Abstract
This rare cystic lesion has an approximate incidence of 1 in 200 000. This patient complained of abdominal distension and was diagnosed with a giant mesenteric cyst measuring 26 cm in height using CT imaging. She underwent a successful ultrasound-guided drainage, which is not previously reported in the literature. This represents utilisation of an established procedure in a novel situation.
Background
This case is important as it provides multiple learning opportunities. First, abdominal distension is a common surgical differential diagnostic issue, and the cause in this case is very rare. In addition, the rarity of the condition presented a management challenge as there is scant knowledge in the literature of their aetiology and they are often misdiagnosed. Management has therefore largely consisted of surgical excision; however, this case demonstrates utilisation of an established procedure in a novel situation, as this is the first reported case of ultrasound-guided drainage being used to treat a giant mesenteric cyst.
First reported in 1907 by the Florentine anatomist Benevieni in an 8-year-old girl,1 a mesenteric cyst is a fluid-filled sac lined with endothelium or mesothelium arising anywhere in the mesentery of the duodenum through the large bowel. They may be filled with serous, chylous, sanguinous or chylolymphatic fluid and may be composed of a single sac, septated or multilocultated.2 Similar cysts also arise in the omentum of the stomach and in the retro-peritoneum and although presenting and appearing largely the same, retroperitoneal cysts may behave in a more complicated manner.3
The incidence of mesenteric cysts has been reported to be in the region of 1/100 000–1/200 000 and between 10% and 30% of these may be in children although can present at any age.3 4 Giant mesenteric cysts are even rarer and those containing chylolymphatic fluid are the rarest.2 The largest review of case reports found mesenteric cysts in the range of 2–36 cm, with 60% associated with the small bowel mesentery, 24% with large bowel and 16% in the retroperitoneum.3
Case presentation
A 38-year-old woman was referred from general practice complaining of a 1-year history of increasing abdominal distension and vague abdominal discomfort. She had no other associated symptoms and was pain free with apparently normally functioning bowels. Clinical examination revealed a large, smooth distended abdomen with no tenderness (see figures 1 and 2). Vital signs were all within normal limits.
Figure 1.
Lateral view of abdomen while supine.
Figure 2.
Lateral view of abdomen while standing.
Investigations
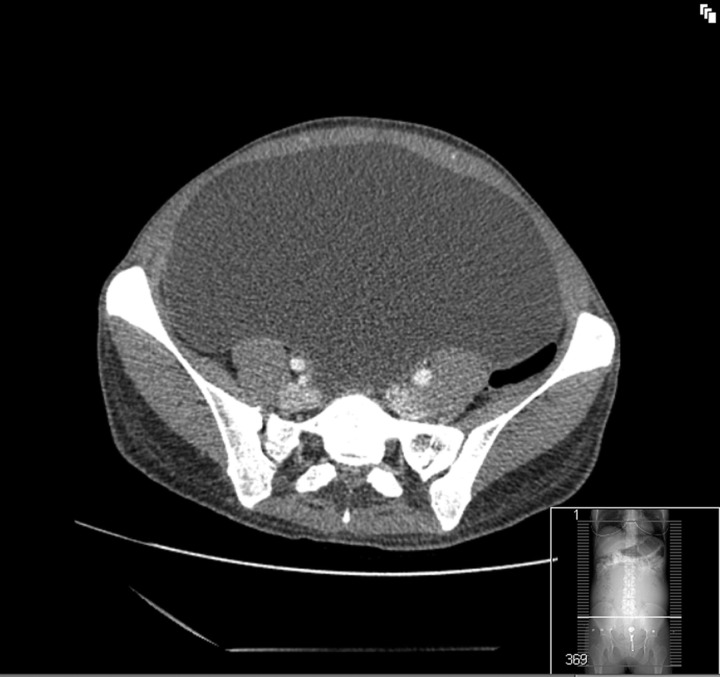
CT demonstrated a giant cyst measuring 26 cm×24 cm×12 cm extending into the pelvis. No significant lymphadenopathy was seen and the cyst did not contain any septi or significant enhancement (see figures 3 and 4).
Figure 3.
Axial CT image of mesenteric cyst.
Figure 4.
Axial CT image of mesenteric cyst.
Differential diagnosis
A surprising number of large mesenteric cysts present with no other symptoms than abdominal distension and are often misdiagnosed as ascites.5 This is probably due to the fact that mesenteric cysts do not invade tissues and are less likely to produce significant pressure on structures due to their fluid nature. However, mesenteric cysts may cause obstruction, volvulus, become infected, tort and rupture. Emergency presentations with an acute abdomen are quoted to represent around 10% of presentations.6 Owing to rarity and the non-specific presentation, 40% of simple mesenteric cysts are found incidentally at laparotomy.7
Treatment
Overall reports within the literature suggest that management of mesenteric cysts is complete surgical excision. However, laparotomy requires a long recovery period and is fraught with potential complications. With consideration to the size of the mesenteric cyst seen in our patient, an extensive incision would be required to excise the cyst completely.
