST-Cefaz branches of the tree, although, because these patients suffered an ADR or allergic reaction to vancomycin, they do not receive vancomycin again.
In the Hx-Cefaz strategy, patients with a history of PCN allergy with anaphylactic features receive vancomycin; patients with milder allergy histories receive cefazolin. Patients may have an allergic reaction to cefazolin necessitating a drug change to vancomycin. Patients who do not tolerate cefazolin but did not have an allergic reaction have an equal chance of receiving vancomycin therapy or a full allergy evaluation with PCN skin testing. The latter strategy is similar to the ST-Cefaz branch, although if these patients are ST negative, they receive another first-line MSSA antimicrobial (nafcillin). If they are ST positive, they receive vancomycin. Patients with an anaphylactic history receive vancomycin, and may have an allergic reaction or an ADR to vancomycin necessitating a drug change to an alternative non–β-lactam drug.
In the ST-Cefaz arm, patients eligible for skin testing receive PCN skin testing. Patients ineligible for skin testing are given vancomycin. Allergy specialists generally define patients ineligible for skin testing as those with anaphylaxis to PCN in the last 10 years, with a history of a Gell and Coombs type II–IV hypersensitivity reaction to PCN, or currently taking medications that interfere with ST results (eg, antihistamines) [17]. For patients skin tested to PCN, those who are ST negative receive cefazolin, those who are ST positive receive vancomycin, and those with a nondiagnostic ST receive history-guided therapy (as in Hx-Cefaz). In this strategy, patients ineligible for ST who develop an allergic reaction to vancomycin have an equal chance of being given cefazolin guided by allergy history alone or given an alternative non–β-lactam drug.
Input Parameters
The model uses data from literature sources as input parameters (Table 1). These data, reported as fractions and frequencies in the primary literature, are converted into probabilities for inclusion into the decision tree model at the chance nodes (Figure 1). We weighted the outcomes from sources based on cohort numbers when >1 source was available for our base case values (Table 1). Reported probabilities are conditional upon prior outcomes, as indicated by tree structure.
Table 1.
Input Parameters for Decision Analysis Model of Methicillin-Sensitive Staphylococcus aureus and Reported Penicillin Allergy
| Description | Baseline Value, % | Range for Sensitivity Analyses, % | Source |
|---|---|---|---|
| Treatment efficacya | |||
| Vancomycin | |||
| MSSA cure | 62.0 | 36.0–90.0 | [7, 8, 16] |
| MSSA recurrence | 18.8 | 0.0–23.2 | [7, 8] |
| MSSA mortality | 19.2 | 10.0–41.0 | [7, 8, 16] |
| Cefazolin | |||
| MSSA cure | 85.0 | 80.0–88.3 | [7, 8, 16] |
| MSSA recurrence | 9.1 | 0.0–10.0 | [7] |
| MSSA mortality | 5.9 | 2.0–6.0 | [7, 16] |
| Alternativeb | |||
| MSSA cure | 86.4 | 36.0–90.0 | [7, 8, 16, 23] |
| MSSA recurrence | 13.2 | 0.0–23.2 | [7, 8, 23] |
| MSSA mortality | 0.4 | 0.0–41.0 | [7, 8, 16, 23] |
| Allergic reactions | |||
| Vanc | |||
| Allergic reaction to vancomycinc | 3.0 | 2.0–6.4 | [39, 40] |
| Allergic reaction to vancomycin considered major | 8.3 | 0.0–10.0 | [40] |
| Hx-Cefaz | |||
| Patients with PCN allergy whose reaction has anaphylactic features | 5.6 | 0.0–11.2 | PEARd |
| Patients without anaphylactic PCN allergy history who react to cefazoline | 2.2f | 0.2–5.6 | [17, 30, 32, 41–44] |
| ST-Cefaz | |||
| Patients not eligible for PCN skin testing | 9.1 | 0.0–11.0 | [20, 21] |
| Patients with a positive PCN skin test | 1.2 | 0.0–10.0 | [20, 21, 24, 25, 45] |
| Patients with a nondiagnostic PCN skin test | 3.2 | 0.0–10.4 | [20, 21, 24, 25, 45] |
| Allergic reaction to cefazolin or nafcillin given a negative skin test to penicilline | 1.6 | 0.1–1.8 | [20, 21, 24, 25, 45] |
| General | |||
| Allergic reaction to cefazolin considered major | 4.7 | 0.0–5.6 | [26, 36] |
| Death from allergic reaction given a major allergic reaction occurs | 0.2 | 0.0–3.8 | [46–49] |
| Adverse drug reactions | |||
| Vancomycin | 5.3 | 0.0–43.0 | [40, 50, 51] |
| Cefazolin | 4.4 | 0.0–7.0 | [40,51,52] |
Abbreviations: Hx-Cefaz, allergy history-guided treatment: if history excludes anaphylactic features, give cefazolin; MSSA, methicillin-sensitive Staphylococcus aureus; PCN, penicillin; PEAR, Partners Enterprise Allergy Repository; ST-Cefaz, complete allergy evaluation with penicillin skin testing, give cefazolin if negative; Vanc, no allergy evaluation, give vancomycin.
