Abstract
Excessive yawning has been reported in the peri-ictal period preceding or following seizures. We describe an exceptional case of an elderly man with impairment of consciousness and paroxysmal excessive yawning. We hypothesise that this can be regarded as an autonomic seizure originating from diencephalic/brainstem structures, manifesting with yawning as an ictal phenomenon.
Background
Physiological yawning is a complex involuntary, paroxysmal movement, lasting 5–10 s, which occurs during the transition between wakefulness and sleep or sleep and wakefulness, as well as in response to fatigue, tiredness, stress, overwork, lack of stimulation, boredom, hunger or satiety. Yawning displays a stereotyped, synergistic, coordinated sequence of motions of the facial, oro-pharyngeal and respiratory muscles accompanied by the activity of the axial and limb extensor muscles1 and sympathetic activity inhibition that favours a parasympathetic dominance.2 Recently, it has been proposed that yawning is part of interoceptiveness because of its capacity to increase arousal and self-awareness.3 The James-Lange theory suggests that peripheral afferent signals coming from muscles and viscera provide feedback to the brain, which recognises and integrates them to create motivational state and arousal; accordingly, yawning provides bodily consciousness.
In humans, the existence of a putative yawning control system in the diencephalon/brainstem comes from brain lesion studies. There is agreement that the paraventricular nucleus (PVN) of the hypothalamus, the locus coeruleus and reticular activating system are primarily involved with yawning control.4 5 The PVN, which is the point of integration between central and peripheral autonomic systems and has connections to the hippocampus, pons, medulla and frontal lobe, seems to be the main control centre.
Human beings yawn with varying frequency, ranging between 0 and 28 in 24 h.3 Abnormal frequency variations have been described accompanying different clinical conditions.
Disappearance of yawning has been reported in Parkinson's disease,6 where it is thought to reflect the activity state of the D3 dopaminergic neurons of the PVN of the hypothalamus, which are necessary for yawning, and following treatment with neuroleptics.7 Excessive (pathological) yawning has been defined as a compulsive, repetitive, action not triggered by appropriate stimuli, and has been arbitrarily defined as more than three yawns in 15 min.8 Excessive yawning has been described in association with numerous clinical conditions including brain tumours,1 amyotrophic lateral sclerosis,9 brainstem stroke5 and acute anterior circulation stroke.8 Excessive yawning has also been reported in the peri-ictal period preceding or following seizures.10–13
We observed a case of an elderly man with yawning as the main ictal seizure manifestation.
Case presentation
An 86-year-old man presented with a history of decreased responsiveness and recurrent falls on a background of chronic general decline over 9 months. On hospital admission, investigations, including routine blood tests, 24 h ECG and blood pressure monitoring, showed no significant abnormalities. A moderate degree of cerebral cortical atrophy, but no space-occupying or vascular lesion, was noticeable on a CT scan. While on the ward, hospital staff observed the patient having episodes of appearing ‘absent’. A routine EEG (Xltek EEG System, Oakville, Ontario, Canada) was revealing and captured a clinical event. About 12 min after the recording started, the patient rested his head back on a pillow and appeared still; 8 min later, the patient became unresponsive. During the period of unresponsiveness, which lasted 14 min, clusters of yawns or single yawning episodes were the most striking manifestation. During this period, the EEG showed diffuse electrodecremental activity (figure 1); a lead II ECG showed a reduction in heart rate (mean 73 beats/min, compared to mean 93 beats/min before and after the event). There was no clinical or EEG response to external (visual, auditory, tactile and painful) stimulation. Upon cessation of this event, as the patient became alert and responsive, the EEG returned to the original resting state.
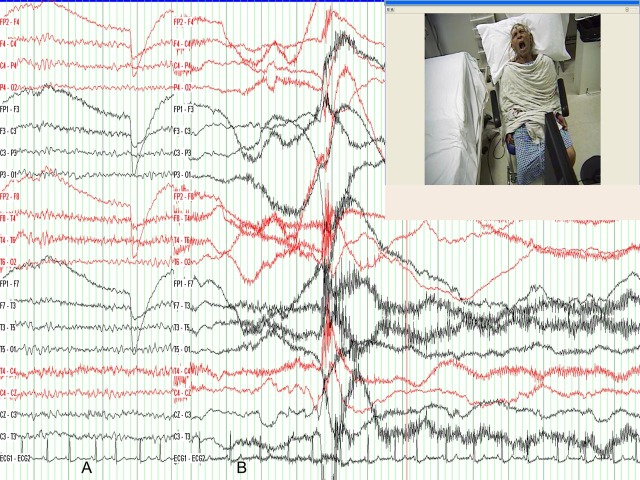
Figure 1.
