Abstract
Non-compaction of the ventricular myocardium is a congenital dysfunction of ventricular morphogenesis caused by the arrest of normal embryogenesis of the ventricles. It is considered as a rare disease and can involve both ventricles but commonly the left ventricle. It is classified into isolated non-compaction of the ventricles and non-compaction associated with other congenital heart defects. Its association with Ebstein's anomaly is very rare. We are reporting a rare case of severe heart failure and complex cardiac anomaly including biventricular non-compaction cardiomyopathy, Ebstein's anomalies and large patent ductus arteriosus with severe persistent pulmonary hypertension in a 31-weeks-old preterm infant. The infant recovered smoothly and continued to be asymptomatic and off medications throughout his 2 years follow-up period. Up to our knowledge, this is the youngest and first patient yet reported to have this disease at this age with good recovery.
Background
Ventricular non-compaction associated with Ebstein's anomaly is a rarely reported pathology.1 2 Attenhofer Jost et al3 reported the first three cases of left ventricular non-compacted cardiomyopathy with Ebstein's anomaly, followed by Sinkovec et al4 who reported two cases of biventricular myocardial non-compaction associated with Ebstein's malformation. In Qatar Numan et al5 reported one case of Ebstein's anomaly with non-compacted cardiomyopathy in adult patients. Reviewing all the reported cases worldwide, none was a preterm infant. Hence, it was the first reported case of this rare condition, which presented immediately after birth and responded very well to treatment. The case also showed a very good example of good outcome with early diagnosis and prompt treatments.
Case presentation
A preterm male infant was born at 31 weeks of gestation to a Gravida 2 mother, after an uneventful pregnancy. Parents are first-degree relatives. The mother received no medications during pregnancy apart from folic acid tablets. Antenatal ultrasound showed the possibility of congenital heart disease and ascites. The patient was born in a level II hospital. At birth he was vigorous with Apgar scores of 8 and 9 at 1 and 5 min, respectively. Soon after birth, the patient developed cyanosis in which resuscitation was performed. Oxygen saturation remained 77% on room air with no obvious respiratory distress. He was then intubated and transferred to a level III perinatal centre. Oxygen saturation remained 80% on 100% FIO2 during transportation. Upon arrival, the patient was cyanosed with respiratory distress. Cardiac examination revealed a significant systolic murmur at left lower sternal border with well-felt pulses and the liver was grossly enlarged. On the basis of these findings, the possibility of cyanotic congenital heart disease was raised. Echocardiography showed very thick trabeculated spongy myocardium (non-compacted) hypertrophied right and left ventricles with impaired shortening fraction (FS) of 16% and significant downward displaced tricuspid valve leaflets (Ebstein's anomaly). Large patent ductus arteriosus with severe persistent pulmonary hypertension of the newborn were also picked up by echo (figure 1). Chest radiograph showed enlarged heart, while electrocardiogram showed biventricular hypertrophy.
Figure 1.
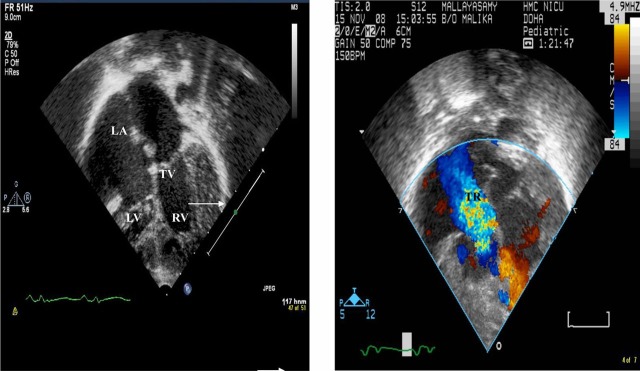
Left. Four chamber views showed downward displacement of tricuspid valve (Ebstein`s anomaly) and the arrow showed non-compacted right and left ventricular wall. Right view with contrast showed tricuspid regurgitation.
Extensive workup was done to elicit the cause of this cardiomyopathy. No abnormalities were found in the chromosomal study, TORCH screening, metabolic screening, abdominal and brain ultrasound.
Hence, we diagnosed biventricular non-compaction cardiomyopathy associated with Ebstein's anomaly; the patient was supported with mechanical ventilation, inhaled nitric oxide, inotropic support and diuretics. No arrhythmias were identified on continuous electrocardiographic monitoring. He needed mechanical ventilation for 17 days; oxygen requirement was reduced gradually and he was extubated with good saturation on room air.
Serial echocardiography follow-up showed that the FS was improving along with better biventricular contractility.
The patient was discharged home on room air, oral digoxin and diuretics were given as long-treatment plan. Growth and development are within the normal range for his age.