a Outcomes defined 12 weeks after initial blood culture.
b Base case outcomes based on 1 study [23]; examined range for outcomes from vancomycin therapy in sensitivity analyses.
c Excludes infusion reactions (eg, “red man syndrome”).
d Partners Enterprise Allergy Repository, accessed November 2013.
e The sum of these reactions were considered potentially iatrogenic allergic reactions.
f Mathematical computation = ∑ (patients who react to cefazolin who are skin test positive + patients who react to cefazolin who are skin test negative) = ∑ [{ proportion of patients skin test positive (0.49)} × {positive predictive value of PCN skin testing (0.4)} × {the cross-reactivity of PCN and cefazolin (0.029)} + {patients who react to cefazolin who are skin test negative (0.016)}] = (0.49 × 0.4 × 0.029) + 0.016 = 0.022 = 2.2%.
Within treatment efficacy, parameters include the 12-week MSSA cure with vancomycin (62.0%) and cefazolin (85.0%), and the 12-week probability of MSSA recurrence and mortality associated with vancomycin (18.8% and 19.2%, respectively) and cefazolin (9.1% and 5.9%, respectively) [7, 8, 16]. Because only 1 study reports MSSA recurrence (13.2%) and death (0.4%) with an alternative drug, we used vancomycin literature ranges to define cure, recurrence, and death with an alternative, non–β-lactam drug [23].
The chance of allergic reaction to vancomycin was 3.0%, of which 8.3% of reactions were considered major and 91.7% considered minor [39, 40]. In the Hx-Cefaz strategy, data from an internal database informed the proportion of patients whose reported reaction to PCN had anaphylactic features (5.6%), defined by reported reactions of bronchospasm, wheezing, anaphylaxis, hypotension, and angioedema [53]. The proportion of patients without an anaphylactic history who react to cefazolin was 2.2%, derived from cohort data and mathematical computation [17, 30, 32, 41–44]. In the ST-Cefaz strategy, we defined 9.1% of patients as ST ineligible [20, 21]; among those eligible, 95.6% were ST negative, 1.2% were ST positive, and 3.2% had a nondiagnostic ST [20, 21, 24, 25, 45]. After a negative ST, 1.6% of patients react to cefazolin [20–22, 45]. In both the Hx-Cefaz and ST-Cefaz strategies, once an allergic reaction occurs, 4.7% can be considered major (95.3% are minor); 0.2% of major reactions result in death [26, 36, 46–49, 54]. ADR rate was 5.3% with vancomycin and 4.4% with cefazolin [40, 50–52].
Sensitivity Analysis
We conducted sensitivity analyses using probability ranges from the primary literature (Table 1). We varied parameters individually (1-way sensitivity analysis) for each outcome and identified influential parameters. We then varied these key inputs simultaneously in a series of multiway sensitivity analyses. Finally, we used literature estimates to create distributions for the key input parameters to conduct PSA, whereby 100 000 patients travel through the decision tree sampling different probabilities from the defined distributions (Supplementary Table 1). We conducted a PSA for all 3 strategies on all outcomes. Because results for the Hx-Cefaz and ST-Cefaz groups were similar, we subsequently ran the PSA for Vanc compared with a sample allergy evaluation strategy (Hx-Cefaz).
RESULTS
Base Case
Individual Outcomes
The Vanc strategy results in 67.3% chance of cure, 14.8% chance of recurrence, and 17.9% chance of death (Table 2). Total allergic reactions are 3.0%, with 0.3% of patients experiencing a major reaction and 0.8% experiencing a potentially iatrogenic reaction. ADRs are present in 5.2% of vancomycin-treated patients. Hx-Cefaz results in better clinical outcomes than Vanc, including a much higher chance of cure (83.4%), as well as a substantially lower chance of recurrence (9.3%), and less than half the 12-week mortality (7.3%). Fewer patients in Hx-Cefaz have allergic reactions (2.4%) and ADRs (4.6%) than in Vanc (3.0% and 5.2%, respectively). While major allergic reactions (0.1%) are less frequent in Hx-Cefaz, more patients experience a reaction that could be considered iatrogenic (2.1%) than in the Vanc strategy.
Table 2.
