Abstract
Purpose
Wheezing following viral lower respiratory tract infections (LRTIs) in children <2 years of age is an important risk factor for the development of asthma later in life; however, not all children with viral LRTIs develop wheezing. This study investigated risk factors for the development of wheezing during viral LRTIs requiring hospitalization.
Methods
The study included 142 children <2 years of age hospitalized for LRTIs with at least one virus identified as the cause and classified them into children diagnosed with LRTIs with wheezing (n=70) and those diagnosed with LRTIs without wheezing (n=72).
Results
There were no significant differences in the viruses detected between the two groups. Multivariate logistic regression analysis showed that, after adjusting for potentially confounding variables including sex and age, the development of wheezing was strongly associated with parental history of allergic diseases (adjusted odds ratio [aOR], 20.19; 95% confidence interval [CI], 3.22-126.48), past history of allergic diseases (aOR, 13.95; 95% CI, 1.34-145.06), past history of hospitalization for respiratory illnesses (aOR, 21.36; 95% CI, 3.77-120.88), exposure to secondhand smoke at home (aOR, 14.45; 95% CI, 4.74-44.07), and total eosinophil count (aOR, 1.01; 95% CI, 1.01-1.02).
Conclusion
Past and parental history of allergic diseases, past history of hospitalization for respiratory illnesses, exposure to secondhand smoke at home, and total eosinophil count were closely associated with the development of wheezing in children <2 years of age who required hospitalization for viral LRTIs. Clinicians should take these factors into consideration when treating, counseling, and monitoring young children admitted for viral LRTIs.
Keywords: Respiratory tract infections, Risk factors, Viruses, Wheezing
Introduction
Lower respiratory tract infections (LRTIs) are common in early childhood and are mostly caused by respiratory viruses. Wheezing caused by viruses is considered an important risk factor for the development of asthma later in life1,2,3,4,5).
Although the same virus may cause LRTIs, only those who develop wheezing during LRTIs are more likely to develop asthma1,5). Thus, upon infection with a virus, children less than 2 years of age with and without wheezing may differ with regard to the development of recurrent wheezing and/or asthma. Children diagnosed with LRTIs with wheezing would be more likely to develop recurrent wheezing and/or asthma in late childhood than those with LRTIs without wheezing, even though they are infected with the same virus. In this regard, previous studies have reported risk factors for young children who are more likely to have wheezing during or following a viral LRTI6,7). However, there are relatively small data focusing on the clinical risk factors related to the development of wheezing in young children with LRTIs who require hospitalization.
This study was designed to determine clinical risk factors associated with the development of wheezing in infants and young children less than 2 years of age who require hospitalization for viral LRTIs.
Materials and methods
1. Study subjects
We conducted a cross-sectional study of all infants and children admitted to the CHA Bundang Medical Center from August 2006 through July 2007 with signs and symptoms of LRTIs. Inclusion criteria were as follows: (1) children less than 2 years of age; and (2) children with a positive nasopharyngeal washing aspirate confirming infection with at least one of the 12 respiratory viruses. A total of 400 children were admitted with LRTIs during the study period. All had signs and symptoms of LRTIs: i.e., cough, tachypnea, respiratory distress, and breathing difficulties with grunting or wheezing sounds with rales8). After a complete physical examination by an experienced pediatrician, children who developed wheezing on auscultation at admission and/or during hospitalization were defined as the LRTIs with wheezing and those who did not develop wheezing were defined as the LRTIs without wheezing.
Infants and young children were excluded if (1) they were infected with Mycoplasma pneumoniae, defined as an initial indirect microparticle agglutinin method (Serodia-Myco II, Fujirebio, Japan) (titer of >1:320) or a fourfold rising titer in double-checking samples and positivity for anti-Mycoplasma IgM9), (2) no virus was detected, (3) their parents or guardians did not respond to questionnaires regarding the patient's past and parental history at admission, (4) they were born prematurely (i.e., less than 37 weeks gestational age), or (5) they had a cardiac anomaly. Clinical factors recorded at admission included sex; age; the presence of fever; laboratory findings; patient's and parental history of allergic diseases, including asthma10), allergic rhinitis-like symptoms11), and atopic dermatitis12); previous hospitalization for respiratory illnesses; and smoking by any member of the household during the previous year, with the latter defined as exposure of the patient to secondhand smoke. At admission, blood samples were obtained from the antecubital vein of each subject and laboratory tests, including complete blood count, absolute neutrophil count, total eosinophil count, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR), were performed and recorded for each subject. The study protocol was reviewed and approved by the Institutional Review Board of CHA University Medical Center, Seongnam, Korea, and written informed consent was obtained from the parents/guardians of each patient.
