Abstract
Myxofibrosarcoma (MFS) also known as myxoid variant of malignant fibrous histocytoma is one of the most common soft tissue sarcomas of the extremities in adult and elderly patients with rare occurrences in head and neck region. Low-grade MFS is unusual among low-grade sarcomas because it often recurs relentlessly and multiplies despite wide local resection with gross negative margins. We report a case of extreme rarity and a tumour of aggressive nature in the maxillary sinus, which presented with non-specific sinonasal symptoms and we present a review of the radiological and histopathological characteristics of this rare tumour and recent evidence of management.
Background
Low-grade myxofibrosarcoma (LGMFS) is unusual among low-grade sarcomas because it often recurs relentlessly and multiplies after surgical resection, despite gross negative margins and wide surgical resection.
We reported a case of extreme rarity, a tumour of aggressive nature in the maxillary sinus, which presented with non-specific sinonasal symptoms. Awareness and high index of suspicion among clinicians is vital. Early detection of these fatal tumours can change the morbidity of the surgery and attain the patient remission and excellent prognosis. The diagnosis of sinusitis is mainly clinical and straightforward (nasal congestion/blockage, rhinorrhoea/postnasal drip, smell disorder and facial pain/discomfort) and any unusual presentation or atypical symptoms such as severe or prolonged facial pain, numbness or hyperesthesia, loose denture, double vision, proptosis and epistaxis must draw the attention of a clinician to more sinister possibility.
Case presentation
A 50-year-old lady of middle-eastern origin presented to our department with a 2-month history of left chronic sinus pain associated with left-sided toothache. Initial assessment showed a minimal symptomatic relief despite the use of repeated courses of antibiotic, analgesia and topical nasal steroids prescribed earlier by her doctor and local dentist. On examination, a mild proptosis in the left eye was noticed associated with a 3 mm inferior scleral show in upper gaze with diplopia. Endoscopic nasal examination was unremarkable. A full otolaryngological examination was normal.
Investigations
An urgent CT scan of the paranasal sinuses illustrated a large mass of mixed attenuation and enhancement filling the left maxillary sinus with expansion into left inferior orbital wall. The mass had eroded superiorly into the lamina papyracea and the posterolateral wall of the sinus. There was also erosion of the left maxillary alveolus, which could explain for her dental complaint (figure 1).
Figure 1.
Coronal CT section.
An MRI scan confirmed the findings of the CT scan and excluded both pterygopalatine soft tissue extension and orbital periosteum involvement (figure 2). CT imaging of the neck and chest were both clear. Haematology and chemistry studies were all normal. Endoscopic examination under anaesthesia later on showed bowing of the lateral nasal wall in the inferior meatus with a normal looking middle meatus (figures 3 and 4); hence, several biopsies taken from inferior turbinate, meatus and maxillary sinus through the inferior antrostomy.
Figure 2.
MRI scan T1 axial section.
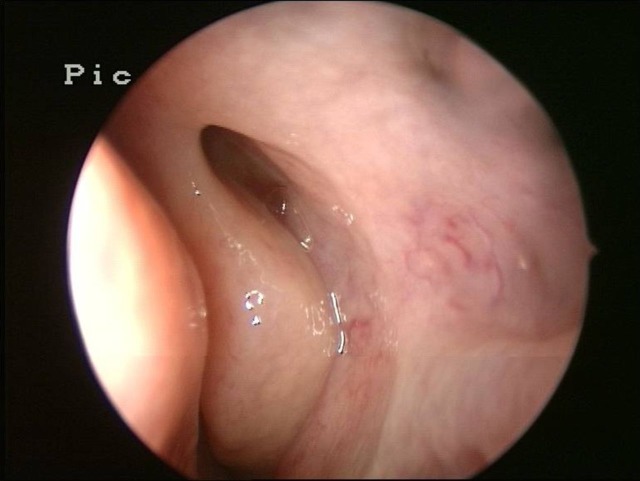
Figure 3.
Endoscopic view of middle meatus.
