Abstract
An 83-year-old lady with type 2 diabetes mellitus was admitted to hospital with pneumonia. After 3 days of oral amoxicillin she developed ballism-choreiform movements of all four limbs. Her serum glucose and osmolality were raised. She had no factors suggestive of genetic or iatrogenic causes. A CT scan of the brain revealed bilateral putamen hyperintensities. She was started on tetrabenazine and subcutaneous insulin, which led to complete resolution of her symptoms.
Background
This case highlights the need for clinicians to be aware that, although rare, hyperosmolar non-ketotic hyperglycaemia (HONK) is an important cause of ballismus and should be considered even when the findings are bilateral. Simple, inexpensive assessment of blood capillary glucose should be considered in all patients with ballismus as early detection and treatment can lead to rapid and effective symptomatic relief and complete long-term recovery.
Case presentation
An 83-year-old lady with a history of diet-controlled type 2 diabetes mellitus, ischaemic heart disease, coronary artery bypass graft, hypertension, chronic kidney disease, gout and fractured neck of her right femur was admitted to a district general hospital with reduced mobility over the preceding week. A chest X-ray revealed cardiomegaly and left basal shadowing; she was diagnosed with a lower respiratory tract infection and was subsequently started on a course of oral amoxicillin.
Blood glucose was found to be raised on admission to the medical assessment unit with levels above 20 mmol/l, and so she was started on a regular dose of gliclazide.
On day 4 of admission she developed ballism-choreiform movements of all four limbs with involvement of the facial muscles. Her Glasgow coma score remained unaltered at 15/15 and she had no cognitive impairment. Neurological examination was otherwise normal.
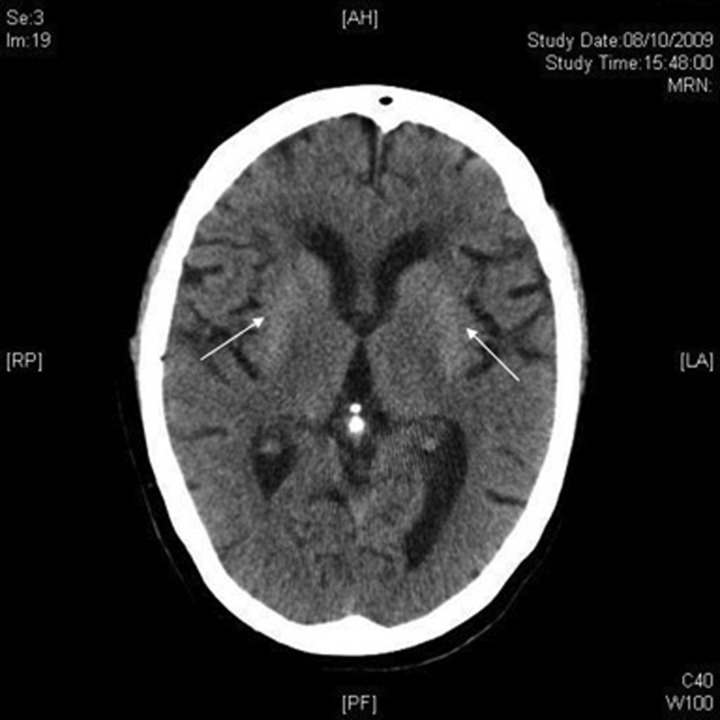
There was no family history of Huntington's disease and she was not on any medication known to cause ballismus or chorea. Her hyperglycaemia had proved difficult to control using oral pharmacotherapy with a persistent hyperglycaemia of 25.3 mmol/l and a raised serum osmolality of 309 mOsm/l. A CT scan of the brain revealed periventricular white matter changes consistent with ischaemic changes due to small vessel disease but no recent infarct or haemorrhage. The scan also reported bilateral putamen hyperintensities (figure 1).
Figure 1.
CT head scan demonstrating bilateral putamen hyperintensities (white arrows).
The working diagnosis at this stage was bilateral ballismus secondary to HONK. The patient was started on a regular regimen of long-acting and short-acting insulin in addition to maximisation of her gliclazide dose at 160 mg twice daily. Tetrabenazine was also started at a dose of 12.5 mg three times daily in addition to intravenous lorazepam at a dose of 2 mg when required, which provided short-term symptomatic relief.
