Abstract
Pancreaticopleural fistula is an extremely rare complication of chronic pancreatitis with characteristic feature that it may appear in the absence of changes of acute pancreatitis. We present a case of a 32-year-old man whose CT scan showed multiple pseudocysts along the body and tail of the pancreas, left crus of diaphragm and in the posterior mediastinum with associated splenoportal thrombosis. MR cholangiopancreatography imaging diagnosed the case as a pancreatico-pleural fistula, with the fistulous tract connecting distal body and tail of the pancreas to the posterior mediastinum through a diaphragmatic hiatus with right-sided mild-to-moderate pleural effusion. Meanwhile the patient was treated conservatively for his acute symptoms that included pleural tap also. Finally, endoscopic retrograde cholangiopancreatography was done and minor papilla papillotomy was performed and a stent was placed. Knowledge about such cases would help one to be aware of such a rare but dangerous complication, so that timely and correct diagnosis and management can be undertaken.
Background
This case is important because it is an unusual occurrence. Knowledge about such a rare complication could help in prompt diagnosis and accurate treatment for the betterment of the patient. This case could guide the appropriate management course also.
Case presentation
A 32-year-old man working as a plumber, coming from a low socioeconomic background presented (in February 2011) with symptoms of severe dyspnoea, chest pain, cough and dull abdominal pain. On examination, there were signs of fever (temperature of 102°F, tachycardia (100 bpm), tachypnoea (30 rpm) and hypotension (a blood pressure of 80/30 mm Hg). The patient had a history of acute pancreatitis 1 year back.
The patient was addicted to alcohol since the last 10 years and was habituated to chewing tobacco since the last 8 years.
He had no history of diabetes, hypertension, tuberculosis or trauma.
Investigations
Blood investigations revealed a normal haemogram (Hb 11.4 g/dl) except raised erythrocyte sedimentation rate (92 mm) and leucocytosis (13 800 cells/mm3).
Pleural fluid revealed high amylase (6839.5 IU/l) and lipase (38622. IU/l) levels, high white blood cell count (2800 cells/mm3) and high protein levels (5.73 g/dl).
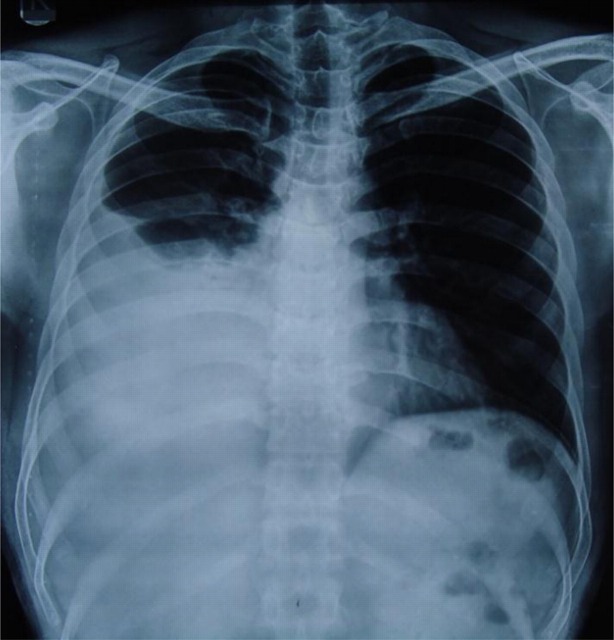
Chest x-ray—showed right-sided pleural effusion (figure 1).
Figure 1.
Right-sided pleural effusion.
On ultrasound—there were multiple pseudocysts along the body–tail of the pancreas, along with splenoportal venous thrombosis.
