Abstract
The hepato-pulmonary syndrome (HPS) is a relatively common complication of hepatic disease that leads to hypoxaemia and dyspnoea secondary to pulmonary shunting. A number of pharmacological therapies have been trialled, yet liver transplantation remains the only definitive treatment. The use of a transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal hypertension and improve oxygenation remains controversial in HPS due to the lack of large clinical series or randomised controlled trials. We present a case of HPS successfully treated with TIPS and review the relevant literature.
Background
Hepato-pulmonary syndrome (HPS) is commonly encountered in busy, tertiary hospitals. Patients may be incapacitated with dyspnoea even when their liver disease is otherwise stable. Management options are limited. The use of a transjugular intrahepatic portosystemic shunt (TIPS) is controversial and is not recommended currently in major position papers. However, we feel that TIPS has a role in HPS and should be considered in certain cases. As more centres gain experience in this area, it may become apparent which patients will benefit from this procedure.
Case presentation
A 51-year-old man was referred to the Royal Perth Hospital's Hepatology Department after developing features of decompensated alcoholic cirrhosis with ascites, jaundice and grade 1 encephalopathy. This occurred after anterior resection and loop ileostomy for a T2N0M0 sigmoid tumour in a private hospital in January 2007. His alcohol intake was noted at between 10 and 12 standard drinks per day for most of his adult life, including beer, wine and occasional spirits. He reported abstinence since January 2007. Upon review in May 2007, a history of increasing dyspnoea over the last 2–3 months was obtained. He had biopsy-proven mild interstitial lung disease and extensive pleural thickening associated with asbestos exposure and it was felt initially that his dyspnoea, which had been mild and present for 5–10 years, was related to this problem. He had severe obstructive sleep apnoea, which was well controlled with regular nasal continuous positive airway pressure. Examination revealed mild tremor, spider naevi and gynaecomastia. He weighed 102 kg, giving a body mass index of 35.3 kg/m2. He had minimal ascites and no palpable organomegaly or peripheral oedema. A stoma bag was in place. Cardiovascular and respiratory examinations were non-contributory. Medications included frusemide 80 mg mane, spironolactone 100 mg mane, magnesium supplements, tramadol as required and a naturopathic remedy (Liver Guard). Upon review 2 weeks later, he was dyspnoeic at rest and was struggling with his activities of daily living. On examination, platypnoea was demonstrated. Orthodeoxia was demonstrated on pulse oximetry with oxygen saturations falling from 97 to 93% when moving to the upright from the supine positions. Arterial blood gases showed a pO2 of 81 mm Hg and an alveolar–arterial oxygen gradient (A–a gradient) of 28.7 mm Hg breathing room air in the supine position. The pO2 fell to 64 mm Hg in the upright position breathing room air and the A–a gradient increased to 47 mm Hg. Home oxygen was prescribed due to increasing shortness of breath, but without benefit.
Investigations
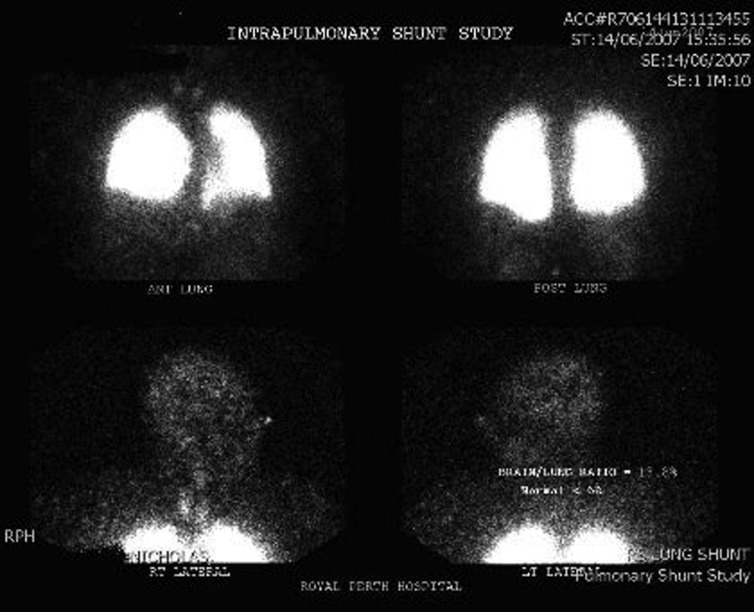
