Abstract
The subject of this case study is a 29-year-old woman who suffered a brainstem stroke. She remained severely dizzy, had a non-functional left hand secondary to weakness, severe spasticity in the right hand, a right lateral sixth nerve palsy and was unable to ambulate on presentation. The stroke occurred 2 years before presentation. The subject had been treated for 21 months at two different stroke rehabilitation centres before presentation. Our stroke protocol includes photobiomodulation administered with the XR3T-1 device and ‘muscle/bone/joint/soft tissue’ recovery techniques. The patient was seen once a week for 8 weeks and treatment sessions lasted approximately 60 min. The results were dramatic: after 8 weeks of implementation of our protocol, the patient demonstrated positive change in every area of her deficits as determined by improvements in physical examination findings. The gains achieved at 8 weeks have been maintained to this day and she continues to be treated once every 4 weeks.
Background
The American Heart Association Statistics Committee and Stroke Statistics Subcommittee data reveal that someone has a stroke in the USA every 45 s. This means that roughly 750 000 people a year suffer a stroke in the USA. Of these cases, 87% are ischaemic strokes and most people survive. The American Heart Association (AHA) states that there are about 5.4 million stroke survivors in the USA alive today. Rehabilitation is thus a major issue. We believe that this case will be very important for publication because of these numbers and because of the dramatic improvement experienced by the patient. We believe that this is a very important report and adds an interesting element to the discussion of stroke rehabilitation. Its full potential and usefulness will be determined by its reproducibility.
This case report introduces muscle/bone/joint/soft tissue recovery (MR) techniques. The techniques are most easily described as a combination of myofascial release, intense physical therapy, physiotherapy, cranio-sacral therapy and neuromuscular therapy. The MR techniques are important and a necessary part of the protocol because in stroke patients the involved muscles and joints have been immobile (and the muscles usually either spastic or flaccid) for such an extended period of time that they are extremely tight, having lost a significant range of motion and flexibility. Toxins have been allowed to build up in the soft tissue as well. Improvement in this setting will be severely limited. The MR techniques help us take these issues out of the recovery equation and set the stage for an optimal recovery.
Photobiomodulation, also known as low-level light (or laser) therapy (LLLT), is a rapidly growing therapeutic approach for diseases requiring healing, tissue regeneration and reduction of pain and inflammation. However, many clinicians are not aware of this technology and its beneficial effects. Furthermore, a proper strategy of use is critical to its successful implementation. Over a decade ago, Naeser et al published an article reporting the use of laser acupuncture in the treatment of paralysis in stroke patients.1 We believe that our report can build upon this and add a new and potent weapon to the armamentarium of clinicians who are involved in helping stroke victims recover.
Case presentation
The subject of this case study is a 29-year-old woman with no significant medical history, no family history of stroke and no social factors that predispose to stroke, who suffered a brainstem stroke in May 2008. The stroke was secondary to non-occlusive dissection of the vertebral arteries bilaterally; she suffered acute infarctions involving the medulla, superior-most aspect of the cervical spinal cord and cerebellar hemispheres bilaterally. She was treated for 3 months at an inpatient stroke rehabilitation centre and then for 18 months at an outpatient centre (where she was seen 3x/week). She was told that she had likely reached the pinnacle of her recovery.
The patient presented to our institution with the following neurological examination
Mental status: Alert, relaxed and cooperative. Mood was melancholic, anxious and fearful (mostly of falling) and emotional (easily moved to tears about issues such as being late for the appointment). No significant attention difficulties. No perceptual (environmental awareness, hallucinations, strange dreams, thought content) abnormalities. Long-term memory intact; however, there were deficits in short-term memory. For example, the patient had difficulty recalling information she had read in the morning newspaper. Thought processes coherent. Good insight into her condition. Oriented to person, place and time. Detailed cognitive testing was deferred.
Cranial nerves: I—intact; II—visual acuity intact; visual fields full; positive for double vision intermittently; III, IV, VI—right sixth nerve palsy—with the right eye fixed in the medial position; left eye without deficits; V, VII, VIII, IX, X, XII—intact; XI—weak trapezii and sternocleidomastoid muscles bilaterally (3/5 strength).
