Abstract
The vast majority of intracardiac thrombi of the patients with atrial fibrillation (AF) are reported to be in the left atrial appendage, which is thought to be an annual 6% to 10% risk. AF is responsible for 10% of ischaemic stroke. There have been few reports about the pulmonary vein thrombi. 64-Multidetector CT (64-MDCT) scan has recently become an optional diagnostic method for the assessment of coronary artery plaque. This study shows the pulmonary vein thrombus by 64-MDCT scan. The patient was a 79-year-old man and had hypertension, chest pain and no AF. 64-MDCT scan demonstrated 17.2×1.2×1.3 mm thrombus in the proximal side of the left upper pulmonary vein (LUPV). The distal portion of thrombus was seen to be attached to the wall of LUPV. This is the first report to show the pulmonary vein thrombus of the patient with hypertension, chest pain and no AF.
Background
The most common arrhythmias encountered in clinical practice are atrial fibrillation (AF), which prevalence has been known to be 1 to 2% in the general population.1 The patients with AF have an annual 6 to 10% risk and are responsible for 10% of all ischaemic strokes and half of all cardioembolic stroke.2 3 According to postmortem and echocardiographic studies, most of intracardiac thrombi are generated in the left atrial appendage (LAA) in patients with non-valvular AF.4 Transoesophageal echocardiography (TEE) is a usual tool to detect LAA thrombi. However, there have been reported little cases about pulmonary vein thrombi. 