Patient's EEG traces (Parasagittal, Temporal, Central (PTC) PTC montage). (A) Shows 5 s of EEG background activities with 7–8 Hz posterior rhythm poorly responding to eye opening. This is compatible with the patient's moderate degree of cerebral cortical atrophy. (B)Shows the EEG during one of the ictal yawning episodes while the patient was unresponsive. Superimposed upon the electrodecremental activity there are prominent muscle artefacts due to yawning movements.
The patient was started on sodium valproate, with a good clinical response: episodes of appearing absent were no longer reported during the period near to hospital discharge.
Unfortunately, in the longer term follow-up period, the patient's general physical condition declined markedly, with superadded intervening clinical depression so that the patient's relatives found not possible to report any of those episodes.
Investigations
The key investigation was a routine EEG, as it revealed changes occurring during a clinical event. In fact, while the patient was unresponsive, the EEG showed diffuse electrodecremental activity; this abnormal activity was different compared to the background activity before and after the clinical event. Hence, the EEG, showing abnormal activity accompanying the clinical event, was instrumental in guiding the diagnosis.
Differential diagnosis
Excessive yawning can occur in association with clinical conditions such as brain tumours, brainstem stroke, acute anterior circulation stroke; however, our patient brain scan showed no space-occupying or vascular lesion. Our patient had no other neurological diseases such as multiple sclerosis, amyotrophic lateral sclerosis or migraine, conditions that have been described in association with excessive yawning. Our patient had a history of recurring episodes of decreased responsiveness/appearing absent; we captured one of these events, during which excessive yawning occurred; for the duration of this event, there were accompanying EEG changes. All these features together are strongly suggestive of a seizure disorder. Because of the patient's change in level of alertness (indicating brainstem involvement), the paroxysmal yawning (with a putative yawning centre in the brainstem) and the EEG electrodecremental pattern (considered an EEG seizure pattern of brainstem origin14), we suggest that a seizure originating from the brainstem structure is the most likely mechanism underlying our patient's event.
Discussion
This is an exceptional case of prolonged seizure with impairment of consciousness and paroxysmal yawning. We hypothesise that this can be regarded as an autonomic seizure originating from diencephalic/brainstem structures, manifesting with yawning as an ictal phenomenon.
Seizures accompanied by excessive yawning in the peri-ictal period have been described. Penfield and Jasper10 were the first to report peri-ictal yawning in two patients with autonomic diencephalic seizures (but they did not mention EEG). Peri-ictal yawning has been observed in a child with infantile spasm, with the EEG showing generalised decremental activity.11 Also, peri-ictal yawning has been described in patients with temporal lobe epilepsy, with yawning preceding complex partial seizures (CPS) and EEG showing interictal epileptiform discharges,12 or with yawning during the post-ictal period following CPS with or without secondary generalisation and EEG showing interictal epileptiform discharges.12 13
To the best of our knowledge, there is only one reference that describes a significant association between ictal yawning and 3 Hz spike and wave discharges.15 Golgie and Green studied a 7-year-old girl with petit mal; the frequency of her seizures was 1 in 15 min, although it could drop to 2/day. The girl was observed during a prolonged EEG recording. They found that in 40 h of total recording there were 351 yawns: 80 (23%) occurred during attacks and 271 (77%) occurred during the resting periods; of the 80 yawns which occurred during attacks, 27 (34%) occurred during spike and wave discharges and 53 (66%) occurred coincident with the onset or 20 s preceding the onset of spike and wave discharges.