2. Nasopharyngeal aspirates collection and multiplex reverse transcription-polymerase chain reaction
Nasopharyngeal aspirates were obtained upon admission by gently flushing the children's nostrils with 4 mL of sterile saline solution. All nasopharyngeal aspirates were tested within 24 hours of collection for respiratory syncytial viruses (A and B), human metapneumovirus, human rhinovirus, influenza A and B viruses, parainfluenza (A, B, and C) virus, coronavirus (A and B), and adenovirus. Total viral RNA was extracted from nasopharyngeal aspirates (300 µL) using Viral Gene-spin Viral DNA/RNA Extraction Kits (iNtRON, Seongnam, Korea) and stored at -80℃. First-strand cDNA was synthesized using Revert Aid First Strand cDNA Synthesis Kits (Fermentas Inc., Burlington, ON, Canada), followed by polymerase chain reactions using Seeplex Respiratory Viruses Detection Kits-1 (Seegene, Seoul, South Korea) and the GeneAmp PCR system 9700 (Applied Biosystems, Waltham, MA, USA). Each 20 µL reaction mixture included 3 µL of cDNA, 4 µL of 5× RV1A or 5× RV1B primer, and 10 µL of 2× Multiplex Master Mix. Briefly, 2.5 µL of extracted RNA was mixed with 5× buffer, 0.2mM of each dNTP, 0.5µM of each primer13,14,15,16), 1 µL of enzyme mix, and DEPC-treated ultrapure water to a final volume of 25 µL. After incubations at 50℃ for 30 minutes and at 94℃ for 15 minutes, the reactions were subjected to 40 cycles of denaturation for 30 seconds at 94℃, annealing for 90 seconds at 60℃, and extension for 90 seconds at 72℃, followed by a final extension at 72℃ for 10 minutes. The amplified products were analyzed on 2% agarose gels containing 0.5 g/mL ethidium bromide.
3. Statistical analysis
Data are expressed as mean±standard deviation unless otherwise indicated. Between-group differences were compared using independent Student t tests, Mann-Whitney U tests, or chi-square tests, as appropriate. Multivariate logistic regression analysis was used to identify clinical risk factors for the development of wheezing caused by viruses, with adjusted odds ratios (aORs) and 95% confidence intervals (CIs) calculated; age and total eosinophil count were used as continuous variables and the other factors were used as categorical variables. All statistical analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). All statistical tests were two-sided, with a P value of <0.05 indicating statistical significance.
