Abstract
Tuberculosis in pregnancy is possibly increasing in Western Europe due to a higher incidence in immigrant women from endemic regions. Common in recent immigrants. Diagnosis during pregnancy is delayed because the disease is more frequently extra-pulmonary with few symptoms and western doctors are no longer familiar with signs and symptoms of tuberculosis. We report the case of a 28-year-old woman presenting in the 13th week of pregnancy with vaginal bleeding, respiratory symptoms including persistent coughing and fever since 1 month. Diagnosis was delayed because of doubts on taking x-rays during pregnancy, and only 6 days after admission chest x-ray and blood-cultures led to diagnose miliary tuberculosis. Despite tuberculostatic medication expulsion of an infected fetus and placenta occurred. Histological examination of the placenta confirmed tuberculosis in the placental tissue.
Background
We think this case is important both because of the uncommon clinical presentation of tuberculosis in pregnancy and the rarity of histology-proven tuberculosis disseminated to the placenta.
Also blocked tubes can be a consequence of disseminated tuberculosis.
Case presentation
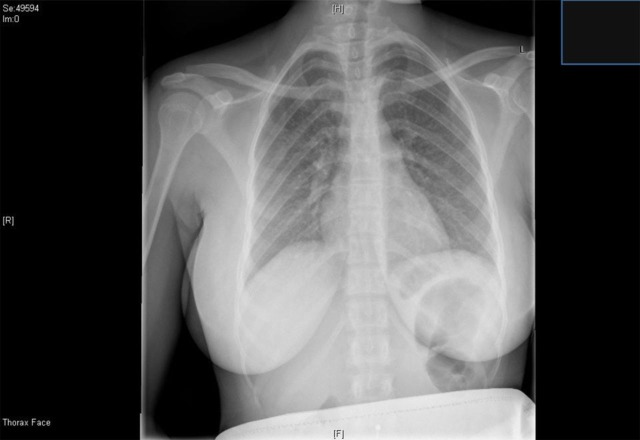
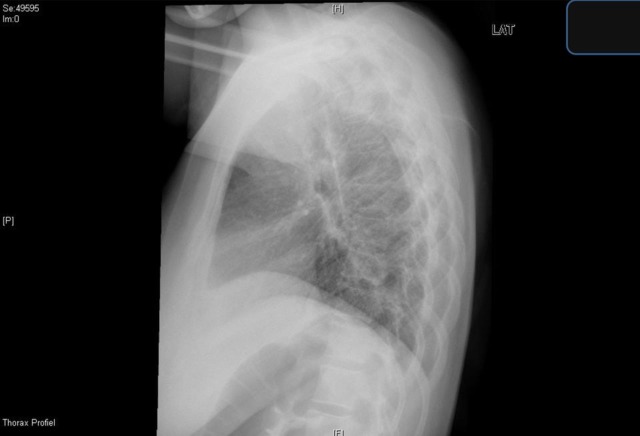
The patient is a G2P0A1, originating from Ghana and residing in Belgium since 4 years. She did not return to Africa in the last 2 years but was regularly visited by her family from Ghana. She had no history of diseases. One year before the current problem she underwent a laparoscopy for secondary infertility after a spontaneous miscarriage 2 years earlier. During laparoscopy a benign serous adenoma was removed from the left ovary and both her tubes were seen to be completely blocked. The couple was referred for in vitro fertilisation (IVF). In the course for the preparation for IVF an infection work-up was performed including testing for syphilis, HIV, chlamydia and gonorrhoea; all tests were negative; testing for tuberculosis is not part of the routine in infertility in Belgium. Pregnancy was achieved in the first cycle of IVF. At 8-weeks amenorrhoea was first seen at the prenatal obstetrics consultation, she had no complaints and a next appointment was scheduled at 11 weeks 5 days. She did not show up for this appointment, 1 week later, at 12 weeks 4 days she presented at the emergency department with persistent coughing, headache and fever for 1 month, and vaginal bleeding without cramps since 1 week. Ultrasound confirmed a viable fetus with biometry for 13 weeks. At the emergency department no chest radiography was taken as the emergency physician was convinced this should never be done in pregnant women. The patient was send home on paracetamol and came back 5 days later, still coughing, when she was seen by a senior obstetrician with experience in tropical medicine, a chest x-ray was performed demonstrating mililary tuberculosis. It was not possible to obtain sputa from the patient (figures 1–2).