64-Multidetector CT (64-MDCT) scan has recently become an optional diagnostic method for the assessment of coronary artery plaque. More recently, 64-MDCT has been shown to be a useful optional tool to assess the LAA thrombi. Especially, 64-MDCT has the strong merit when 64-MDCT assesses the spacial structure of LAA thrombi.5
This study showed the pulmonary vein thrombus of the patient without AF by 64-MDCT.
Case presentation
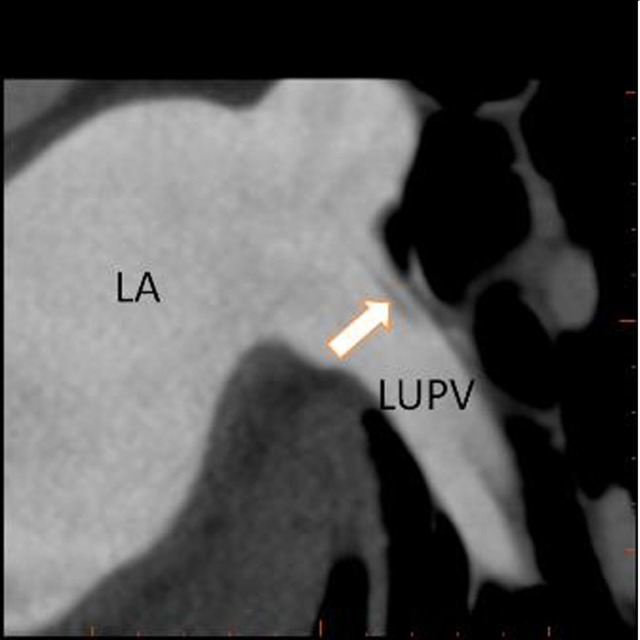
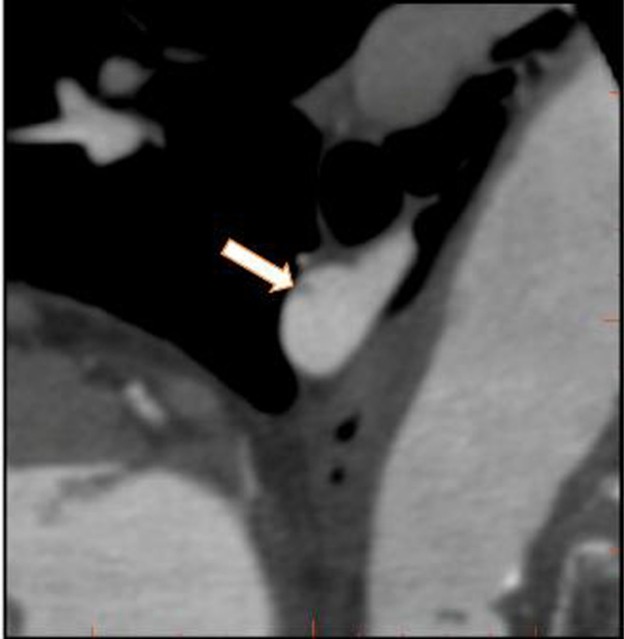
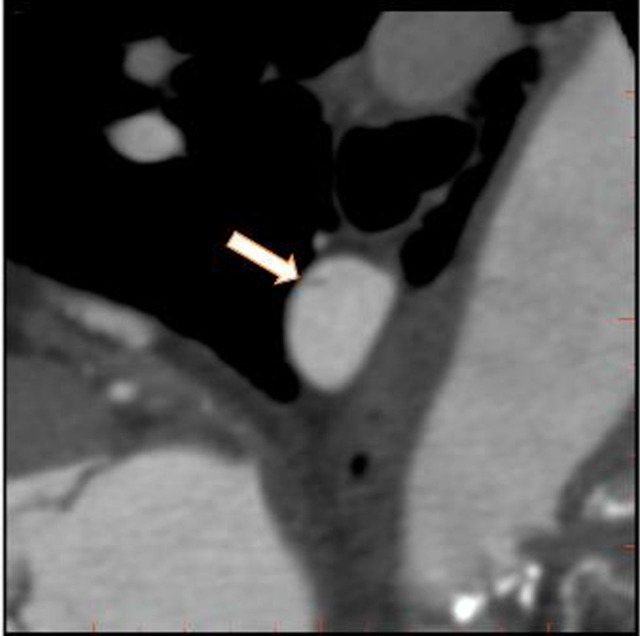
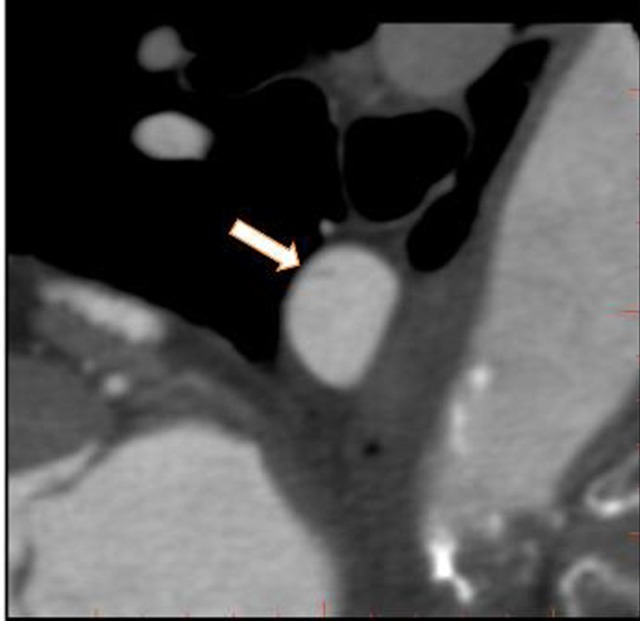
The patient was a 79-year-old man and had hypertension and chest pain. He was referred to our hospital for the evaluation of chest pain. He was treated with hypertension only and no previous treatment with anticoagulant had been performed. 64-MDCT scan demonstrated that 17.2×1.2×1.3 mm thrombus was situated at the proximal side of left upper pulmonary vein (LUPV) (figure 1; axial, figures 2 to 4; sagittal) and calcification of left anterior descendant (LAD; #6 and #7). And 64-MDCT demonstrated no thrombus in LAA. The distal portion of thrombus was seen to be attached to the wall of the LUPV (figure 2). The area attached to the wall of LUPV decreased (figure 3). The distal portion of thrombus was seen to separate from the wall of the LUPV (figure 4).
Figure 1.
Axial image showing a thrombus (17.2 to 1.2 mm) within the LUPV (white arrow). LUPV, left upper pulmonary vein, LA, left atrium.
Figure 2.
