Abstract
Cutaneous tuberculosis constitutes an uncommon presentation of extrapulmonary tuberculosis, especially among immune-competent patients. Here, there is a report of a 38-year-old man who presented with non-pruritic skin plaques, caused by isoniazid-resistant Mycobacterium tuberculosis, over his buttock, inguinal area and earlobe.
Background
Cutaneous tuberculosis is a rare subset of extrapulmonary infection caused by Mycobacterium tuberculosis. More commonly, the disease begins by haematogenous or lymphatic spread of bacilli from a primary focus such as lung. However, the infection can be acquired by direct inoculation of bacilli into the skin.1 The clinical spectrum of cutaneous tuberculosis varies according to the degree of the host's cell-mediated immunity. Lupus vulgaris, tuberculosis verrucosa cutis, scrofuloderma and tuberculosis cutis orificialis are the prototypical example across the spectrum.2–4 The constellation of a patient's history, physical examination, histopathological study and mycobacteriology surveys help in diagnosis. Here, we report a case of a 38-year-old man who presented with skin plaques over earlobe, buttock and inguinal area caused by isoniazid-resistant strain of M tuberculosis.
Case presentation
An otherwise healthy 38-year-old man presented with several-week history of growing non-pruritic skin plaques over his left earlobe (figure lA), inguinal area (figure 1B) and buttock (figure 1C). He denied any history of fatigue, fever, night sweat or weight loss. He had no memory of injection or skin trauma over the involved areas. He was immune competent and did not complain of any respiratory symptoms. He received treatment for pulmonary tuberculosis when he was 5 year old.
Figure 1.

Well-demarcated skin plaques of tuberculosis over (A) ear lobe, (B) inguinal area and (C) buttock.
Investigations
On physical examination, he was reasonably well .There were well-demarcated scaly red skin plaques over his left earlobe, buttock and inguinal area. The lesion over the earlobe was somehow deforming. There were also bilateral freely moving, non-tender enlarged cervical nodes. Otherwise, the rest of the examination was unremarkable.
Tests of blood cell count, liver/renal function and electrolytes were all normal. Tuberculin test was reactive at 17 mm and erythrocyte sedimentation rate was 85 mm/h.
Skin biopsy of the earlobe lesion and excisional biopsy of cervical lymph nodes were done. Histopathological study of the samples revealed granulomatosis reaction without caseosis necrosis. Specimen staining for Mycobacterium and fungi was negative. The result of culture was pending. Mycobacterium, fungal infection, sarcoidosis and lymphoma were probable diagnoses. CT scan of thorax revealed mediastinal lymph adenopathies and old fibrotic scars in upper lobes and no evidence of active pulmonary tuberculosis (figure 2). CT scanning of abdomen did not show any evidence of enlarged lymph nodes, or hepatosplenomegaly. On the basis of the childhood history of tuberculosis, positive tuberculin test and histology of skin and lymph node biopsy, the most probable diagnosis was tuberculosis.
Figure 2.
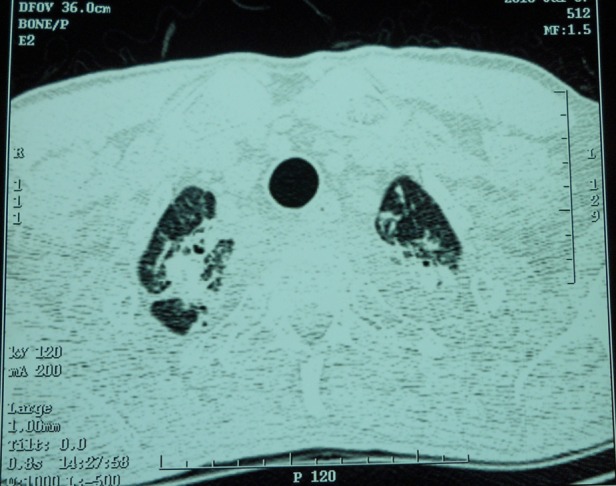
A section of thoracic CT scan showing fibrotic scars of old tuberculosis over both upper lobes.
Differential diagnosis
Mycobacterium, fungal infection, sarcoidosis and lymphoma.
Treatment
The patient received the regimen containing isoniazid, rifampin, ethambutol and pyrazinamide. Within a few weeks, cutaneous lesions and cervical lymph nodes started to shrink. Two months later, culture study of both skin and lymph node samples showed the growth of isoniazid-resistant M tuberculosis. Therefore, rifampin along with ethambutol and pyrazinamide were continued across the rest of the treatment. The total duration of treatment was 6 months.