Motor: Good muscle bulk in all four extremities. Spasticity was assessed using a Modified Ashworth Scale. Right upper extremity muscle strength 1/5. Right upper extremity spasticity/rigidity as follows: shoulder mild, elbow moderate, wrist moderate to severe and the hand severe. Right shoulder, forearm, elbow, wrist and hand without voluntary movement; positive involuntary movements of the right upper extremity at the shoulder. Left upper extremity 4/5 strength (biceps, triceps and wrist); fingers of the left hand slightly flexed and hand grip strength 2/5; unable to grasp objects with the left hand. Right lower extremity 0/5 strength, good tone (not flaccid) and no spasticity/rigidity; left lower extremity 3/5 strength, good tone (not flaccid), no spasticity or rigidity. All four extremities without cyanosis or oedema. Core muscle strength severely compromised as evidenced by slumping in the wheelchair with the inability to straighten up.
Cerebellar: No ability to do rapid alternating movements, finger-to-nose, or heel-to-shin tests. Not able to stand. Not able to ambulate. Severe dizziness present when supine.
Sensory: Light touch and proprioception intact.
Treatment
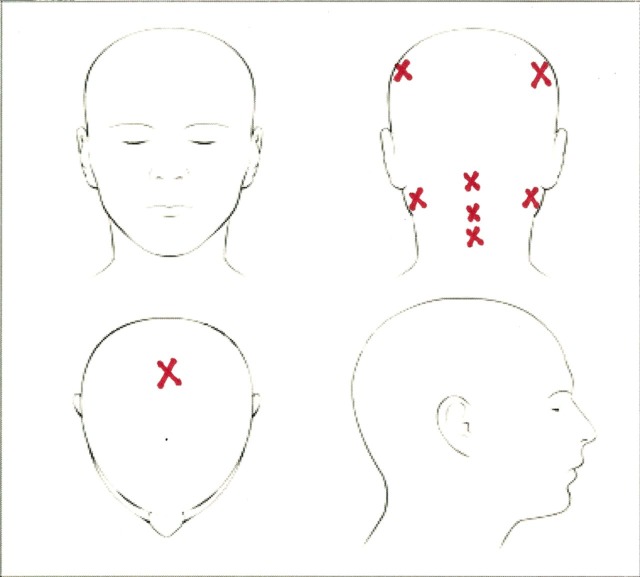
The treatment protocol requires the patient to be in the supine position. Our patient, however, became excessively dizzy when placed in this position and so this issue needed to be addressed first. The XR3T-1 device was placed on top of her head (main cranial), on each side of her head (fronto-parietal lobe), behind the ear on each side of the head (cerebellum) and in the centre of the back of her head (brainstem) for six positions in total, for 1 min per position, while the patient sat in her wheelchair. After 3 weeks she was able to lie supine on the treatment bed without dizziness. We were then able to continue with the treatment protocol.
The treatment protocol has not yet been published in the world literature so it is described here briefly. It consists of techniques termed as MR and the XR3T-1 device. MR begins with a thorough evaluation and physical examination of the area in question to assess for muscle/bone/joint/soft tissue inflammation, oedema, weakness, stiffness, nerve injury and the presence of scar tissue. This is followed by a combination of myofacial release/neuromuscular therapy/cranio-sacral therapy and intense physical therapy. The techniques were originally created by two of the authors (MC and AB) and the exact implementation is dependent on the initial evaluation and physical exam. The XR3T-1 device uses light-emitting diodes at a wavelength combination of 660 nm visible red and 850 nm near-infrared. The energy is non-ionising and the device delivers 1400 mW of power. The spot size (area) is 0.196 cm2.