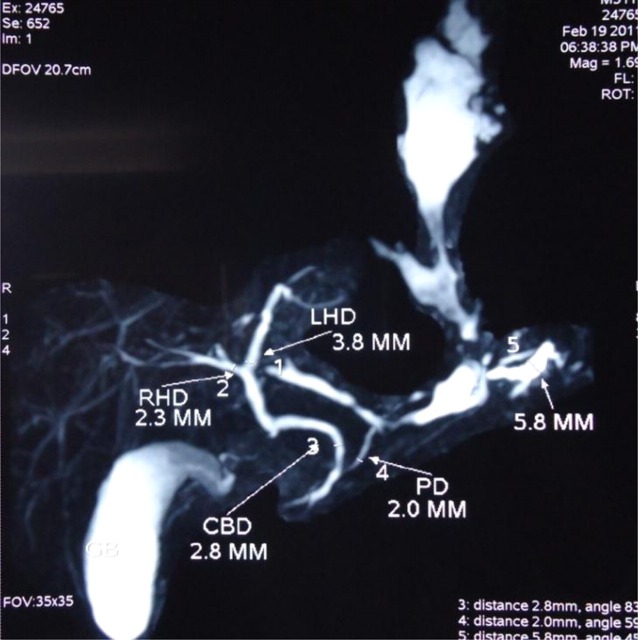
CT scan images showed multiple pseudocysts along the body and tail of the pancreas, along the left crus of the diaphragm and in the posterior mediastinum with splenoportal thrombosis (figure 2).
Figure 2.
Selected coronal CT scan image showing pseudocysts along the left crus of the diaphragm and in the posterior mediastinum.
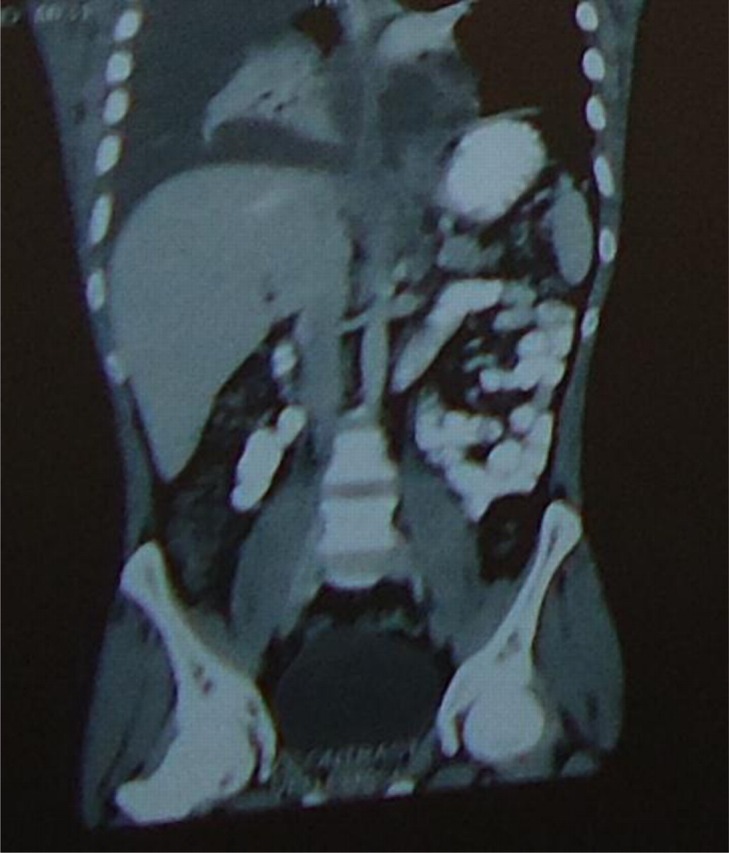
MR cholangiopancreatography (MRCP) imaging—demonstrated a fistulous tract arising from the distal body and tail of the pancreas that was extending through the diaphragmatic hiatus into the posterior mediastinum along with right-sided mild-to-moderate pleural effusion. There was another tract noted from proximal body of pancreas to porta with splenoportal thrombosis. There was no evidence of pancreatic divisum (figure 3).
Figure 3.
MR cholangiopancreatography images demonstrating a fistulous tract arising from the distal body and tail of the pancreas that was extending through the diaphragmatic hiatus into the posterior mediastinum along with right-sided mild-to-moderate pleural effusion.