We reported the case of an elderly patient with yawning as the main ictal phenomenon during a prolonged period of unresponsiveness. In 37 min of total EEG recording, 10 yawns were observed, all of them occurring during the 14 min of unresponsiveness. Most likely, this could be an autonomic complex partial seizure arising from diencephalic/brainstem structures with paroxysmal yawning. Cattaneo et al5 reported two cases of brain stem stroke, with lesions confirmed by MRI presenting with transient excessive pathological yawning; the authors hypothesised that the pathogenesis of excessive yawning could be due to denervation hypersensitivity of a putative brainstem yawning centre. In our case, no identifiable brainstem lesion was visible at brain imaging. However, the involvement of brainstem structures is unquestionable, considering the patient's change in the level of alertness (unresponsiveness) and the paroxysmal yawning. Nevertheless, neocortical brain areas have a regulatory effect on diencephalic and brainstem yawning centres, as excessive yawning can occur in supratentorial stroke.8 A neocortical contribution to the excessive yawning in our case cannot be ruled out. Moreover, the ictal EEG changes (electrodecremental activity) observed during the event in our patient are different than those (spike and wave discharges) reported by Golgie and Green. Diffuse electrodecremental activity is considered an EEG seizure pattern of possible brainstem origin,14 further corroborating our hypothesis that our report could be an exceptional case of a seizure originating from brainstem structures.
Our report is an addition to the previous ones on excessive yawning and emphasises the importance of this clinical pathological manifestation in the elderly.
Learning points.
Routine EEG can be instrumental in guiding diagnosis.
Excessive yawning can be an ictal seizure manifestation in the elderly.
Seizure originating from autonomic structures should be recognized.
Acknowledgments
Dr Paul Strutton is acknowledged for his help.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Barbizet J. Yawning. J Neurol Neurosurg Psychiatry 1958:21:203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Askenasy JJ, Askensy N. Inhibition of muscle sympathetic nerve activity during yawning. Clin Auton Res 1996;6:237–9. [DOI] [PubMed] [Google Scholar]
- 3.Walusinski O. Yawning: unsuspected avenue for a better understanding of arousal and interoception. Med Hypotheses 2006;67:6–14. [DOI] [PubMed] [Google Scholar]
- 4.Walusinski O. Yawning in diseases. Eur Neurol 2009;62:180–7. [DOI] [PubMed] [Google Scholar]
- 5.Colosimo C, Pontieri FE. Yawning in Parkinson's disease. Neurology 1999;52:428. [PubMed] [Google Scholar]
- 6.Cattaneo L, Cucurachi L, Chierici E, et al. Pathological yawning as a presenting symptom of brain stem ischaemia in two patients. J Neurol Neurosurg Psychiatry 2006;77:98–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mogilnicka E, Klimek V. Drugs affecting dopamine neurons and yawning behaviour. Pharmacol Biochem Behav 1977;7:303–5. [DOI] [PubMed] [Google Scholar]
- 8.Singer OC, Humpich MC, Lanfermann H, et al. Yawning in acute anterior circulation stroke. J Neurol Neurosurg Psychiatry 2007;78:1253–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams DR. The yawning reflex: an upper motor neuron sign in amyotrophic lateral sclerosis. Neurology 2000;55:1592–3. [DOI] [PubMed] [Google Scholar]
- 10.Penfield W, Jasper H. In: Epilepsy and the functional anatomy of the Human Brain. Boston, MA: Little, Brown & Co, 1954:416–18. [Google Scholar]
- 11.Donat JF, Wright FS. Unusual variants of infantile spasms. J Child Neurol 1991;6:313–18. [DOI] [PubMed] [Google Scholar]
- 12.Muchnik S, Finkielman S, Semeniuk G, et al. Yawning and temporal lobe epilepsy. Medicina (B Aires) 2003;63:137–9; (Spanish). [PubMed] [Google Scholar]
- 13.Yankovsky AE, Andermann F, Dubeau F. Video case report post-ictal forceful yawning in a patient with nondominant hemisphere epilepsy. Med Hypotheses 2006;67:6–14. [PubMed] [Google Scholar]
- 14.Gastaut H, Roger J, Ouahchi S, et al. An electroclinical study of generalize epileptic seizures of tonic expression. Epilepsia 1963;4:15–44. [DOI] [PubMed] [Google Scholar]
- 15.Goldie L, Green JM. Yawning and epilepsy. J Psychosom Res 1961;5:263–8. [DOI] [PubMed] [Google Scholar]