Figure 1.
Posteroanterior chest radiograph.
Figure 2.
Lateral chest radiograph.
Investigations
Bronchoscopy and brocho-alveolar lavage revealed only Gram-negative bacilli.
Tuberculin test was positive.
Blood cultures were positive for Mycobacterium tuberculosis after 6 days.
Abdominal ultrasound, performed because of elevated serum liver enzymes, showed normal liver tissue and no other abdominal abnormalities.
Treatment
She was then immediately started on triple therapy including rifampicine, nicotibine and myambutol.
Outcome and follow-up
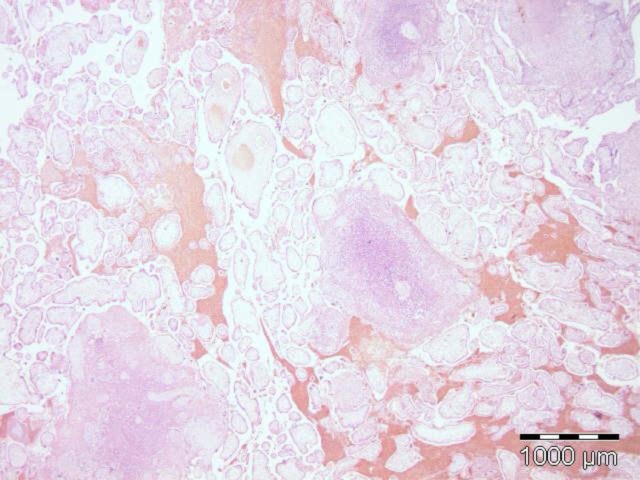
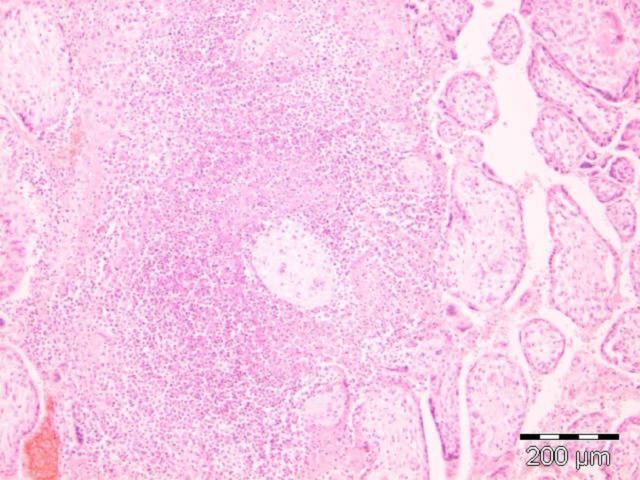
Two days after starting vaginal bleeding increased followed by cramping and resulting in the complete expulsion of fetus and placenta. (figures 3–5).
Figure 3.
Amniotic sac after expulsion with amniotic fluid and fetus inside.
Figure 4.
After opening the amniotic sac.
Figure 5.
Part of placental tissue with necrotic zone (white-yellow).
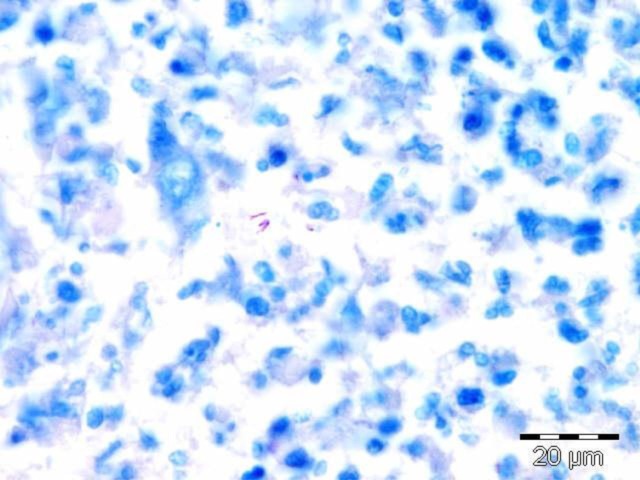
Histopathological examination of the placenta demonstrated many acid-fast bacilli in Ziehl-Neelsen staining. The fetus was not infected. (figures 6–8).