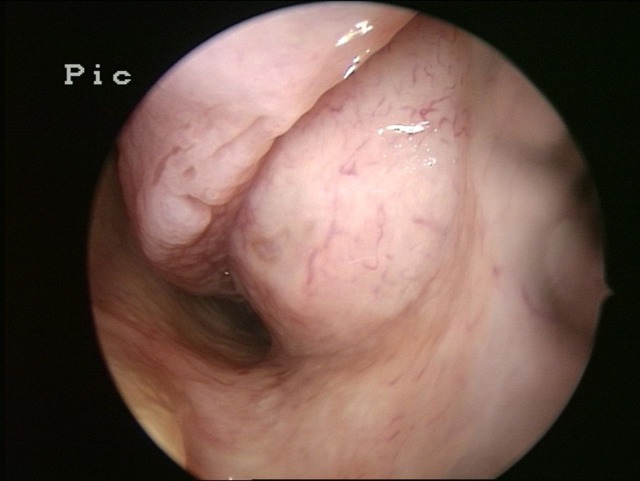
Figure 4.
Endoscopic view of the left inferior meatus.
Diagnostic histology featured spindle-shaped and stellate cells with poorly defined cytoplasm and pleomorphic nuclei, in a myxoid stroma. There were thin-walled curvilinear vessels within the tumour. The mitotic index is 1–2/10 high-power field. Necrosis was not identified. Scattered lymphocytes, plasma cells and mast cells were noted. Immunostaining showed that the spindle cells did not express DESMIN, SMA, EMA, CD68 or S100. Scattered CD68 positive monocytes/macrophages cells were present (figures 5 and 6).
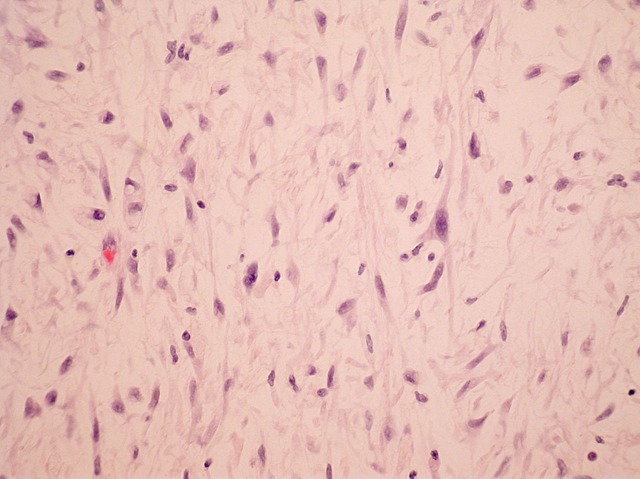
Figure 5.
Macroscopic view.
Figure 6.
Microscopic view.
Differential diagnosis
Sinonasal tumour
Rhinosinusitis
Nasal polyps
Teeth root retention
Dental infection
Silent sinus syndrome
Treatment
The lesion was excised en-bloc (maxillectomy with orbital preservation) via midfacial degloving approach and all margins were clear of the disease. Patient was referred afterwards for adjuvant radiotherapy. However, in last December, the patient had another craniofacial procedure to extirpate recurrent disease.
Outcome and follow-up
The recovery with each procedure was uneventful and she currently remains on regular review under a multidisciplinary team as part of head and neck cancer surveillance monitoring.
Discussion
LGMFS is slow growing and rarely leads to distant metastases. But the local recurrence rate of the low-grade type is as high (50–60%) as that of the high-grade type. The middle-aged and elderly are most commonly affected (1)1 with an approximately equal incidence in men and women.2 Regions affected by the tumour as published in various series showed that the most common site was the lower limb (57%), followed by the upper limb (31%), trunk (8%) and lastly head and neck (4%).3
LGMFS in the sinonasal tract usually exhibits features similar to other soft tissue neoplasms, namely epistaxis, rhinorrhea, nasal obstruction and non-specific nasal discomfort. However, there are no distinguishing physical signs to LGMFS.4
Findings pertain to the relatively smooth surface of the tumour and its uniform density or no necrotic area; the clear separation of the tumour from the surrounding soft tissues on the CT images.5 A poor periosteal reaction to the tumour invasion; that is an osteolytic bone change was also noticed in some cases.