Significant investigations demonstrated a platelet count of 90 × 109/l (normal 145–400 × 109/l), international normalised ratio 1.5 (0.9–1.3), plasma sodium 125 mmol/l (134–146 mmol/l), plasma creatinine 69 μmol/l (60–110 μmol/l), total bilirubin 55 μmol/l (<20 μmol/l), alanine transaminase 30 U/l (<40 U/l), aspartate transaminase 59 U/l (<45 U/l) and albumin 35 g/l (35–50 g/l). His model for end-stage liver disease score was calculated at 13. Arterial blood gases showed a pO2 of 81 mm Hg and an A–a gradient of 28.7 mm Hg breathing room air in the supine position. The pO2 fell to 64 mm Hg in the upright position breathing room air and the A–a gradient increased to 47 mm Hg. Pulmonary function tests showed both reduced lung capacity (64% of the predicted value) and diffusion capacity for carbon monoxide (50% of the predicted value), consistent with his underlying interstitial and pleural disease. A trans-thoracic echocardiogram with injection of agitated saline demonstrated both a patent foramen ovale and features suggestive of a pulmonary shunt. Subsequently, a Technetium-99m macroaggregated albumin scan (figure 1) demonstrated abnormal uptake in the brain and kidneys with a brain/lung ratio of 13.8% (normal <6%).
Figure 1.
Technetium-99m macroaggregated albumin scan performed prior to transjugular intrahepatic portosystemic shunt, demonstrating increased uptake in the brain with an abnormal brain/lung ratio of 13.8% (normal <6%) consistent with a diagnosis of hepato-pulmonary syndrome.
Differential diagnosis
Dyspnoea from pre-existing interstitial and pleural disease was considered as a differential; however, the features of platypnoea and orthodeoxia with stable CT chest appearances, combined with typical features on the echocardiogram and Technetium-99m macro-aggregated albumin scan, led to the diagnosis of HPS as the cause of the patient's symptoms.
Treatment
Home oxygen was prescribed due to increasing shortness of breath, but without benefit. At this stage, liver transplantation was considered, but it was not felt appropriate due to the recent diagnosis of colon cancer. The HPS appeared progressive with further deterioration in his breathing and worsening hypoxia. This prompted consideration of a TIPS as a measure to reduce portal hypertension and potentially reverse the pulmonary shunting. A TIPS procedure was performed in July 2007. Hepatic venous pressure gradient (HPVG) was 12 mm Hg prior to the procedure and decreased to 9 mm Hg after placing the stent. The procedure was performed without complication and was well tolerated. No worsening encephalopathy was demonstrated in the short term. Stent patency was confirmed on ultrasound 3 days later and the patient was discharged. His liver disease remained stable without decompensation post-TIPS.
Outcome and follow-up
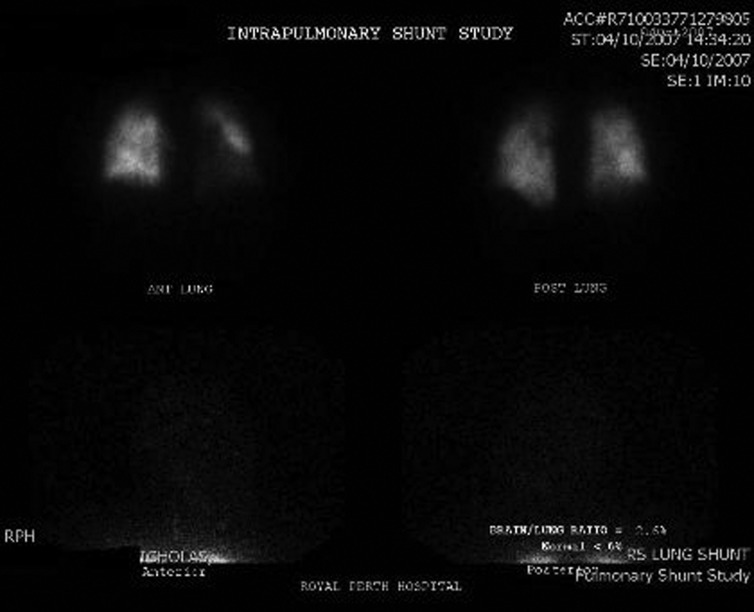
Arterial blood gases subsequent to shunt placement showed an improved pO2 of 90 mm Hg with demonstrable reduction in exertional dyspnoea and no requirement for domiciliary oxygen. Repeat Technetium-99m macro-aggregated albumin scan performed in October 2007 showed a brain/lung uptake of 2.8%, confirming reversal of the pulmonary shunting (figure 2). The patient's exercise tolerance greatly improved and he was able to walk 3–4 km per day. A flight simulation test showed resting saturation of 99% at simulated altitude with desaturation to 85% after 2 min of stepping to and from a raised surface of 20 cm. He was able to fly internationally without symptoms. Unfortunately, approximately 6 months after TIPS placement, while on an international holiday, the patient was admitted to hospital with sepsis and died a short time later.