Outcome and follow-up
No significant complication occurred during drug therapy and the lesions improved significantly (figure 3).
Figure 3.

The same earlobe lesion 6 months after completion of treatment showing significant improvement.
Discussion
Skin tuberculosis is a rare subtype of extra pulmonary tuberculosis. It is more commonly caused by haematogenous or lymphatic spread of bacilli from a distant focus such as lung. However, the direct inoculation of bacilli into the skin can induce the disease. The lesions present in different manners, giving rise to the various dermatological terms such as lupus vulgaris, tuberculosis verrucosa cutis, scrofuloderma and tuberculosis cutis orificialis. Tuberculosis verrucosa cutis is a rare form of skin tuberculosis with wart-like lesions, while tuberculosis cutis orificialis has a predilection for body orifices. The patient in this report had lupus vulgaris. Lupus vulgaris is one of the most common forms of cutaneous tuberculosis that mostly occurs in tuberculin-sensitive patients. Skin lesions are small soft reddish-brown papules that form sharply defined margin plaques that slowly evolved by peripheral extension and central atrophy. Lupus vulgaris can involve any site including face, head and neck, limbs and trunk. Limbs, head and neck are the most reported sites of involvement.1–5 Multiple site involvement are common as it was seen in our patient.6 There are patients with cutaneous tuberculosis who have internal organ tuberculosis at the same time. Lymphadenitis, musculoskeletal and pulmonary tuberculosis are more probable co-infections.7 The patient in this report has simultaneous cutaneous and cervical lymph node tuberculosis.
Diagnosis of cutaneous tuberculosis is almost challenging. The lesions are not pathognomic and resemble other dermatological entities such as sarcoidosis and fungal infections, so it may take several months or even years before true diagnosis. High clinical suspicion, microbiological and histopathological examinations are necessary for early diagnosis and treatment. Pathologically, the infection is associated with granulomatose inflammation. The quantity of bacilli encountered in cutaneous lesion is small and acid-fast staining of the samples is negative. Isolation of the bacilli in culture or positive PCR assay help in diagnosis.2–5
Cutaneous tuberculosis is treated like other forms of the tuberculosis and total duration of treatment is 6 months. According to the WHO guideline, the patient in this report received 6-month treatment with rifampin, ethambutol, and pyrazinamid. Isoniazid was discontinued because the isolated Mycobacterium was resistant to it.8 There are a few reports of cutaneous tuberculosis resistant to drugs of antitubercular treatment.9
Learning points.
Cutaneous tuberculosis may involve multiple sites simultaneously.
On the basis of similarity of lesions to fungal infections, sarcoidosis, foreign body reaction, a constellation of history, clinical findings and microbiological studies are necessary for timely diagnosis.
Patients may present with cutaneous tuberculosis and internal organ involvement at the same time.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Zadbuke S, Khan N, Set R, et al. Primary inoculation tuberculosis following a vehicular accident. Indian J Med Microbiol 2012;30:98–100. [DOI] [PubMed] [Google Scholar]
- 2.Thakur BK, Verma S, Hazarika D. A clinicopathological study of cutaneous tuberculosis at dibrugarh district, assam. Indian J Dermatol 2012;57:63–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puri N. A clinical and histopathological profile of patients with cutaneous tuberculosis. Indian J Dermatol 2011;56:550–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Afsar FS, Afsar I, Diniz G, et al. Lupus vulgaris in a pediatric patient: a clinicohistopathological diagnosis. Braz J Infect Dis 2008;12:152–4. [DOI] [PubMed] [Google Scholar]
- 5.Erbagci Z, Tuncel A, Bayram N, et al. Tuberculosis verrucosa cutis in a patient with long-standing generalized lichen planus: improvement of lichen after antitubercular polychemotherapy. J Dermatol Treat 2006;17:314–18. [DOI] [PubMed] [Google Scholar]
- 6.Rajan J, Mathai AT, Prasad PV, et al. Multifocal tuberculosis verrucosa cutis. Indian J Dermatol 2011;56:332–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukta V, Jayachandran K. Lung and lupus vulgaris. Lung India 2011;28:127–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis. Geneva, Switzerland: World Health Organization, 2006. [Google Scholar]
- 9.Wang H, Wu Q, Lin L, et al. Cutaneous tuberculosis: a diagnostic and therapeutic study of 20 cases. J Dermatol Treat 2011;22:310–14. [DOI] [PubMed] [Google Scholar]