Clinical Outcomes of 3 Strategies for Management of Methicillin-Sensitive Staphylococcus aureus Bacteremia and Reported Penicillin Allergy
| Outcome | Vanc | Hx-Cefaz | ST-Cefaz |
|---|---|---|---|
| Cure, % | 67.3 | 83.4 | 84.5 |
| Recurrence, % | 14.8 | 9.3 | 8.9 |
| Death, % | 17.9 | 7.3 | 6.6 |
| Allergic reactionsa, total, % | 3.0 | 2.4 | 1.7 |
| Major, % | 0.3 | 0.1 | 0.1 |
| Minor, % | 2.8 | 2.2 | 1.6 |
| Iatrogenic allergic reactionsb, % | 0.8 | 2.1 | 1.6 |
| Adverse drug reactions, % | 5.2 | 4.6 | 4.7 |
| Composite outcome valuec (strategy rank) | 21.3 (3) | 35.9 (2) | 36.8 (1) |
Abbreviations: Hx-Cefaz, allergy history-guided treatment: if history excludes anaphylactic features, give cefazolin; PCN, penicillin; ST-Cefaz, complete allergy evaluation with PCN skin testing, give cefazolin if negative; Vanc, no allergy evaluation, give vancomycin.
a Major and minor reactions do not sum to total due to rounding.
b Reactions from cefazolin in a patient with reported PCN allergy.
c Composite outcome weights: cure, +50; recurrence of infection, −20; death, −50; major allergic reactions, −10; minor allergic reactions, −2; adverse drug reactions, −6.
Clinical outcomes for ST-Cefaz are marginally better than for Hx-Cefaz and markedly improved over Vanc. The probabilities of MSSA cure, recurrence, and death with ST-Cefaz are 84.5%, 8.9%, and 6.6%, respectively. ST-Cefaz projects the fewest allergic reactions of the strategies, with 1.7% having an allergic reaction, including 0.1% experiencing a major reaction and 1.6% of patients experiencing an allergic reaction that could be considered iatrogenic. ST-Cefaz projects similar ADRs to Hx-Cefaz (4.7% vs 4.6%).
Composite Outcome
Using the composite outcome, ST-Cefaz is the optimal strategy, with a value of 36.8, over Hx-Cefaz (35.9) and Vanc (21.3). Overall, the optimal strategy was insensitive to clinically reasonable alternative weighting of individual outcomes chosen for the composite score. Even when iatrogenicity was included in the composite with weight on par with death (−50), ST-Cefaz remains the optimal strategy (36.0) compared with Hx-Cefaz (34.9) and Vanc (20.9).
Sensitivity Analyses
Vanc Versus Allergy Evaluation
Because the allergy evaluation strategies offer similar outcomes, for simplicity, we focused sensitivity analyses on Vanc compared to a sample allergy strategy, Hx-Cefaz.
One-Way Sensitivity Analyses
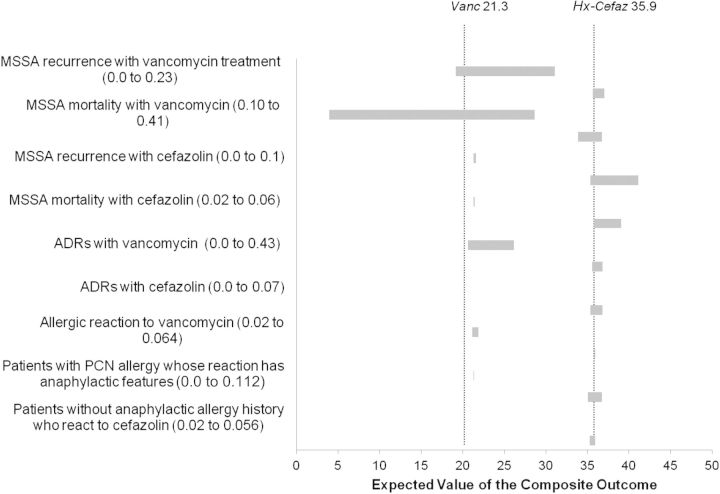
With variation of input parameters within all reasonable ranges from reported literature, Vanc consistently has inferior clinical outcomes of MSSA cure, recurrence, death, and the composite outcome. The input parameters with the greatest effect on the value of the composite outcome are the probability of death and recurrence with vancomycin (Figure 2). However, varying these inputs within reported literature ranges still leads to Vanc giving the least desired outcomes.
Figure 2.
One-way sensitivity analyses for the composite outcome for patients with methicillin-sensitive Staphylococcus aureus (MSSA) bacteremia and reported penicillin (PCN) allergy, comparing Vanc to Hx-Cefaz (see Figure 1 for decision tree). This tornado diagram summarizes the results of all influential 1-way sensitivity analyses on the composite outcome (cure, +50; recurrence of infection, −20; death, −50; major allergic reactions, −10; minor allergic reactions, −2; adverse drug reactions [ADRs], −6) with the variables examined within the probabilities described on the vertical axis. Each horizontal bar represents the range of expected values generated by varying the related variable across its plausible range, as indicated at opposite ends of each bar. A wide bar indicates that the associated variable has a large potential effect on the composite outcome. The vertical dotted lines represent the expected value of the composite outcome for Vanc (21.3) and Hx-Cefaz (35.9). Because there is no overlap between bars in Vanc and Hx-Cefaz, there is no plausible input parameter change that could result in the Vanc strategy having a higher composite outcome than the Hx-Cefaz strategy. Abbreviations: Hx-Cefaz, allergy history–guided treatment: if history excludes anaphylactic features, give cefazolin; Vanc, no allergy evaluation, give vancomycin.