Figure 2.
Technetium-99m macro-aggregated albumin scan performed after a transjugular intrahepatic portosystemic shunt, demonstrating normal brain uptake (brain/lung ratio 2.8%) consistent with reversal of shunting and resolution of hepato-pulmonary syndrome.
Discussion
The HPS is a complication of hepatic disease characterised by the presence of an oxygenation defect along with evidence of pulmonary vascular dilatation.1 Cirrhosis with portal hypertension is the most common hepatic disorder leading to HPS although it has been reported in acute liver conditions.2 Depending on the classification used, its reported prevalence ranges from 5 to 32%.1 Patients typically present with dyspnoea and low arterial oxygen saturation that worsens when moving from the supine to the upright positions (known as platypnea and orthodeoxia, respectively).3 Pathogenesis is unknown; however, a number of vascular mediators including nitric oxide, endothelin-1 and tumour necrosis factor-α have been implicated in the development of intra-pulmonary vascular dilatation that results in right to left shunting and hypoxaemia.4 Diagnosis is made by demonstrating hypoxaemia (pO2 <80 mm Hg or A–a gradient >15 mm Hg breathing room air) and right to left intrapulmonary shunting by trans-thoracic echocardiogram or Technetium-99m macro-aggregated albumin scanning in the setting of hepatic disease.1 The only established curative treatment for HPS is liver transplantation;3 several compounds have been trialled in the past with little success, including β-blockers, almitrine, nitric oxide inhibitors, inhaled nitric oxide, somatostatin, glucocorticoids and antibiotics.1 Garlic supplementation has recently shown encouraging results although this modality will require further investigation5 The use of TIPS for treating HPS has arisen from a theory that a reduction in portal pressure will in turn result in a reduction in levels of vascular mediators believed to be causing the pulmonary shunting. There have been several case reports on the use of TIPS in HPS with mainly encouraging results.6–14 In one report that suggested no improvement post TIPS, the HPVG was only reduced to 15 mm Hg, which suggested insufficient decompression of the portal system.12 In the only multi-case series, three patients with HPS and successful decompression of the portal system by TIPS failed to show a demonstrable improvement in gas exchange up to 4 months after the procedure.7 Those case reports that have shown positive results have been criticised for short follow-up times, although a more recent case of a 46-year-old woman with alcoholic cirrhosis reports ongoing improved oxygenation 3 years post TIPS.8 Furthermore, several reports have shown that TIPS has been used as a successful bridge to transplant, in which case a few months of improved oxygenation might be all that is required.6 10 13 Better oxygenation may also reduce the perioperative risk of liver transplantation surgery and the ICU recovery period. Despite this, TIPS is not currently recommended for use in HPS due to a lack of strong evidence and a theoretical risk of worsening the condition by enhancing the hyper-dynamic circulation.1 Our case demonstrated sustained improvement in hypoxaemia and exertional dyspnoea with successful decompression of the portal system following TIPS. There was no worsening of cardiac function from hyper-dynamic circulation, nor was there any deterioration of the underlying hepatic function. Following the TIPS procedure, there was a vast improvement in the patient's quality of life to the point where he was able to tolerate long-haul overseas flights (without the need to use oxygen) that would have otherwise been impossible. We feel that TIPS should be considered as a management option for patients with HPS, particularly as a bridge to transplantation, or in patients in which liver transplantation is contraindicated and where dyspnoea is progressive and incapacitating. Further investigation is required in order to establish the factors that predict a successful outcome for the TIPS procedure in HPS and to account for the varying results reported.