Figure 6.
H&E—placenta histopathology with necrotic zone.
Figure 7.
H&E—placenta histopathology with necrotic zone.
Figure 8.
Acid-fast bacilli in Ziehl-Neelsen staining (pink colour).
This result comfirms the diagnosis from disseminated tuberculosis in pregnant woman and placenta.
The patient continued medication and could leave the hospital after 4 days. She was further followed in the department of tropical medicine until complete cure of her tuberculosis.
Discussion
We report a rare case of disseminated tuberculosis in an otherwise healthy, pregnant woman living in Western Europe since several years and having undergone a complete work-up for IVF. Cases of disseminated tuberculosis in pregnancy in non-immune-compromised women have rarely been published and none after in vitro fertilisation for as far as we were able to find.1–10
A chest radiograph does not have to be done during routine study of infertility.
Learning points.
Clinicians should be alert for tuberculosis also in women that have lived in endemic areas in the past but have moved to the West since several years.
In the case of persistent coughing in pregnancy a chest x-ray should be performed, omitting this can lead to harmful diagnostic delay.
Tuberculosis is not confined to immune-suppressed women.
A chest radiograph should be performed in a woman submitted to routine study of infertility. Blocked tubes can be a consequence of disseminated tuberculosis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Song JY, Park CW, Kee SY, et al. Disseminated Mycobacterium avium complex infection in an immuncompetent pregnant woman. BMC infect Dis 2006;6:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liewelyn M, Cropley I, Wilkinson RJ, et al. Tuberculosis diagnosed during pregnancy: a prospective study from London. Thorax 2000;55:129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sosa LM, Cala LL, Mantilla JC. Congenital tuberculosis associated with maternal disseminated military tuberculosis. Biomedica 2007;27:475–82. [PubMed] [Google Scholar]
- 4.Gasparetto EL, Tazoniero P, de Carvalho Net A. Disseminated tuberculosis in a pregnant woman presenting with numerous brain tuberculomas. Arq Neuropsiquiatr 2003;61:855–8. [DOI] [PubMed] [Google Scholar]
- 5.Lessnau KD, Burke AC. Miliary tuberculosis. Overview Med Ref Drugs Dis Proced 2011. http://emedicine.medscape.com/article/221777-overview (accessed 15 March 2012). [Google Scholar]
- 6.Khilmani GC. Tuberculosis and pregnancy. Indian J Chest Dis Allied Sci 2000;46:105–11. [PubMed] [Google Scholar]
- 7.Hassan G, Qureshi W, Kadri SM. Congenital tuberculosis. Mini Rev JK Sci 2006;8:193–4. [Google Scholar]
- 8.Raouf S, Sharma S, Sumanda GV, et al. Disseminated extra pulmonary tuberculosis in an immune competent pregnant woman. J Obstet Gynaecol 2009;29:148–50. [DOI] [PubMed] [Google Scholar]
- 9.Gao HJ, Hu YJ, Zhu YM, et al. Retrospective analysis of cases of military tuberculosis in pregnant woman after in vitro fertilization and embryo transfer. Zhonghua Jie He He Hu Xi Za Zhi 2007;30:848–50. Abstract. Full text only Chinese. [PubMed] [Google Scholar]
- 10.Feinberg BB, Soper DE. Miliary tuberculosis: unusual cause of abdominal pain in pregnancy. South Med J 1992;85:184–6. [PubMed] [Google Scholar]