Endoscopic retrograde cholangiopancreatography (ERCP) showed a normal ampulla and common bile duct. The major pancreatic duct could not be cannulated, rather the pancreaticogram was done through minor papilla. It revealed a normal pancreatic duct in the head and body region with leakage of contrast in the tail region. Fresh blood was seen coming out of the minor papilla suggesting the possibility of haemorrhage within the cyst (further steps are discussed in management) (figure 4).
Figure 4.
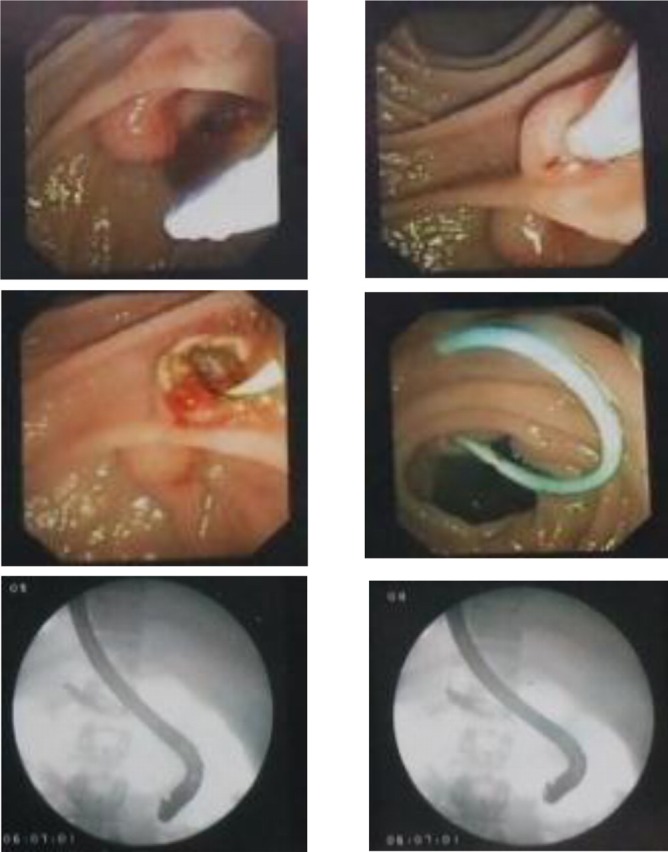
Endoscopic retrograde cholangiopancreatography image demonstrating stenting through minor papilla.
Treatment
Initially, the patient symptoms of acute attack on chronic pancreatitis were treated conservatively with antibiotics and octreotide (a somatostatin analogue). After a fistula was diagnosed, tapping of the right-sided pleural fluid was done twice.
In ERCP as difficulty was encountered in cannulating the major pancreatic duct, minor papilla papillotomy was done and a 5-Fr plastic zimmon stent was placed.
Outcome and follow-up
The poststenting phase was uneventful and the patient was well and without any complaints on discharge from the hospital after 15 days. Then the patient got a follow-up CT scan done after 1 year (March 2012) that showed no evidence of pleural effusion on either side indicating that the pancreatico-pleural fistula had resolved. However, CT scan of the abdomen showed changes of chronic pancreatitis in the form of atrophic pancreatic parenchyma with a few foci of calcification.
Thus, the fistula was cured on 1-year follow-up scan.