When examining individual outcomes, iatrogenic allergic reactions, although generally infrequent in all strategies (<2.1%), are always minimized with Vanc. If <1.7% of patients (base case 3.0%) have an allergic reaction to vancomycin, then Vanc results in the fewest total allergic reactions. If >5% of patients experience an ADR from cefazolin (base case 4.4%), then Vanc becomes optimal over allergy evaluation in terms of minimizing ADRs.
Multiway Sensitivity Analyses
We varied the most influential parameters determining the composite outcome (Figure 2); we also set all inputs to be the most attractive with regard to the Vanc strategy. In all situations, Vanc projects the least attractive infectious outcomes and composite score. As in the 1-way sensitivity analyses, within reasonable parameter variations from the literature-reported values, specific parameter variations lead to Vanc being optimal in terms of minimizing allergic reactions and ADRs (Supplementary Figures 1 and 2).
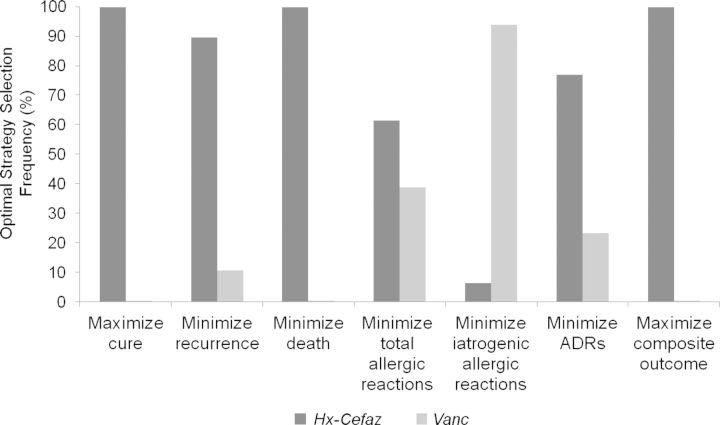
Probabilistic Sensitivity Analysis
Using distributions for influential input parameters (Supplementary Table 1), average results are very close to the base case values, and Vanc consistently provides the lowest composite score (Supplementary Table 2). In PSA, Hx-Cefaz is preferred over Vanc to maximize cure (99.8%), minimize recurrence (89.5%), minimize death (99.9%), minimize total allergic reaction (61.3%), minimize ADRs (76.8%), and maximize the composite outcome 99.9% of the time (Figure 3). Only if the most important goal is to minimize total potentially iatrogenic allergic reactions would Vanc be favored (93.8%).
Figure 3.
Optimal strategy selection in Monte Carlo simulation of 100 000 patients with methicillin-sensitive Staphylococcus aureus bacteremia and reported penicillin allergy using probabilistic sensitivity analysis, comparing Vanc to Hx-Cefaz (see Figure 1 for decision tree). The bars (horizontal axis) display the frequency (vertical axis) with which a strategy is optimal for each clinical outcome defined, allowing variability in all input parameters simultaneously in probabilistic sensitivity analyses. Hx-Cefaz is the optimal choice for all outcomes, except minimizing iatrogenic allergic reactions where the Vanc strategy is preferred. Abbreviations: ADR, adverse drug reaction; Hx-Cefaz, allergy history–guided treatment: if history excludes anaphylactic features, give cefazolin; Vanc, no allergy evaluation, give vancomycin.
Optimal Allergy Evaluation Strategy
One-Way Sensitivity Analyses
Although outcomes between Hx-Cefaz and ST-Cefaz were quite close, variations of most parameters within literature-reported ranges continued to modestly favor ST-Cefaz. MSSA cure, recurrence, and death were sensitive to the proportion of patients with a positive ST, with Hx-Cefaz becoming optimal within the range examined. Considering total allergic reactions, the optimal strategy is most sensitive to the proportion of patients with a nonanaphylactic PCN allergy history who react to cefazolin. Specifically, Hx-Cefaz becomes optimal if <1.4% (base case, 2.2% [range, 0.02%–5.6%]) of patients with a nonanaphylactic PCN allergy history react to cefazolin. Considering ADRs, ST-Cefaz becomes optimal if the probability of an ADR from cefazolin is <2.9% (base case, 4.4% [range, 0%–7.0%]). The composite outcome favored ST-Cefaz, but was also sensitive to the probability of a positive ST; Hx-Cefaz becomes optimal when >8.5% (base case, 1.2% [range, 0%–10.0%]) of patients are ST positive.
Multiway Sensitivity Analyses
Variation of 2–3 input parameters at the same time favored ST-Cefaz. Parameters identified in 1-way sensitivity analyses lead to different conclusions about the optimal allergy strategy.