The patient in this case study had a number of areas of her body affected by the stroke as detailed in the Case presentation section. The treatment protocol for her was as follows:
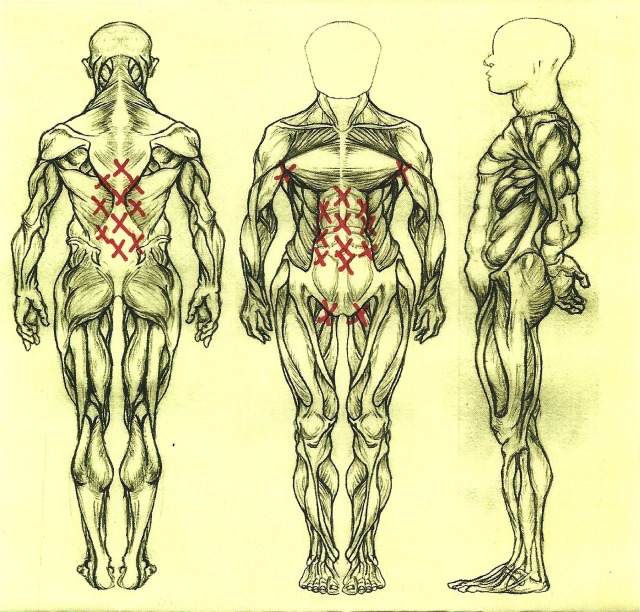
Begin each treatment section with application of the XR3T-1 device to cover a total of 32 locations, including the cerebral cortices, brainstem, cervical spine (8 locations) and the core musculature and lymphatics (24 locations). The XR3T-1 probe was placed over each site for 1 min. The total energy delivered to the patient was 2016 J and the total fluence was 2.95 J/cm2 delivered to 32 areas of the body (figure 1).
Follow up with MR to the affected areas of the body: neck, shoulders, upper extremities, hands, chest, back, flanks, core musculature, hips, lower extremities, feet and ankles (figure 2). The major muscles targeted by MR were the sternocleidomastoid, trapezius, rhomboids, latissimus dorsi, biceps, triceps, brachioradialis, teres major, teres minor, pectoralis, quadriceps, hamstrings, psoas, gluteals, piriformis, gastrocnemius, soleus, IT band and the muscles of the wrist, hands, ankles and feet.
The effect on the body was then assessed with regard to muscle spasticity, flexibility and pain. Furthermore, the patient was evaluated to assess her tolerance of the treatment session. If she felt excessively tired or fatigued, the session was stopped. If she did not feel excessively tired or fatigued, then further application of the XR3T-1 device was employed along with more MR—targeted to a particularly problematic area of the body.
Figure 1.
The red X's mark the 24 locations where the XR3T-1 device was administered. The locations include the core musculature (front and back) and the lymphatic drainage (armpits and groins bilaterally).
Figure 2.
The red X's mark the eight spots on the head and neck where the XR3T-1 device was administered. This includes the cerebral cortex, cerebellar hemispheres, brainstem and cervical spinal cord.
It is vital to note that constant evaluation and discussion with the patient was instrumental in administering the protocol. The patient's condition and response to therapy that day would dictate how quickly we could proceed. Treatment on the right eye for the sixth nerve palsy consisted of the XR3T-1 device being centred over the outside corner of the right eye. The sixth nerve palsy was resolved in three treatment sessions over a 3-week period. In summary, the treatment duration in this case report was a total of 8 weeks. The first 3 weeks of this were used to address the patient's dizziness.
Outcome and follow-up
The results were dramatic. After 8 weeks of implementation of our protocol:
Her mood became much less melancholic and she had become much less anxious and fearful. She engaged much more with us during the treatment sessions and she would often smile during the sessions. She reported to us being much more alert and aware of her environment and surroundings. She reported being able to read the newspaper again and retain information she was reading.
She was cured of her right sixth nerve palsy after three 1 min treatments.
Her double vision was eliminated.
She was cured of her dizziness and could thus lie supine on the treatment bed for her treatments.
Her right upper extremity strength improved to 2/5 and her right hand spasticity decreased; she could now move the fingers of the right hand.
Her left upper extremity strength improved to 4+/5 and she could now use her left hand to grasp objects (such as a cup, fork, etc).
Her right lower extremity strength improved to 4/5.
Her left lower extremity strength improved to 4/5.
She can stand with minimal to no assistance.
She is able to ambulate with a walker.
The gains achieved at 8 weeks have been maintained to this day (12 months) and she continues to be treated once every 4 weeks. Further progress will be detailed in a subsequent report.