LGMFS showed a myxoid component, which is defined on MRI as a lesion showing hypointense T1-weighted and extrahyperintense T2-weighted signals. The presence of an increased perifacial T2 signal is characteristic in myxofibrosarcoma. Fluid level might be present in some cases.6 The infiltrative growth pattern may be obvious in gadolinium-enhanced fat-suppressed T1-weighted images even in tumour with focal growth pattern. In addition, diffusion-weighted imaging can improve assessment of infiltration with myxofibrosarcoma.6
Tumour cells of myxofibrosarcoma are likely to be derived from fibroblastic and primitive mesenchymal cells rather than from a histiocytic lineage.7
Myxofibrosarcoma were graded according to the system proposed by Mentzel et al.7 All tumours showed a broad spectrum of histological grade characterised as low, intermediate and high. The principle feature shared by all tumours of any grade was a varying proportion of hypocellular myxoid and cellular areas, the myxoid areas being more prominent in lower-grade lesions.
Macroscopically (figure 5) the resected tumour is very soft and well circumscribed. Its cut surface is uniformly gelatinous and yellow-grey in colour.8 Microscopically (figure 6), myxofibrosarcoma compromises a continuous range from hypocellular tumours, consisting of small spindle cells widely spaced among the myxoid matrix, to more cellular variants with pleomorphic nuclei and pseudolipoblasts.
LGMFS must be distinguished from other benign and malignant mesenchymal lesions with a prominent myxomatous matrix. It is also prone to misinterpretation as other benign or malignant myxoid mimickers such as myxoid liposarcomas, Low-grade fibromyxoid sarcomas (FMSs), cellular myxomas, nodular fasciitis, myxoid neurofibroma, myxoma and superficial angiomyxoma.4 8 LGMFS and low-grade FMS are two distinct entities in the spectrum of myxoid mesenchymal sarcomas with fibroblastic differentiation. Low-grade FMS is characterised by an indolent but ultimately malignant clinical course with metastases in more than half of the cases, which underlines the importance of distinguishing between the two entities.
The capacity of lower-grade lesions to advance in histological grade underpins the necessity for accurate diagnosis and adequate excision of these lesions, especially because tumours that are purely low grade seem to have little or no potential for metastasis and are therefore potentially curable. LGMFS demonstrates a high rate of local recurrence if treated inappropriately. Low-grade lesions often become higher grade in subsequent recurrence and acquire metastatic potential. Therefore, tumour resection with wide surgical margin is critical for disease cure.6 However, achieving a complete resection with wide margins is generally not possible in the head and neck region.
Adjuvant radiotherapy is usually reserved for recurrent, unresectable or large lesion with high chance of microscopic tumour involvement of the margin, its efficacy is controversial.4 Fayda et al9 in their study showed that there is no difference in local control between patients with negative or microscopically positive disease if they receive postoperative radiotherapy. Regarding overall survival, median survivals of patients receiving both surgery and radiotherapy with negative and microscopically positive margins were significantly better than patients who were not treated with surgery.9 Therefore, the treatment strategy is a combination of surgical excision and radiotherapy. The goal of surgery is to obtain tumour-free margins of 1–3 cm.10 11
Chemotherapy has been used for the treatment of myxofibrosarcoma, but the results are poor. Likewise, the use of adjuvant chemotherapy does not significantly affect local control. Zagars et al10 found no evidence that adjuvant chemotherapy decreased the metastatic or local recurrence rates.
The overall 5-year and 10-year survival rates for LGMFS are 65% and 52%, respectively.12 Patient age, tumour size (>5 cm), histological grade, positive section margin and deep-seated tumours are all poor prognostic factors for various soft tissue sarcomas of the head and neck and significantly associated with poor overall survival.13 14
Learning points.
Rare and potentially fatal tumours can give few or no symptoms in clinical context; hence, high index of suspicion is very important in all cases of unusual presentation or failure of responding to empiric treatment.