Multidisciplinary teams including a neonatologist, cardiologist and geneticist together with the neurodevelopmental clinic planned for a follow-up. His condition remained stable and the patient improved over time. The serial follow-up echoes showed improvement in the contractility and his last echocardiography at the age of 2 years showed good biventricular contractility with mild tricuspid regurgitation and FS of 40% (figure 2). Currently, he is off medications and achieving a normal growth pattern together with adequate milestone for his age.
Figure 1.
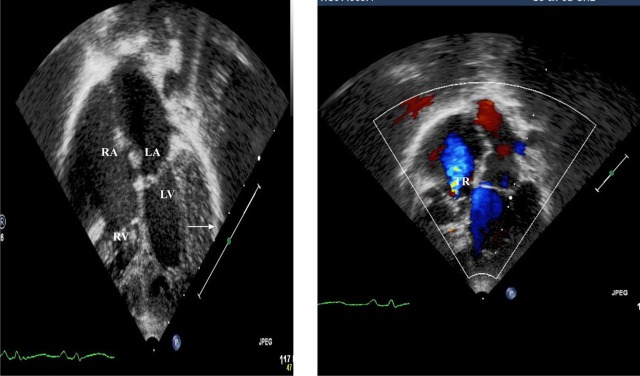
Left. After 2 years. Four-chamber view showed downward displacement of tricuspid valve (Ebstein`s anomaly) and the arrow showed reduction in right ventricular wall non-compaction. Right view with contrast showed improved tricuspid regurgitation.
Investigations
Full blood count was normal
Renal function test were normal throughout
Liver function test was normal
Chest x-ray showed enlarged cardiac shadow
Ultrasound brain and abdomen were normal
Chromosomes study: XY 46
TORCH screening negative
DNA banking for parent's blood was collected and it was normal
Differential diagnosis
The possibility of cyanotic congenital heart disease was considered together with myocarditis to explain the congestive heart failure.
Treatment
The baby was discharged home on oral digoxin and diuretics .Currently, the baby is off medication.
Outcome and follow-up
The baby was discharged home haemodynamically stable, asymptomatic on full feeding.
He was being followed up in multidisciplinary clinics including a neonatologist, cardiologist and geneticist together with the neurodevelopmental clinic.
Discussion
Non-compaction cardiomyopathy is a myocardial disease characterised anatomically by deep trabeculations in the ventricular wall, producing endocardial recesses that communicate with the main ventricular chamber.1 In the early embryo; the heart is a loose interwoven mesh of muscle fibres that forms trabeculae with deep intertrabecular recesses. The myocardium gradually condenses and large spaces within the trabecular meshwork flatten. These large intertrabecular spaces transform into capillaries as the process of compaction occurs from the epicardium to the endocardium and from the base towards the apex, with trabecular compaction being more complete in the left ventricular than in the right ventricular myocardium. In the abnormal condition, the process of compaction arrests at an early stage, leaving numerous excessively prominent trabeculations and deep intertrabecular recesses in a segmental distribution usually from the apex.6
Ventricular non-compaction is a rare disease that affects mainly the left ventricle but can affect the right ventricle as well. There are controversies regarding the cause of right ventricle non-compaction due to the normally trabeculated shape of its walls. Non-compaction confined to only the right ventricle has never been reported.7
Non-compaction of the myocardium (NCM) was first described by Bellet in 1932. Two forms of NCM have been described with an isolated form and a form associated with congenital heart disease.8 Chin et al9, in 1990, described the condition and possibly attributed it to be a result of persistent embryonic myocardial morphology found in the absence of other cardiac anomalies that might explain this abnormal development.
No specific cause has been identified though familial occurrence has been reported.10 Non-compaction cardiomyopathy can be either sporadic or familial.11 Autosomal-dominant inheritance is more common than X linked inheritance or autosomal-recessive inheritance.12
NCM is rarely seen in other congenital cardiac disorders such as Ebstein's anomaly, bicuspid aortic valve, aorta-to-left ventricular tunnel, congenitally corrected transposition, isomerism of the left atrial appendage and ventricular septal defects.13 Ventricular non-compaction associated with Ebstein's malformation has rarely been reported.3
The clinical presentation is similar to that of other cardiomyopathies: systolic and diastolic left ventricular dysfunction, arterial embolism and tachyarrhythmias. The most common symptom is dyspnoea due to low cardiac output.2 Atrial and ventricular arrhythmias and thromboembolic events are suspected problems associated with the disease.14
The diagnosis of non-compacted cardiomyopathy is usually established by echocardiography, cardiovascular magnetic resonance imaging and CT. Left ventriculography is another imaging modality that may be diagnostic or may raise the initial clinical suspicion.