Results
1. Clinical characteristics of subjects
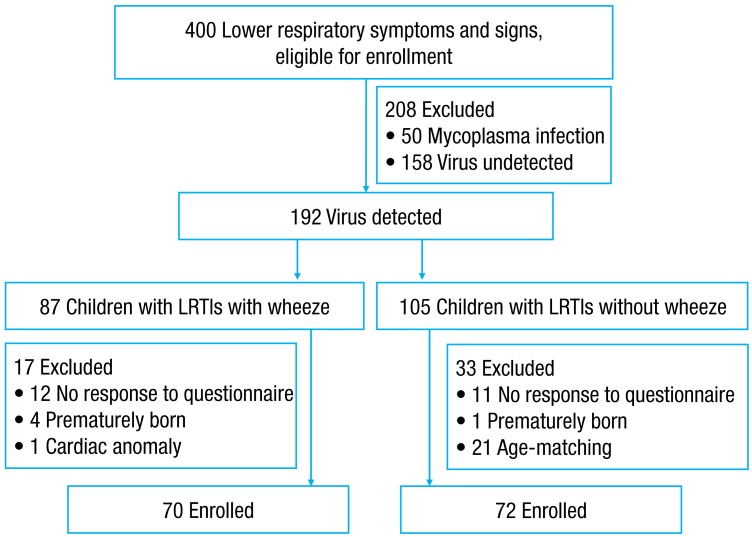
The demographic and clinical characteristics of the study population are shown in Table 1. The study population consisted of 142 children aged <2 years, 70 children with LRTIs with wheezing and 72 children with LRTIs without wheezing (Fig. 1). The mean ages of the children with the LRTIs with and without wheezing were 7.0±5.4 and 8.3±5.9 months, respectively. Approximately 70% of the children in each group were male. There were no between-group differences in sex, age, absolute neutrophil count, CRP concentration, and ESR. The percentage of subjects with temperature >38℃ during hospitalization (42.9% [30/70] vs. 73.6% [53/72], P<0.001) and the white blood cell (WBC) count (10,044.1±3,391.7 cells/mm3 vs. 11,609.2±4,343.4 cells/mm3, P=0.018) were significantly lower in children with the LRTIs with wheezing than in those with the LRTIs without wheezing. The total eosinophil count was significantly higher in children with the LRTIs with wheezing than in those with the LRTIs without wheezing (155.8±219.3 cells/mm3 vs. 90.7±125.9 cells/mm3, P=0.031) (Table 1).
Table 1. Demographic and clinical characteristics of children diagnosed with lower respiratory tract infections with and without wheezing.
| Variable | Children diagnosed with LRTIs with wheezing (n=70) | Children diagnosed with LRTIs without wheezing (n=72) | P value |
|---|---|---|---|
| Male sex | 50 (71.4) | 50 (69.4) | 0.855 |
| Age (mo) | 7.0±5.4 | 8.3±5.9 | 0.150 |
| Temperature >38℃ | 30 (42.9) | 53 (73.6) | <0.001 |
| White blood cell ( /mm3) | 10,044.1±3,391.7 | 11,609.2±4,343.4 | 0.018 |
| Absolute neutrophil count (cells/mm3) | 3,483.5±2,942.5 | 4,437.9±2,848.8 | 0.052 |
| Total eosinophil count (cells/mm3) | 155.8±219.3 | 90.7±125.9 | 0.031 |
| C-reactive protein (mg/dL) | 1.1±1.7 | 1.8±3.1 | 0.068 |
| Erythrocyte sedimentation rate (mm/hr) | 17.6±12.7 | 22.5±19.3 | 0.073 |
| Parental history of allergic diseases | 15 (21.4) | 2 (2.8) | 0.001 |
| Past history of allergic diseases | 12 (17.1) | 1 (1.4) | 0.001 |
| Past history of hospitalization for respiratory illnesses | 15 (21.4) | 2 (2.8) | <0.001 |
| Secondhand smoke at home | 37 (52.9) | 7 (9.7) | <0.001 |
Values are presented as number (%) or mean±standard deviation.
P values were determined using the chi-square tests, independent Student t tests, or Mann-Whitney U tests, as appropriate.
LRTIs, lower respiratory tract infections.
Fig. 1. Flow chart of study subject enrollment. Four hundred patients admitted for typical signs and symptoms of lower respiratory tract infections (LRTIs) were eligible for enrollment. Nasopharyngeal swabs from 192 of these patients (48%) showed positive results upon virus polymerase chain reaction testing. After excluding subjects in line with the exclusion criteria (no response to questionnaire, prematurity, age-matching, and cardiac anomaly), a total of 142 subjects were included in the final analysis. These subjects consisted of 70 children diagnosed with LRTIs with wheezing and 72 children diagnosed with LRTIs without wheezing.