Discussion
Photobiomodulation and LLLT are emerging technologies in the field of science. Their beginnings can be traced back to the discovery of laser biostimulation by Endre Mester of Semmelweis University in Budapest in 1967. Since then, there have been over 200 clinical trials and over 2000 laboratory studies reported in the world literature covering a wide range of applications. However, its use in clinical medicine is not yet widespread and many clinicians are unaware of the science and its benefits. We believe that this is due to a number of reasons: first, the biochemical mechanisms underlying the effects have only been partially elucidated and not yet completely understood; second, the complexity of choosing among a large number of illumination parameters, such as wavelength, power density, fluence, pulse structure and treatment timing, has led to the publication of negative results2; and, third, many clinicians were not taught about this technology in medical school or residency.
LLLT acts by inducing a photochemical reaction in the cell, a process known as photobiomodulation. The principle is that when light hits certain molecules called chromophores (examples of chromophores are chlorophyll in plants and haemoglobin in red blood cells), present in the protein components of the mitochondrial respiratory chain, the photon energy causes electrons to ‘jump’ from low-energy orbits to higher-energy orbits. This stored energy is used by the cell to perform various tasks (such as photosynthesis in plants).3
The mitochondria are where ATP production occurs, through the oxidative phosphorylation process and the electron transport chain. It has been shown that visible light and near-infrared light are absorbed by the mitochondria with a resultant upregulation of cellular respiration. When the energy is absorbed (the chromophore is cytochrome c oxidase, or CCO) there is photodissociation of nitric oxide (NO) from CCO which prevents the displacement of oxygen from CCO. The result is unhindered cellular respiration and an increase in ATP production. Increased ATP production will raise cellular energy levels and also result in upregulation of the cyclic AMP molecule, which is involved in many signalling pathways.3
LLLT also promotes the metabolism of oxygen, so there is an increase in reactive oxygen species (ROS). These ROS are chemically active molecules that are involved in cell signalling, regulation of the cell cycle, enzyme activation, nucleic acid synthesis and protein synthesis.4 An increase in ROS leads to the upregulation of various stimulatory and protective genes.
Other mechanisms of action of LLLT include the following:
The photodissociation of NO from CCO leads to vasodilatation as NO is a potent vasodilator through its effect on cyclic guanine monophosphate (GMP) production. Cyclic GMP is involved in other signalling pathways.
LLLT promotes the synthesis of DNA and RNA1 and increases the production of proteins.6
LLLT also modulates enzymatic activity, affects intracellular and extracellular pH and accelerates cellular metabolism.3 6
LLLT has been shown to stimulate the expression of multiple genes related to cellular proliferation, migration and the production of cytokines and growth factors.7
One can see that there are a myriad of cellular and molecular effects induced by LLLT. These photobiomodulation treatments have been reported to be effective in a variety of clinical applications, but the use of LLLT in the treatment of chronic stroke patients has never been studied. Naeser et al in 19951 used LLLT-laser acupuncture to stimulate acupuncture points on the body in chronic stroke patients with paralysis. Their findings suggested that some recovery of motor function can occur. Three patients had increases in the active range of motion for shoulder abduction, knee flexion and knee extension. One patient with hand paresis had slight increases in grip strength, lateral pinch and tip pinch. Since 1995, however, the only report of photobiomodulation and its use in stroke patients was by the (NeuroThera Effectiveness and Safety Trial) NEST-18 and NEST-29 investigators. They used a similar (although not identical) LLLT technology for the treatment of ACUTE stroke (within 24 h of the event). The authors document the safety and effectiveness of this technology and showed a trend towards statistical significance. They believe that further studies will clarify the subsets of stroke patients who will truly benefit from this treatment.