Learning points.
The hepato-pulmonary syndrome (HPS) is a relatively common complication of cirrhosis and should be considered in all patients with dyspnoea or hypoxia who are cirrhotic. Specific clinical features include orthodeoxia and platypnea; their presence should make a clinician strongly suspect HPS.
Diagnosis is made with demonstration of hypoxaemia along with left-to-right intrapulmonary shunting on transthoracic echocardiogram with injection of agitated saline or with a Technetium-99m macro-aggregated albumin scan.
The only curative treatment option is liver transplantation, but is not available or appropriate for all patients. To date, drug therapies have been disappointing.
A transjugular intrahepatic portosystemic shunt (TIPS) to reduce portal pressures has been shown to be beneficial in a selection of patients; however, it is not currently in favour in most clinical settings.
As the experience with using TIPS in treating HPS increases, so may our understanding of why it works in some patients and not in others, thereby improving the clinical utility of this potentially life-altering procedure.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Rodriguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome—a liver-induced lung vascular disorder. N Engl J Med 2008;358:2378–87. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Roisin R, Krowka MJ, Herve P, et al. Pulmonary-hepatic vascular disorders (PHD). Eur Respir J 2004;24:861–80. [DOI] [PubMed] [Google Scholar]
- 3.Ho V. Current concepts in the management of hepatopulmonary syndrome. Vasc Health Risk Manag 2008;4:1035–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spagnolo P, Zeuzem S, Richeldi L, et al. The complex interrelationships between chronic lung and liver disease: a review. J Viral Hepat 2010;17:381–90. [DOI] [PubMed] [Google Scholar]
- 5.De BK, Dutta D, Pal SK, et al. The role of garlic in hepatopulmonary syndrome: a randomized controlled trial. Can J Gastroenterol 2010;24:183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benitez C, Arrese M, Jorquera J, et al. Successful treatment of severe hepatopulmonary syndrome with a sequential use of TIPS placement and liver transplantation. Ann Hepatol 2009;8:71–4. [PubMed] [Google Scholar]
- 7.Martinez-Palli G, Drake BB, Garcia-Pagan JC, et al. Effect of transjugular intrahepatic portosystemic shunt on pulmonary gas exchange in patients with portal hypertension and hepatopulmonary syndrome. World J Gastroenterol 2005;11:6858–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chevallier P, Novelli L, Motamedi JP, et al. Hepatopulmonary syndrome successfully treated with transjugular intrahepatic portosystemic shunt: a three-year follow-up. J Vasc Interv Radiol 2004;15:647–8. [DOI] [PubMed] [Google Scholar]
- 9.Paramesh AS, Husain SZ, Shneider B, et al. Improvement of hepatopulmonary syndrome after transjugular intrahepatic portasystemic shunting: case report and review of literature. Pediatr Transplant 2003;7:157–62. [DOI] [PubMed] [Google Scholar]
- 10.Lasch HM, Fried MW, Zacks SL, et al. Use of transjugular intrahepatic portosystemic shunt as a bridge to liver transplantation in a patient with severe hepatopulmonary syndrome. Liver Transpl 2001;7:147–9. [DOI] [PubMed] [Google Scholar]
- 11.Selim KM, Akriviadis EA, Zuckerman E, et al. Transjugular intrahepatic portosystemic shunt: a successful treatment for hepatopulmonary syndrome. Am J Gastroenterol 1998;93:455–8. [DOI] [PubMed] [Google Scholar]
- 12.Corley DA, Scharschmidt B, Bass N, et al. Lack of efficacy of TIPS for hepatopulmonary syndrome. Gastroenterology 1997;113:728–30. [DOI] [PubMed] [Google Scholar]
- 13.Riegler JL, Lang KA, Johnson SP, et al. Transjugular intrahepatic portosystemic shunt improves oxygenation in hepatopulmonary syndrome. Gastroenterology 1995;109:978–83. [DOI] [PubMed] [Google Scholar]
- 14.Allgaier HP, Haag K, Ochs A, et al. Hepato-pulmonary syndrome: successful treatment by transjugular intrahepatic portosystemic stent-shunt (TIPS). J Hepatol 1995;23:102. [DOI] [PubMed] [Google Scholar]