Sinonasal pain is unusual in cases of chronic sinusistis. Patients with assumed sinus infection (nasal congestion/blockage, rhinorrhoea/postnasal drip, smell disorder and facial pain) should be diagnosed and treated according to the sinusitis protocol. Any unresponsiveness or failure should be dealt with by referring the patient to the specialist.
Rare sarcoma proved to be difficult to diagnosis clinically, radiologically and histologically.
Low-grade myxofibrosarcoma is rare and very aggressive tumour, hence early intervention is important.
Early referral to the specialist is necessary, if the clinical presentation is unusual.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Fang ZW, Chen J, Teng S, et al. Analysis of soft tissue sarcomas in 1118 cases. Chin Med J (Engl) 2009;122:51–3. [PubMed] [Google Scholar]
- 2.Mentzel T, Calonje E, Wadden C, et al. Myxofibrosarcoma. Clinicopathologic analysis of 75 cases with emphasis on the low-grade variant. Am J Surg Pathol 1996;20:391–405. [DOI] [PubMed] [Google Scholar]
- 3.Huang HY, Lal P, Qin J, et al. Low-grade myxofibrosarcoma: a clinicopathologic analysis of 49 cases treated at a single institution with simultaneous assessment of the efficacy of 3-tier and 4-tier grading systems. Hum Pathol 2004;35:612–21. [DOI] [PubMed] [Google Scholar]
- 4.Lam PK, Trendell-Smith N, Li JH, et al. Myxofibrosarcoma of the sphenoid sinus. J Laryngol Otol 2002;116:464–6. [DOI] [PubMed] [Google Scholar]
- 5.Sato T, Kawabata Y, Morita Y, et al. Radiographic evaluation of malignant fibrous histiocytoma affecting maxillary alveolar bone: a report of 2 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:116–23. [DOI] [PubMed] [Google Scholar]
- 6.Kaya M, Wada T, Nagoya S, et al. MRI and histological evaluation of the infiltrative growth pattern of myxofibrosarcoma. Skeletal Radiol 2008;37:1085–90. [DOI] [PubMed] [Google Scholar]
- 7.Mentzel T, Katenkamp D, Fletcher CD. Low malignancy myxofibrosarcoma versus low malignancy fibromyxoid sarcoma. Distinct entities with similar names but different clinical course . Pathologe 1996;17:116–21. [DOI] [PubMed] [Google Scholar]
- 8.Udaka T, Yamamoto H, Shiomori T, et al. Myxofibrosarcoma of the neck. J Laryngol Otol 2006;120:872–4. [DOI] [PubMed] [Google Scholar]
- 9.Fayda M, Aksu G, Yaman Agaoglu F, et al. The role of surgery and radiotherapy in treatment of soft tissue sarcomas of the head and neck region: review of 30 cases. J Craniomaxillofac Surg 2009;37:42–8. [DOI] [PubMed] [Google Scholar]
- 10.Zagars GK, Mullen JR, Pollack A. Malignant fibrous histiocytoma: outcome and prognostic factors following conservation surgery and radiotherapy. Int J Radiat Oncol Biol Phys 1996;34:983–94. [DOI] [PubMed] [Google Scholar]
- 11.Zagars GK, Ballo MT, Pisters PW, et al. Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer 2003;97:2530–43. [DOI] [PubMed] [Google Scholar]
- 12.Merck C, Angervall L, Kindblom LG, et al. Myxofibrosarcoma. A malignant soft tissue tumor of fibroblastic-histiocytic origin. A clinicopathologic and prognostic study of 110 cases using multivariate analysis . Acta Pathol Microbiol Immunol Scand Suppl 1983;282:1–40. [PubMed] [Google Scholar]
- 13.de Bree R, van der Valk P, Kuik DJ, et al. Prognostic factors in adult soft tissue sarcomas of the head and neck: a single-centre experience. Oral Oncol 2006;42:703–9. [DOI] [PubMed] [Google Scholar]
- 14.Wang CP, Chang YL, Ting LL, et al. Malignant fibrous histiocytoma of the sinonasal tract. Head Neck 2009;31:85–93. [DOI] [PubMed] [Google Scholar]