Probabilistic Sensitivity Analysis
Using distributions for influential input parameters (Supplementary Table 1), ST-Cefaz was preferred to Hx-Cefaz to maximize cure 99.5% of the time, minimize recurrence 90.4% of the time, minimize death 99.7% of the time, minimize total allergic reactions 83.8% of the time, and maximize the composite outcome 99.8% of the time. Hx-Cefaz was preferred to ST-Cefaz to minimize ADRs 96.1% of the time.
DISCUSSION
Using a decision analysis model, we project that patients with MSSA bacteremia and reported PCN allergy will have inferior outcomes if treated with vancomycin rather than having their PCN allergy addressed. Both the base case analysis and sensitivity analyses favored a full evaluation with PCN skin testing to optimize outcomes compared with basing therapy on PCN allergy history alone; however, differences were small and sensitive to uncertain input parameters.
Despite our finding that no allergy evaluation and treatment with vancomycin is inferior, patients with MSSA bacteremia and reported PCN allergy commonly receive vancomycin [11, 23]. This could reflect providers' concerns about iatrogenic allergic reactions and limited PCN allergy knowledge [18, 55]. Indeed, the only model outcome that suggested benefit to vancomycin was minimizing potential iatrogenic allergic reactions. Given our findings, the practice of giving vancomycin to patients with MSSA bacteremia and a reported PCN allergy without investigating the allergy should not be standard, regardless of the availability of allergy specialists or PCN skin testing. A brief bedside allergy history that excludes anaphylactic features can guide cefazolin use and result in better outcomes than choosing vancomycin.
Perhaps counterintuitively, our model projects that the use of vancomycin would result in more allergic reactions than the use of cefazolin through allergy history–guided therapy or skin testing–guided therapy. Allergy to vancomycin includes immediate reactions as well as delayed reactions (eg, morbilliform eruptions, drug rash with eosinophilia, and systemic symptoms syndrome) [17, 56–58]. Notably, our projection of increased allergic reactions with vancomycin excluded the common infusion reaction “red man syndrome” [17, 39, 59].
Our model projects that ST-Cefaz results in the most favorable outcomes. However, the differences were small, and literature-reported variations suggest that data may be inadequate to definitively determine which allergy evaluation strategy is optimal. Whereas much of the allergy skin testing and challenge literature is derived from outpatients, those with MSSA bacteremia are usually inpatients [24, 26, 36]. Because we may see different skin testing eligibility and results among inpatients, more robust inpatient data would be of value. A key parameter in determining the optimal allergy strategy is the proportion of patients without an anaphylactic PCN allergy history who react to cefazolin; this parameter was based on sparse literature and mathematical calculation. Last, because of the declining rate of reported ST positivity in the literature, we deliberately used recent allergy data to inform skin testing inputs [20, 21, 24, 26, 45, 51]. The optimal allergy strategy was sensitive to this parameter within reported ranges, and older data that used more skin-testing reagents reported higher rates of ST positivity [31].
While the model suggests that Hx-Cefaz may be as good as ST-Cefaz, ST-Cefaz is likely preferable for avoiding iatrogenic allergic reactions that can result in patient dissatisfaction. PCN skin testing is currently performed using Pre-Pen (penicilloyl-poly-lysine) and dilutions of PCN. The negative predictive value with these reagents is at least 95%; the procedure can safely be performed on general medical floors, and results are available within 1 hour [17, 21, 26, 45]. With proper training, PCN skin testing can be performed by registered nurses, which allows for reduced costs of providing the service [22].
Although data limitations and variability of input parameters in this analysis made it challenging to project which allergy strategy was optimal, either strategy is substantially better than Vanc. This conclusion is insensitive to parameters and despite evaluations of Vanc in a “best case for Vanc” scenario. We did not consider that patients with PCN allergy may have other drug allergies that could impact treatment. We justify exclusion of nafcillin because cefazolin is considered to be equally effective, better tolerated, and less expensive than nafcillin for MSSA bacteremia [16, 52, 60–62]. We additionally justify exclusion of other alternative agents (eg, daptomycin) as initial therapy because of limited comparative infectious outcome data in MSSA bacteremia [63–66]. However, given vancomycin's poor efficacy and tolerability in MSSA bacteremia, future comparisons of β-lactams to alternative agents will be important to consider. Finally, although we limited our outcome assessment to 12 weeks, we believe this strengthens our conclusion that the allergy must be addressed, as recurrences are more likely with vancomycin than cefazolin [7–11, 15, 16, 23].