2. Clinical variables in the children diagnosed with LRTIs with and without wheezing
The children with the LRTIs with wheezing were more likely to have parents with a history of allergic diseases than the children with the LRTIs without wheezing (21.4% [15/70] vs. 2.8% [2/72], P=0.001) (Table 1). Moreover, the rates of doctor-diagnosed asthma (7.1% [5/70] vs. 0% [0/72], P=0.019) and doctor-diagnosed atopic dermatitis (8.6% [6/70] vs. 1.4% [1/72], P=0.046), but not allergic rhinitis-like symptoms (2.0% [2/70] vs. 0% [0/72], P=0.146), were significantly higher in children with wheezing than those without wheezing. When asthma, allergic rhinitis-like symptoms, and atopic dermatitis were analyzed together as past history of allergic diseases, those with wheezing were significantly more likely to have past history of allergic diseases than those diagnosed with the LRTIs without wheezing (17.1% [12/70] vs. 1.4% [1/72], P=0.001). Moreover, past history of hospitalization for respiratory illnesses (21.4% [15/70] vs. 2.9% [2/72], P<0.001), and exposure to secondhand smoke (52.9% [37/70] vs. 9.7% [7/72], P<0.001) were significantly more common in children with the LRTIs with wheezing than in those with the LRTIs without wheezing.
3. Comparison of viruses in the children diagnosed with LRTIs with and without wheezing
Table 2 shows the comparison of viruses identified in the study subjects diagnosed with LRTIs with and without wheezing. Respiratory syncytial virus was detected in 39 subjects (55.7%) in the children diagnosed with LRTIs with wheezing and 37 (51.4%) in those diagnosed with LRTIs without wheezing; human metapneumovirus in 14 (20.0%) and 9 (12.5%), respectively; and human rhinovirus in 12 (17.1%) and 11 (15.3%), respectively. There were no between-group differences in the incidence of each virus (P>0.05 each).
Table 2. Comparison of viruses identified in children less than 2 years of age hospitalized with lower respiratory tract infections with and without wheezing.
| Variable | Children diagnosed with LRTIs with wheezing (n=70) | Children diagnosed with LRTIs without wheezing (n=72) | P value |
|---|---|---|---|
| RSV | 39 (55.7) | 37 (51.4) | 0.618 |
| Human metapneumovirus | 14 (20.0) | 9 (12.5) | 0.260 |
| Human rhinovirus | 12 (17.1) | 11 (15.3) | 0.822 |
| Influenza virus | 4 (5.7) | 9 (12.5) | 0.244 |
| Parainfluenza virus | 8 (11.4) | 4 (5.6) | 0.241 |
| Coronavirus | 2 (2.9) | 3 (4.2) | 1.000 |
| Adenovirus | 1 (1.4) | 3 (4.2) | 0.620 |
| Coinfections | 9 (12.9) | 4 (5.6) | 0.155 |
Values are presented as number (%).
P values were determined using the chi-square test.
LRTIs, lower respiratory tract infections; RSV, respiratory syncytial virus.
4. Association between development of wheezing and clinical variables
We utilized multivariate analysis to determine the relationships between the development of wheezing and clinical variables in the study subjects. Multivariate logistic regression analysis showed that after adjusting for potential confounding variables including sex and age, the development of wheezing was strongly associated with parental history of allergic diseases (aOR, 20.19; 95% CI, 3.22-126.48), past history of allergic diseases (aOR, 13.95; 95% CI, 1.34-145.06), past history of hospitalization for respiratory illnesses (aOR, 21.36; 95% CI, 3.77-120.88), exposure to secondhand smoke at home (aOR, 14.45; 95% CI, 4.74-44.07), and total eosinophil count (aOR, 1.01; 95% CI, 1.01-1.02) (Table 3).
Table 3. Results of multivariate logistic regression analysis to assess independent relationships between the development of wheezing and clinical risk factors in children hospitalized for viral lower respiratory tract infections.
| Variable | Multivariate model | |
|---|---|---|
| aORs (95% CIs) | P value | |
| Male sex | 1.44 (0.49-4.25) | 0.506 |
| Age | 1.12 (0.96-1.31) | 0.154 |
| Parental history of allergic diseases | 20.19 (3.22-126.48) | 0.001 |
| Past history of allergic diseases | 13.95 (1.34-145.06) | 0.027 |
| Past history of hospitalization due to respiratory illnesses | 21.36 (3.77-120.88) | 0.001 |
| Secondhand smoke at home | 14.45 (4.74-44.07) | <0.001 |
| Total eosinophil count | 1.01 (1.01-1.02) | 0.003 |
aORs, adjusted odds ratios; CI, confidence interval.