Our case report demonstrates the benefits of the treatment protocol in helping a stroke patient rehabilitate. The protocol includes two components—photobiomodulation (using the XR3T-1) and MR techniques. Both parts are integral for achieving a successful rehabilitation outcome. Photobiomodulation and LLLT have been described above. A new term (MR) was coined to describe the second component of the protocol because the techniques are novel—they were created by two of the authors (MC and AB) and have been refined over the course of 15 years. The techniques are most easily described as a combination of physical therapy, physiotherapy, cranio-sacral therapy and neuromuscular therapy. The MR techniques played an essential role in allowing the muscle groups affected by the stroke to obtain full benefit from the LLLT treatments. The techniques were instrumental in helping prevent the patient's muscles from becoming overly stiff and inflexible secondary to decreased use. If the pain and the stiffness and inflexibility had not been addressed, optimal muscular recovery and subsequent motor function recovery would not have been achieved.
Implementation of the protocol begins with a knowledgeable and thorough initial evaluation to direct treatment. This is followed by an evaluation of the patient's response (to the XR3T-1 and MR), assessment of the gap between the actual response and the desired response, and then further treatment to bridge that gap. Analogous to different physical therapists employing different strategies to achieve a desired goal, or different cardio-thoracic surgeons employing different strategies to go on bypass, arrest the heart or expose the mitral valve, an MR therapist employing our protocol will implement different strategies for the recovery of a stroke patient as dictated by the clinical situation. One can become an MR therapist and proficient in MR techniques with proper training from our institute.
The patient in this case report experienced a dramatic recovery/rehabilitation outcome after being treated with the treatment protocol. We believe that our protocol was directly responsible for the dramatic outcome because the clinical impact was seen after the treatment protocol had been used in her recovery for 2 months and after she had been treated for the previous 2 years at two different stroke recovery institutions with only minimal benefit. Nothing changed in the daily routine or in the activities of the patient other than treatment at our institute.
In summary, we believe that all of the above-listed mechanisms of action could have contributed to the improvement of our patient's motor function. Research suggests that the underlying mechanisms for the functional benefit are possible induction of neurogenesis,10 prevention of apoptosis and exertion of a neuroprotective effect11 and increased mitochondrial function.12 As Lampl states, ‘… although the mechanism of action of infrared laser therapy for stroke is not completely understood … infrared laser therapy is a physical process that can produce biochemical change at the tissue level. The putative mechanism … involves the stimulation of ATP formation by mitochondria and may also involve prevention of apoptosis in the ischaemic penumbra and enhancement of neurorecovery mechanisms’.8
The cognitive and psychological improvements brought about via the photobiomodulation treatments have been described in case reports.13 A few mechanisms are likely involved:
Increased ATP production would provide beneficial effects, including an increase in cellular respiration and oxygenation. This will help restore function in damaged cortical cells.
Oxidative stress plays a role in the damage after stroke. It is believed that photobiomodulation technology produces low levels of ROS in mitochondria of illuminated cells and that these ROS cause nuclear factor kappa B (NF-κB) activation via the redox-sensitive sensor enzyme protein kinase D1, which results in upregulation of the mitochondrial superoxide dismustase. In the short term, NF-κB is increased, but in the long term it is decreased, leading to a decrease in inflammation (less NF-κB) and an upregulation of gene products that are cytoprotective, such as superoxide dismutase, glutathione peroxidase and heat shock protein 70.13
Transcranial application of LLLT may irradiate the blood via the emissary veins located on the scalp surface, which interconnect with veins in the superior sagittal sinus. Thus, it is possible that the transcranial application of LLLT may have affected local, intracerebral blood and circulation.13 There is no study or report confirming this suggestion; further research is indicated.
There may be an increase in regional cerebral blood flow to the frontal lobes as evidenced by her improvements in memory and in her ability to read the newspaper. There may have also been increased regional cerebral blood flow to frontal pole areas, as observed in a recent study to treat major depression14; this may be responsible for the patient feeling less anxious, less melancholic, less fearful and more engaged during her sessions.
Until more basic science and clinical research is done, the exact mechanisms responsible for the observed benefits will be only partly understood. What is clear, however, is that in our patient a dramatic change did occur in both motor and cognitive areas. These changes occurred after implementation of our protocol and these dramatic changes were noted by our staff as well as by the patient and the patient's spouse.