The ballistic movements improved with correction of her blood glucose levels although she experienced significant tiredness and lethargy, which was thought to be secondary to the tetrabenazine. This was reduced to 12.5 mg twice daily before being discontinued completely. She was eventually discharged from hospital on a regular subcutaneous insulin course with complete resolution of her ballism-choreiform movements.
Discussion
Ballismus usually presents as a unilateral disorder termed ‘hemiballismus’ but may rarely be bilateral. The vast majority of patients presenting with hemiballismus will have a lesion in the contralateral subthalamic nucleus,1–4 which is most often caused by stroke (ischaemic or haemorrhagic).1 5 A wide range of pathological processes can cause ballismus. The largest cohort described in the literature is from a retrospective study in 1994 in which all patients presenting to a neurology department with hemiballismus or biballismus over a 10-year period were screened. Twenty-five patients were identified; in 16 patients ischaemic stroke was either confirmed or considered to be the likely cause of the movement disorder. One further patient presented with hemiballismus secondary to a transient ischaemic attack and two additional patients presented with intracerebral haemorrhage. There were two cases of basal ganglia calcification, one as a result of tuberous sclerosis. There were also single presentations of hemiballismus secondary to encephalitis, Sydenham's chorea, central nervous system lupus and one case of HONK.5
The clinical picture in ballismus secondary to HONK is an abrupt onset of ballism-chorea associated with a raised serum glucose level and serum osmolality.2–8 There may also be involvement of facial muscles.2 5 Cerebral imaging may reveal a hyperdense area within the basal ganglia on the contralateral side to the symptoms2–4 8 or bilaterally.2 3 6 8 MRI and single-photon emission computer tomography studies may demonstrate hyperintensity3 4 6 8 and hypoperfusion3 in the basal ganglia, respectively. The first reported autopsy study of a patient presenting with hyperglycaemic ballismus demonstrated multiple lacunar infarcts associated with a proliferation in hypertrophic astrocytes.7 The prognosis of this syndrome is good, with the majority of patients achieving symptom resolution with control of serum glucose levels2–6,8 and antidopaminergic or dopamine-depleting agents such as tetrabenazine.4
Learning points.
Hyperosmolar non-ketotic hyperglycaemia (HONK) is an important cause of ballismus which may present unilaterally or bilaterally
CT, MRI and single-photon emission computer tomography imaging produces characteristic changes
Prompt treatment of the underlying metabolic abnormality can lead to a resolution of symptoms and excellent clinical outcome
The use of tetrabenazine may be useful in symptom control during the acute stage of the illness
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Riley DE, Lang AE. Movement disorders. In: Bradley WG, Daroff RB, Fenichel GM, et al. eds. Neurology in clinical practice. Woburn, MA: Butterworth-Heinemann, 2000:1913–17. [Google Scholar]
- 2.Lin JJ, Chang MK. Hemiballism-hemichorea and non-ketotic hyperglycaemia. J Neurol Neurosurg. 1994;57:748–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai PH, Tien RD, Chang MH. Chorea-ballismus with nonketotic hyperglycemia in primary diabetes mellitus. Am J Neuroradiol 1996;17:1057–64. [PMC free article] [PubMed] [Google Scholar]
- 4.Sitburana O, Ondo WG. Tetrabenazine for hyperglycemic-induced hemichorea-hemiballismus. Mov Disord 2006;21:2023–5. [DOI] [PubMed] [Google Scholar]
- 5.Vidaković A, Dragasević N, Kostić VS. Hemiballism: report of 25 cases. J Neurol Neurosurg 1994;57:945–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boughammoura-Bouatay A, Chebel S, Younes-Mhenni S, et al. Biballism due to non-ketotic hyperglycaemia. Diabetes Metab 2008;34:617–19. [DOI] [PubMed] [Google Scholar]
- 7.Ohara S, Nakagawa S, Tabata K, et al. Hemiballism with hyperglycemia and striatal t1-mri hyperintensity: an autopsy report. Mov Disord 2001;16:521–5. [DOI] [PubMed] [Google Scholar]
- 8.Lee BC, Hwang SH, Chang GY. Hemiballismus-hemichorea in older diabetic women: a clinical syndrome with MRI correlation. Neurology 1999;52:646–8. [DOI] [PubMed] [Google Scholar]