With a definitive diagnosis and good-quality imaging, discussion between clinician and patient resulted in a management plan that would avoid traumatic surgery, using ultrasound imaging to guide drainage of the cyst to avoid further radiation exposure. Three litres of straw-coloured fluid was drained.
Outcome and follow-up
An uneventful recovery followed without need for inpatient admission. Cytology of the drained fluid showed scattered macrophages on a background of blood, in keeping with cyst contents, with no malignant cells seen.
Discussion
Aspiration or drainage of mesenteric cysts alone is not common and we find no other reports published in the literature. There are some reports of laparoscopic excisions of mesenteric cysts8 but mostly complete surgical excisions are reported.
The thin range of experience regarding giant mesenteric cysts means that there are no published rates of recurrence nor are there any indicators as to how rapidly this may happen. Malignancies are rarely observed in case literature. The largest retrospective cohort of 162 cases presented by Kurtz et al3 found just 5 malignancies, 2 of which were associated with retroperitoneal cysts that should be considered aside from giant mesenteric cysts because they behave differently. The only malignancy that reported, is a cystic malignant mesothelioma which may rarely be misidentified as a benign mesothelial cyst.9 In female patients an another important differential diagnosis is giant cystic ovarian neoplasms.
With today's advanced imaging techniques it is possible to identify and rule out signs of malignant processes. The risks of a large operation must be balanced against the possible complications of recurrence or malignancy following radiological drainage.
Lucey and Kuligowska10 argue the benefits of interventional radiological drainage of cysts in the abdomen and pelvis over surgery, but do, however, recommend that omental and mesenteric cysts are managed by surgical excision but fail to give reasons. They discuss the indication for alcohol sclerotherapy on cysts that recur. Other agents are used in sclerotherapy but alcohol is less toxic, easy and available and gives excellent results.10 In the event of recurrence, it may be possible that this patient simply be treated with a further drainage and sclerotherapy.
We conclude here, that there is a very deficient body of knowledge regarding giant mesenteric cysts and encourage future cases to be reported. The lack of knowledge and understanding of the condition restricts management options and we suggest that interventional radiology, meaning CT or ultrasound-guided drainage of clearly diagnosed and characterised mesenteric cysts, may save a patient from undergoing surgery. Continued investigation and experience of these rare cases should be reported to enable an effective and safe management which offers minimal invasiveness.
Learning points.
Giant mesenteric cysts are a rare cause for abdominal distension and may present painlessly with no other symptoms.
Ascites may wrongly be diagnosed clinically and detailed imaging is required for definitive diagnosis and planning of management.
Percutaneous drainage of giant mesenteric cysts is not usually performed. Imaging-guided drainage should be considered as a less invasive alternative to excision when a mesenteric cyst is clearly defined and with no worrying features.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Mohanty SK, Bal RK, Maudar KK. Mesenteric cyst—an unusual presentation. J Pediatr Surg 1998;33:792–3. [DOI] [PubMed] [Google Scholar]
- 2.Rattan K, Vimoj JN, Manish P, et al. Pediatric chylolymphatic mesenteric cyst—a separate entity from cystic lymphangioma: a case series. J Med Case Rep 2009;3:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurtz RJ, Heimann TM, Holt J, et al. Mesenteric and retroperitoneal cysts. Ann Surg 1986;203:109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bliss DP, Jr, Coffin CM, Bower RJ, et al. Mesenteric cysts in children. Surgery 1994;115:571–7. [PubMed] [Google Scholar]
- 5.Dursun H, Albayrak F, Yildirim R, et al. Giant mesenteric cyst can present as pseudoascites with raised Ca125. Gastroenterol 2009;20:305–6. [DOI] [PubMed] [Google Scholar]
- 6.Ahmadi MH, Seifmanesh H, Alimohammadi M, et al. Ileal mesenteric cyst in a patient with immediate abdominal emergency: always consider appendicitis. Am J Emerg Med 2011;29:572. [DOI] [PubMed] [Google Scholar]
- 7.Aydinli B, Yildirgan Mİ, Kantarci M, et al. Giant mesenteric cyst. Dig Dis Sci 2005;51:1380–2. [DOI] [PubMed] [Google Scholar]
- 8.Saw EC, Ramachandra S. Laparoscopic resection of a giant mesenteric cyst. Surg Laparosc Endosc 1994;4:59–61. [PubMed] [Google Scholar]
- 9.Miljković D, Gmijović D, Radojković M, et al. Mesenteric cyst. Arch Oncology 2007;15:91–3. [Google Scholar]
- 10.Lucey BC, Kuligowska E. Radiologic management of cysts in the abdomen and pelvis. Am J Roentgenol 2006;186:562–73. [DOI] [PubMed] [Google Scholar]