Compared to treatment with vancomycin, we find that patients with MSSA bacteremia and reported PCN allergy have improved outcomes when treated with cefazolin, either by an allergy history–guided treatment or full allergy evaluation with skin testing. Although full allergy evaluation is likely preferred over history alone, more data from inpatients are needed.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online (http://cid.oxfordjournals.org). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Financial support. This work was supported by the NIH (grant number T32 HL116275 to K. G. B.).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Reed SD, Friedman JY, Engemann JJ, et al. Costs and outcomes among hemodialysis-dependent patients with methicillin-resistant or methicillin-susceptible Staphylococcus aureus bacteremia. Infec Control Hosp Epidemiol 2005; 26:175–83. [DOI] [PubMed] [Google Scholar]
- 2.Naidoo R, Nuttall J, Whitelaw A, Eley B. Epidemiology of Staphylococcus aureus bacteraemia at a tertiary children's hospital in Cape Town, South Africa. PLoS One 2013; 8:e78396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Hal SJ, Jenson SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev 2012; 25:362–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003; 39:53–9. [DOI] [PubMed] [Google Scholar]
- 5.Fowler VG, Sexton DJ. Clinical approach to Staphylococcus aureus bacteremia in adults. In: UpToDate, Baron EL, ed. Waltham, MA: UpToDate, 2013. Accessed 27 May 2015. [Google Scholar]
- 6.Bai AD, Showler A, Burry L, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis 2015; 60:1451–61. [DOI] [PubMed] [Google Scholar]
- 7.Stryjewski ME, Szcech LA, Benjamin DK, et al. Use of vancomycin or first generation cephalosporins for the treatment of hemodialysis dependent patients with methicillin-susceptibile Staphylococcus aureus bacteremia. Clin Infect Dis 2006; 44:190–6. [DOI] [PubMed] [Google Scholar]
- 8.Kim EK, Oh M, Choe K, Kim S, Kim K, Kim H. Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 2008; 52:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.González C, Rubio M, Romero-Vivas J, González M, Picazo JJ. Bacteremic pneumonia due to Staphylococcus aureus: a comparison of disease caused by methicillin-resistant and methicillin-susceptible organisms. Clin Infect Dis 1999; 29:1171–7. [DOI] [PubMed] [Google Scholar]
- 10.Mylotte JM, McDermott C, Spooner JA. Prospective study of 114 consecutive episodes of Staphylococcus aureus bacteremia. Rev Infect Dis 1987; 9:891–907. [DOI] [PubMed] [Google Scholar]
- 11.McDanel JS, Perencevich EN, Diekema DJ, et al. Comparative effectiveness of beta-lactams versus vancomycin for treatment of methicillin-susceptible Staphylococcus aureus bloodstream infections among 122 hospitals. Clin Infect Dis 2015; 61:361–7. [DOI] [PubMed] [Google Scholar]
- 12.Fowler VG, Kong LK, Corey GR, et al. Recurrent Staphylococcus aureus bacteremia: pulsed-field gel electrophoresis findings in 29 patients. J Infect Dis 1999; 179:1157. [DOI] [PubMed] [Google Scholar]
- 13.LaPlante KL, Rybak MJ. Impact of high-inoculum Staphylococcus aureus on the activities of nafcillin, vancomycin, linezolid, and daptomycin, alone and in combination with gentamicin, in an in vitro pharmacodynamic model. Antimicrob Agents Chemother 2004; 48:4665–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011; 52:1–38. [DOI] [PubMed] [Google Scholar]
- 15.Chang FY, Peacock JE, Jr, Musher DM, et al. Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study. Medicine 2003; 82:333–9. [DOI] [PubMed] [Google Scholar]
- 16.Schweizer ML, Furuno J, Harris AD, et al. Comparative effectiveness of nafcillin or cefazolin versus vancomycin in methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis 2011; 11:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Solensky R, Khan D. Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010; 105:259–73. [DOI] [PubMed] [Google Scholar]
- 18.Picard M, Begin P, Bouchard H, et al. Treatment of patients with a history of penicillin allergy in a large tertiary care academic hospital. J Allergy Clin Immunol Pract 2013; 1:252–7. [DOI] [PubMed] [Google Scholar]
- 19.Lee CE, Zembower TR, Fotis MA, et al. The incidence of antimicrobial allergies in hospitalized patients: implication regarding prescribing patters and emerging bacterial resistance. Arch Inter Med 2000; 160:2819–22. [DOI] [PubMed] [Google Scholar]
- 20.Arroliga ME, Wagner W, Bobek MB, Hoffman-Hogg L, Gordon SM, Arroliga AC. A pilot study of penicillin skin testing in patients with a history of penicillin allergy admitted to the medical ICU. Chest 2000; 118:1106–8. [DOI] [PubMed] [Google Scholar]