The stroke recovery literature is adamant that rehabilitation should begin as soon as possible after the stroke and that only intense training brings about the best results. We began treatment in our patient almost 2 years after the stroke. We look forward to studying the possibilities and potential of the treatment protocol in the case when it is implemented sooner. We also look forward to implementing this strategy on future patients and reporting our results. We understand that the efficacy and applicability will depend on its reproducibility.
Learning points.
The technology of photobiomodulation can have an impact in the field of stroke rehabilitation. The wavelengths of light chosen and the other illumination parameters employed are critical elements of a successful outcome. However, muscle/bone/joint/soft tissue recovery (MR) techniques as described are also essential—the MR techniques prime the muscles and tissues to obtain full benefit from the low-level light therapy-induced photobiomodulation.
There is potential for stroke victims to benefit from photobiomodulation when it is applied with a proper protocol in the setting of stroke rehabilitation and recovery. These benefits may be seen in the realm of cognitive improvement and motor function (such as walking).
The benefits to our patient occurred almost 2 years after the stroke. There is a potential for our protocol to help even when instituted years after the insult. However, the possibility of a greater impact if instituted sooner needs to be explored.
Footnotes
Competing interests: The protocol was created by Dr. Boonswang and Ms. Chicchi.
Patient consent: Obtained.
References
- 1.Naeser MA, Alexander MP, Stiassny-Eder D, et al. Laser acupuncture in treatment of paralysis in stroke patients: CT scan lesion site study. Am J Acupuncture 1995;23:13–28. [DOI] [PubMed] [Google Scholar]
- 2.Huang YY, Chen AC, Carroll JD, et al. Biphasic dose response in low level light therapy. Dose-Response 2009;7:358–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashmi JT, Huang YY, Osmani BZ, et al. Role of low-level therapy in neurorehabilitation. PM R 2010;2(12 Suppl 2):S292–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karu TI, Kolyakov SF. Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg 2005;23:355–61. [DOI] [PubMed] [Google Scholar]
- 5.Kam T, Kalendo G, Lethokov V. Biostimulation of HeLa cells by low-intensity visible light II. Stimulation of DNA and RNA synthesis in a wide spectral range. Nuevo Cimento 1984;309.–. [Google Scholar]
- 6.Baxter GD. Therapeutic lasers: theory and practice. London, England: Churchill Livingstone, 1994:89–138. [Google Scholar]
- 7.Zhang Y, Song S, Fong C, et al. cDNA microarray analysis of gene expression profiles in human fibroblast cells irradiated with red light. J Invest Dermatol 2003;120:849–57. [DOI] [PubMed] [Google Scholar]
- 8.Lampl Y, Zivin JA, Fisher M, et al. Infrared therapy for ischemic stroke: a new treatment strategy. Stroke 2007;38:1843–9. [DOI] [PubMed] [Google Scholar]
- 9.Zivin JA, Albers GW, Bornstein N, et al. Effectiveness and safety of transcranial laser therapy for acute ischemic stroke. Stroke 2009;40:1359–64. [DOI] [PubMed] [Google Scholar]
- 10.Lampl Y. Laser treatment for stroke. Expert Rev Neurother 2007;7:961–5. [DOI] [PubMed] [Google Scholar]
- 11.Carnevalli CM, Soares CP, Zangaro RA, et al. Laser light prevents apoptosis in Cho K-1 cell line. J Clin Laser Med Surg 2003;21:193–6. [DOI] [PubMed] [Google Scholar]
- 12.Lapchak PA, De Taboada L. Transcranial near infrared laser treatment (NILT) increases cortical adenosine-5'-triphosphate (ATP) content following embolic stroke in rabbits. Brain Res 2009;1306:100–5. [DOI] [PubMed] [Google Scholar]
- 13.Naeser MA, Saltmarche A, Krengel MH, et al. Improved cognitive function after trans-cranial, light-emitting diode treatments in chronic, traumatic brain injury: two case reports. Photomed Laser Surg 2011;29:351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schiffer F, Johnston AL, Ravichandran C, et al. Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety. Behav Brain Func 2009;5 http://www.behavioralandbrainfunctions.com/content/5/1/46. [DOI] [PMC free article] [PubMed] [Google Scholar]