Discussion
Pleural effusion due to pancreatico-pleural fistula is extremely rare accounting for less than 1% of cases.1 It is seen in 3–7% of patients with pancreatitis.2 Cameron et al theorised that pleuropancreatic fistulas result when duct rupture occurs in a subacute state. If the rupture occurs anteriorly, pancreatic ascites ensues. With posterior rupture, the path of least resistance is through aortic and oesophageal hiatus in the mediastinum. A mediastinal pseudocyst results, with secretion contained by the pleura.3 Pancreaticopleural fistulae and pancreatic ascites have been termed as internal pancreatic fistulae, which share common pathogenesis.4 Middle-aged men between 40 and 50 years, who have a history of chronic alcoholism and develop pancreatitis, form the common group of patients who develop pancreatico-pleural fistula.5–8 The clinical manifestations are often misleading as symptoms are usually associated with significant pleural effusion and consist of dyspnoea, cough, chest pain fever and septicaemia.5–8 Respiratory symptoms are commoner than abdominal symptoms and usually the commonest presenting symptom is dyspnoea.2
Although CT is a non-invasive diagnostic modality, it may not demonstrate a fistula connecting the pancreas with the pleural cavity. MRCP is a recently developed technique that can demonstrate the billiary tree and pancreatic duct without contrast materials.9
But as far as management is concerned the advent of ERCP together with stenting has revolutionised the approach. ERCP shows the site of leak and reveals the ductal morphology. It also favours interventional procedures such as stent insertion vital to aid the cure of Pancreaticopleural fistula.10
Surgical treatment is safe and effective and is appropriate either when medical management fails or where underlying condition requires surgical intervention.4–11 12 The main indications for surgery are failure of conservative and endoscopic treatment, obstruction of pancreatic duct that cannot be managed endoscopically and a symptomatic fit patient.4–8 11 12 If there is an obstruction of the main pancreatic duct proximal to the fistula, surgical treatment is necessary to decompress the obstructed duct with or without excision of the involved portion of the obstructed pancreas.2–6 9 11 Cystogastrostomy, cystojejunostomy and distal and middle pancreatectomy are appropriate options in the setting of symptomatic pancreatic pseudocysts or pancreatic duct obstruction.4–8 11 12 Cystogastrostomy, cystojejunostomy and distal and middle pancreatectomy are appropriate options in the setting of symptomatic pancreatic pseudocysts or pancreatic duct obstruction.4–8 12
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Burgess NA, Moore HE, Williams JO, et al. A review of pancreatico-pleural fistula in pancreatitis and its management. HPB Surg 1991;5:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Materne R, Vranckx P, Pauls C, et al. Pancreaticopleural fistula: diagnosis with magnetic resonance pancreatography. Chest 2000;117:912–4. [DOI] [PubMed] [Google Scholar]
- 3.Carthy SM, Pellegrini CA, Moss AA, et al. Pancreaticopleural fistula: endoscopic retrograde cholangiopancreaticography & computerized tomography. AJR 1984;142:1152. [Google Scholar]
- 4.King JC, Reber HA, Shiraga S, et al. Pancreatic pleural fistula is best managed by early operative intervention. Surgery 2010;147:154–9. [DOI] [PubMed] [Google Scholar]
- 5.Sut M, Gray R, Ramachandran M, et al. Pancreaticopleural fistula: a rare complication of ERCP-induced pancreatitis. Ulster Med J 2009;78: 185–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Dhebri AR, Ferran N. Non-surgical management of pancreaticopleural fistula. JPancreas 2005;6:152–61. [PubMed] [Google Scholar]
- 7.Vyas S, Gogoi D, Sinha SK, et al. Pancreaticopleural fistula: an unusual complication of pancreatitis diagnosed with magnetic resonance cholangiopancreatography. JPancreas 2009;10:671–3. [PubMed] [Google Scholar]
- 8.Safadi BY, Marks JM. Pancreatic-pleural fistula: the role of ERCP in diagnosis and treatment. Gastrointest Endosc 2000;51:213–5. [DOI] [PubMed] [Google Scholar]
- 9.Guibaud L, Bret PM, Reinhold C, et al. Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology 1995;197:109–15. [DOI] [PubMed] [Google Scholar]
- 10.Pokharna RK, Mathur BB, Pal M, et al. Management of pancreatic-pleural fistula by endoscopic pancreatic stenting. Bikaner, Rajasthan, India: S.P. Medical College. [Google Scholar]
- 11.Uchiyama T, Suzuki T, Adachi A, et al. Pancreatic pleural effusion: case report and review of 113 cases in Japan. Am J Gastroenterol 1992;87:387–91. [PubMed] [Google Scholar]
- 12.Rockey DC, Cello JP. Pancreaticopleural fistula: report of 7 patients and review of the literature. Medicine 1990;69:332–44. [DOI] [PubMed] [Google Scholar]