- 21.Rimawi RH, Cook PP, Gooch M, et al. The impact of penicillin skin testing on clinical practice and antimicrobial stewardship. J Hosp Med 2013; 8:341–5. [DOI] [PubMed] [Google Scholar]
- 22.Macy E, Contreras R. Health care use and serious infection prevalence associated with penicillin “allergy” in hospitalized patients: a cohort study. J Allergy Clin Immunol 2014; 133:790–6. [DOI] [PubMed] [Google Scholar]
- 23.Chan KE, Warren HS, Thadhani RI, et al. Prevalence and outcomes of antimicrobial treatment for Staphylococcus aureus bacteremia in outpatients with ESRD. J Am Soc Nephrol 2012; 23:1551–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.del Real GA, Rose ME, Ramirez-Atamoros MT, et al. Penicillin skin testing in patients with a history of beta-lactam allergy. Ann Allergy Asthma Immunol 2007; 98:355–9. [DOI] [PubMed] [Google Scholar]
- 25.Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomyin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol 2006; 97:681–7. [DOI] [PubMed] [Google Scholar]
- 26.Macy E, Ngor E. Safely diagnosing clinically significant penicillin allergy using only penicilloyl-poly-lysine. J Allergy Clin Immunol Pract 2013; 1:258–63. [DOI] [PubMed] [Google Scholar]
- 27.Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD, Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med 2009; 54:72–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blanca M, Torres MJ, Garcia JJ, et al. Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol 1999; 103(5 pt 1):918–24. [DOI] [PubMed] [Google Scholar]
- 29.Stember RH. Prevalence of skin test reactivity in patients with convincing, vague, and unacceptable histories of penicillin allergy. Allergy Asthma Proc 2005; 26:59–64. [PubMed] [Google Scholar]
- 30.Solensky R, Earl HS, Gruchalla RS. Penicillin allergy: prevalence of vague history in skin test-positive patients. Ann Allergy Asthma Immunol 2000; 85:195–9. [DOI] [PubMed] [Google Scholar]
- 31.Sogn DD, Evans RR, Shepherd GM, et al. Results of the National Institute of Allergy and Infectious Diseases Collaborative Clinical Trial to test the predictive value of skin testing with major and minor penicillin derivatives in hospitalized adults. Arch Int Med 1992; 152:1025–32. [PubMed] [Google Scholar]
- 32.Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. Pediatrics 2005; 115:1048–57. [DOI] [PubMed] [Google Scholar]
- 33.Pichichero ME. Cephalosporins can be prescribed safely for penicillin-allergic patients. J Fam Pract 2006; 55:106–12. [PubMed] [Google Scholar]
- 34.Pichichero ME. Use of selected cephalosporins in penicillin-allergic patients: a paradigm shift. Diagn Microbiol Infect Dis 2007; 57(3 suppl):13S–8. [DOI] [PubMed] [Google Scholar]
- 35.Pichichero ME, Casey JR. Safe use of selected cephalosporins in penicillin-allergic patients: a meta-analysis. Otolaryngol Head Neck Surg 2007; 36:340–7. [DOI] [PubMed] [Google Scholar]
- 36.Kao L, Rajan J, Roy L, Kavosh E, Khan DA. Adverse reactions during drug challenges: a single US institution's experience. Ann Allergy Asthma Immunol 2013; 110:86–91. [DOI] [PubMed] [Google Scholar]
- 37.Solensky R, Earl HS, Gruchalla RS. Clinical approach to penicillin-allergy patients: a survey. Ann Allergy Asthma Immunol 2000; 84:329–33. [DOI] [PubMed] [Google Scholar]
- 38.Kohn LT, Corrigan JM, Donaldson MS, eds. To err is human: building a safer health system. Washington, DC: The National Academies Press, 2000. [PubMed] [Google Scholar]
- 39.Cavalcanti AB, Goncalves AR, Almeida CS, Bugano DD, Silva E. Teichoplanin versus vancomycin for proven or suspected infection. Cochrane Database Syst Rev 2010; CD007022. [DOI] [PubMed] [Google Scholar]
- 40.Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. Clin Infect Dis 2004; 38:1651–72. [DOI] [PubMed] [Google Scholar]
- 41.Gadde J, Spence M, Wheeler B, Adkinson FJ. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993; 270:2456–63. [PubMed] [Google Scholar]
- 42.Fox S, Park MA. Penicillin skin testing in the evaluation and management of penicillin allergy. Ann Allergy Asthma Immunol 2011; 106:1–7. [DOI] [PubMed] [Google Scholar]
- 43.Goodman EJ, Morgan MJ, Johnson PA, Nichols BA, Denk N, Gold BB. Cephalosporins can be given to penicillin-allergic patients who do not exhibit an anaphylactic response. J Clin Anesth 2001; 13:561–4. [DOI] [PubMed] [Google Scholar]
- 44.Earl HS, Casey WC, Gruchalla RS. Safety of cephalosporin administration to patients with histories of penicillin allergy. J Allergy Clin Immunol 2004; 113:1220–2. [DOI] [PubMed] [Google Scholar]