Left ventricular function may improve with treatment.12 The short-term prognosis may also be better in children who present in the neonatal period, as seen in our patient. Lilje illustrated in a series of 36 children with NCM (median age 90 days, range 1 day to 17 years at diagnosis) a good recovery.14 The death rate at 3 years was 14%. Some children who presented in the neonatal period had a transient recovery of function followed by later deterioration at 3–12 years that can lead to presentation in adulthood.15
Our case was the first reported neonate with combined non-compaction and Ebstein's. All the reported cases were with the median age, at diagnosis, 7–3.6 years.16 17
In our patient, no clear cause of cardiomyopathy was elicited. The outcome is favourably agreeing with the literature showing marked improvement of his cardiac function with normal growth and development.
Learning points.
Early detection is very important and helps in providing proper management in the accurate time.
Screening for the presence of associated condition is mandatory.
Counselling the parents about the natural history and mode of inheritance of the disease and its tendency to improve with time.
Counselling the parents about the outcome of the disease to anticipate all the adverse consequences.
Follow-up of these cases in a multidisciplinary approach.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Rigopoulos A, Rizos IK, Aggeli C. Isolated left ventricular noncompaction: an unclassified cardiomyopathy with severe prognosis in adults. Cardiology 2002;98:25–32. [DOI] [PubMed] [Google Scholar]
- 2.Pignatelli RH, McMahon CJ, Dreyer WJ. Clinical characterization of left ventricular noncompaction in children: a relatively common form of cardiomyopathy. Circulation 2003;108:2672–8. [DOI] [PubMed] [Google Scholar]
- 3.Attenhofer Jost CH, Connolly HM, Warnes CA, et al. Noncompacted myocardium in Ebstein's anomaly: initial description in three patients. J Am Soc Echocardiogr 2004;17:677–80. [DOI] [PubMed] [Google Scholar]
- 4.Sinkovec M, Kozelj M, Podnar T. Familial biventricular myocardial noncompaction associated with Ebstein's malformation. Int J Cardiol 2005;102:297–302. [DOI] [PubMed] [Google Scholar]
- 5.El-Menyar AA, Gendi SM, Mohammed T. Numan, noncompaction cardiomyopathy in the state of Qatar. Saudi Med J 2007;28:429–34. [PubMed] [Google Scholar]
- 6.Chatterjee S, Chakraborty A, Bodiwala K, et al. A review of ventricular non-compaction. The Internet Journal of Cardiovascular Research 2008;5(2) doi:10.5580/22d2. [Google Scholar]
- 7.Ritter M, Oechslin M, Sutsch G, et al. Isolated noncompaction of the myocardium in adults. Mayo Clin Proc 1997;72:26–31. [DOI] [PubMed] [Google Scholar]
- 8.Stollberger C, Finsterer J, Blazek G. Left ventricular hypertrabeculation/noncompaction and association with additional cardiac abnormalities and neuromuscular disorders. Am J Cardiol 2002;90:899–902. [DOI] [PubMed] [Google Scholar]
- 9.Chin TK, Perloff JK, Williams RG. Isolated noncompaction of left ventricular myocardium: a study of eight cases. Circulation 1990;8:507–13. [DOI] [PubMed] [Google Scholar]
- 10.Lorsheyd A, Cramer MJ, Velthuis BK, et al. Familial occurrence of isolated non-compaction cardiomyopathy. Eur J Heart Fail 2006;8:826–31. [DOI] [PubMed] [Google Scholar]
- 11.Sinkovec M, Kozelj M, Podnar T. Familial biventricular myocardial noncompaction associated with Ebsteins malformation. Int J Cardiol 2005;102:297–302. [DOI] [PubMed] [Google Scholar]
- 12.Murphy RT, Thaman R, Blanes JG. Natural history and familial characteristics of isolated left ventricular non-compaction. Eur Heart J 2005;26:187. [DOI] [PubMed] [Google Scholar]
- 13.Attenhofer Jost CH, Connolly HM, O'Leary PW. Left heart lesions in patients with Ebstein anomaly. Mayo Clin Proc 2005;80:361. [DOI] [PubMed] [Google Scholar]
- 14.Lilje C, Rázek V, Joyce JJ, et al. Complications of non-compaction of the left ventricular myocardium in a p ediatric population: a prospective study. Eur Heart J 2006;27:1855–60. [DOI] [PubMed] [Google Scholar]
- 15.Lofiego C, Biagini E, Pasquale F. Wide spectrum of presentation and variable outcomes of isolated left ventricular non-compaction. Heart 2007;93:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birgit J. Gerecke, günter breithardt isolated non-compaction cardiomyopathy. Dtsch Arztebl Int 2010;107:206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kádár K, Tóth A, Tóth L, et al. Noncompacted cardiomyopathy in infants and children. Clinical findings and diagnostic techniques. Orv Hetil 2010;151:659–64. [DOI] [PubMed] [Google Scholar]