Sagittal image showing a thrombus (1.1 to 1.3 mm) within the left upper pulmonary vein (LUPV) (white arrow). The distal portion of thrombus was seen to be attached to the wall of the LUPV.
Figure 3.
Sagittal image showing a thrombus (1.0 to 1.4 mm) within the left upper pulmonary vein (LUPV) (white arrow). The distal portion of thrombus was seen to be attached to the wall of the LUPV. The area attached to the wall of LUPV decreased.
Figure 4.
Sagittal image showing a thrombus (1.2 to 1.3 mm) within the left upper pulmonary vein (LUPV) (white arrow) before warfarin therapy. The distal portion of thrombus was seen to separate the wall of the LUPV.
Discussion
This study showed the strong merit of 64-MDCT is that it can estimate 3D structure of the heart and the pulmonary vein. It has been established that appropriate tool for detection of intracardiac thrombus is TEE, but TEE cannot demonstrate most part of the pulmonary vein via being inhibited by pulmonary air. 64-MDCT can demonstrate the pulmonary vein completely, so we can identify the small thrombus like that in the present study.
Although there are numerous studies showing that a significant relationship exists between stroke and AF, there is little information, to our best knowledge, in the relationship between stroke and the pulmonary vein thrombi and/or LAA thrombi formation in the patients without AF.
In the present case, 64-MDCT scan demonstrated the calcification of LAD (#6 and #7). At the same examination, 64-MDCT scan can demonstrate the state of the coronary artery, the pulmonary vein thrombus and no thrombi in LAA.
Presently, we know little about the pulmonary vein thrombi, and LAA thrombi of the patients without AF. When we perform 64-MDCT scan examinations to estimate the coronary artery, we should check the existence of pulmonary vein thrombi and LAA thrombi.
How to treat pulmonary vein thrombi of the patients without AF is not established, we should establish the medication to avert cerebral infarction.
Learning points.
-
▶
This is the first reported case of pulmonary vein thrombus detected by 64-MDCT in the patient without AF, which was found out when coronary artery stenosis was examined.
-
▶
When we examine the cause of cerebral infarction in the patients with AF or without AF, we may have to pay attention to the pulmonary vein thrombi, which could cause cerebral infarction.
-
▶
There is a possibility that pulmonary vein thrombi may be much more common than we recognise, because we found out the present patient among about 100 patients who were executed 64-MDCT to examine coronary artery stenosis. Much more studies are desirable.
-
▶
The cost performance of 64-MDCT is better because, when 64-MDCT examinations are performed to assess the coronary artery stenosis, calcification and plaque, we could check 3D reconstruction of the LAA and the existence of the pulmonary vein thrombi and the LAA thrombi at the same time.
-
▶
Presently, we have rivaroxaban, dabigatran and apixaban in addition to warfarin as anticoagulant treatment for the patients with AF. It remains unsolved problems whether we should use anticoagulant or not for the patients with pulmonary vein thrombi and without AF, and if we use, what medication is best among them or the others such as aspirin.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Kannel WB, Abbott RD, Savage DD, et al. Epidemiologic features of chronic atrial fibrillation: the Framingham study. N Engl J Med 1982;306:1018–22. [DOI] [PubMed] [Google Scholar]
- 2.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983–8. [DOI] [PubMed] [Google Scholar]
- 3.Hart RG, Pearce LA, Rothbart RM, et al. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. Stroke Prevention in Atrial Fibrillation Investigators. J Am Coll Cardiol 2000;35:183–7. [DOI] [PubMed] [Google Scholar]
- 4.Leung DY, Black IW, Cranney GB, et al. Prognostic implications of left atrial spontaneous echo contrast in nonvalvular atrial fibrillation. J Am Coll Cardiol 1994;24:755–62. [DOI] [PubMed] [Google Scholar]
- 5.Takeuchi H. A 64-slice multi-detector CT scan could evaluate the change of the left atrial appendage thrombi of the atrial fibrillation patient, which was reduced by warfarin therapy BMJ Case Rep 2011. 10.1136/bcr.11.2009.2491. [DOI] [PMC free article] [PubMed] [Google Scholar]