- 45.Sagar PS, Katelaris CH. Utility of penicillin skin testing in patients with a history of penicillin allergy. Asia Pac Allergy 2013; 3:115–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma L, Danoff TM, Borish L. Case fatality and population mortality associated with anaphylaxis in the United States. J Allergy Clin Immunol 2014; 133:1075–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Renaudin JM, Beaudouin E, Ponvert C, Demoly P, Moneret-Vautrin DA. Severe drug-induced anaphylaxis: analysis of 333 cases recorded by the Allergy Vigilance Network from 2002 to 2010. Allergy 2013; 68:929–37. [DOI] [PubMed] [Google Scholar]
- 48.Ribiero-Vaz I, Marques J, Demoly P, Polonia J, Gomes ER. Drug-induced anaphylaxis: a decade of reporting to the Portugese Pharmacovigilance Authority. Eur J Clin Pharmacol 2013; 69:673–81. [DOI] [PubMed] [Google Scholar]
- 49.Wang DY, Forslund C, Persson U, Wiholm BE. Drug-attributed anaphylaxis. Pharmacoepidemiol Drug Saf 1998; 7:269–74. [DOI] [PubMed] [Google Scholar]
- 50.Kohno S, Yamaguchi K, Aikawa N, et al. Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J Antimicrob Chemother 2007; 60:1361–9. [DOI] [PubMed] [Google Scholar]
- 51.Park MA, McClimon BJ, Ferguson B, et al. Collaboration between allergists and pharmacists increases beta-lactam antibiotic prescriptions in patients with a history of penicillin allergy. Int Arch Allergy Immunol 2011; 154:57–62. [DOI] [PubMed] [Google Scholar]
- 52.Youngster I, Shenoy ES, Hooper DC, Nelson SB. Comparative evaluation of the tolerability of cefazolin and nafcillin for treatment of methicillin-susceptible Staphylococcus aureus infections in the outpatient setting. Clin Infect Dis 2014; 59:369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuperman GJ, Marston E, Paterno M, et al. Creating an enterprise-wide allergy repository at Partners HealthCare System. AMIA Annu Symp Proc 2003; 2003:376–80. [PMC free article] [PubMed] [Google Scholar]
- 54.Iammatteo M, Blumenthal KG, Saff R, Long AA, Banerji A. Safety and outcomes of test doses for the evaluation of adverse drug reactions: a 5-year retrospective review. J Allergy Clin Immunol Pract 2014; 2:768–74. [DOI] [PubMed] [Google Scholar]
- 55.Blumenthal KG, Shenoy ES, Hurwitz S, Varughese CA, Hooper DC, Banerji A. Effect of a drug allergy educational program and antibiotic prescribing guideline on inpatient clinical providers’ antibiotic prescribing knowledge. J Allergy Clin Immunol Pract 2014; 2:407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Blumenthal KG, Patil SU, Long AA. The importance of vancomycin in drug rash eosinophilia and systemic symptoms (DRESS) syndrome. Allergy Asthma Proc 2012; 33:165–71. [DOI] [PubMed] [Google Scholar]
- 57.Stevens DL, Herr D, Lampiris H, Hunt JL, Batts DH, Hafkin B. Linezolid versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus infections. Clin Infect Dis 2002; 34:1481–90. [DOI] [PubMed] [Google Scholar]
- 58.An SY, Hwang EK, Kim JE, et al. Vancomycin-associated spontaneous cutaneous adverse drug reactions. Allergy Asthma Immunol Res 2011; 3:194–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wallace MR, Mascola JR, Oldfield EC. Red man syndrome: incidence, etiology and prophylaxis. J Infect Dis 1991; 164:1180–5. [DOI] [PubMed] [Google Scholar]
- 60.Faden D, Faden HS. The high rate of adverse drug events in children receiving prolonged outpatient parenteral antibiotic therapy for osteomyelitis. Pediatr Infect Dis 2009; 28:539–41. [DOI] [PubMed] [Google Scholar]
- 61.Lee S, Choe PG, Song KH, et al. Is cefazolin inferior to nafcillin for treatment of methicillin-susceptible Staphylococcus aureus bacteremia? Antimicrob Agents Chemother 2011; 55:5122–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paul M, Zemer-Wassercug N, Talker O, et al. Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia? Clin Microbiol Infect 2011; 17:1581–6. [DOI] [PubMed] [Google Scholar]
- 63.Martone WJ, Lamp KC. Efficacy of daptomycin in complicated skin and skin-structure infections due to methicillin-sensitive and -resistant Staphylococcus aureus: results from the CORE Registry. Curr Med Res Opin 2006; 22:2337–43. [DOI] [PubMed] [Google Scholar]
- 64.Sakoulas G, Brown J, Lamp KC, Friedrich LV, Lindfield KC. Clinical outcomes of patients receiving daptomycin for the treatment of Staphylococcus aureus infections and assessment of clinical factors for daptomycin failure: a retrospective cohort study utilizing the Cubicin Outcomes Registry and Experience. Clin Ther 2009; 31:1936–45. [DOI] [PubMed] [Google Scholar]
- 65.Fowler VG, Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med 2006; 355:653–65. [DOI] [PubMed] [Google Scholar]
- 66.Segreti JA, Crank CW, Finney MS. Daptomycin for the treatment of gram-positive bacteremia and infective endocarditis: a retrospective case series of 31 patients. Pharmacotherapy 2006; 26:347–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.