Discussion
The present study showed that past and parental history of allergic diseases, past history of hospitalization for respiratory illnesses, exposure to secondhand smoke at home, and serum total eosinophil count were independently associated with the development of wheezing in children <2 years of age who had viral lower respiratory infections requiring hospitalization.
Our findings are in good agreement with those of previous studies, which reported that the development of childhood wheezing is closely associated with parental history of allergic disease17) and a personal history of allergic diseases18). A recent study from the PARIS (Pollution and Asthma Risk: an Infant Study) birth cohort focusing on the determinants of wheezing severity in infants found that the risk of severe wheezing was mainly ascribed to the atopic status of the child17). This study corresponds well with our findings that the children included in the present study had signs and symptoms severe enough to require hospitalization and that the children diagnosed with LRTIs with wheezing had a higher incidence of parental and past history of allergic diseases than those with LRTIs without wheezing.
Viral lower respiratory infection is a major risk factor for development of wheezing. These illnesses are thought to interact with allergic inflammation, altering airways by damaging lower epithelial cells, increasing the release of mast cell mediators, and amplifying allergic inflammation19). Several viruses, including respiratory syncytial virus20,21,22), human rhinovirus20,23,24), and human metapneumovirus20,25), have been associated with the development of wheezing in children. In contrast, we observed no differences in the incidence of each virus in the children diagnosed with and without wheezing, suggesting that, at least in this cohort of children, the development of wheezing was not associated with specific viral agents causing LRTIs requiring hospitalization.
Previous studies have suggested the hypothesis that susceptibility to viral bronchiolitis may be an early manifestation of biased immune responses, which associates with both diminished viral defense and atopic airway inflammation26). Furthermore, viral infection in infancy may alter subsequent Th1/Th2 immune responses and enhance Th2 sensitization to inhalant allergens, resulting in the development of an asthmatic phenotype27,28). Although we did not look into the long-term outcome of the children with LRTIs with wheezing, we speculate that the development of wheezing in these young children may be an early manifestation of Th2-biased immune response to viral respiratory infections. Therefore, the interaction between age at initial infection, genetic susceptibility, and virus will determine the outcome of respiratory virus infection and airway disorders.
One clinically important finding in the present study is that the children diagnosed with LRTIs with wheezing showed a lower incidence of temperature >38℃, a lower WBC count, and a higher total eosinophil count when compared with those with LRTIs without wheezing. This may be due to the notion that upon viral LRTI, the children with wheezing may demonstrate Th2-type response, whereas those without wheezing demonstrate Th1-type response; this is also supported by the higher incidence of past and parental history of allergic diseases in children with wheezing. It is well-known that blood eosinophil count reflects systemic eosinophilic inflammation and associates with having wheeze. A recent cross-sectional study examining the value of blood eosinophil count in a random population sample of 12,408 subjects found that a higher blood eosinophil count was closely associated with having asthma, wheeze, and asthma attacks29), a finding that corresponds well with our results.
The harmful effects of exposure to secondhand smoke on the development of wheezing in infants and toddlers are well established17,30,31,32,33). In line with previous studies, we found that exposure to secondhand smoke was a risk factor for development of wheezing in children with viral LRTIs requiring hospitalization. The severity of bronchiolitis in early life has been shown to be altered by postnatal exposure to maternal tobacco smoke, and by atopy and age of the infant34). Thus, children exposed to secondhand smoke are at risk of airway infiltration by small particles, making these children more susceptible to develop wheezing when infected with a respiratory virus. We speculate that contrary to the other clinical risk factors, exposure to secondhand smoke at home is a modifiable environmental risk factor for young children in terms of preventing the development of wheezing when inflicted with viral LRTIs.
The present study had some limitations. First, it was of cross-sectional design; therefore, we were unable to determine predictive factors for recurrent wheezing in late childhood. Second, we did not classify familial smoking into smoking during pregnancy and/or after delivery or into paternal and/or maternal smoking. Third, the infants were not subjected to pulmonary function tests; therefore, wheezing and lung function were not measured in an objective manner. Fourth, the present study yielded high odds ratios for clinical factors such as past and parental history of allergic diseases with regard to the development of wheeze in the study subjects. This may be ascribed to the fact that they are the most likely sensitizers to wheezing in children hospitalized for LRTIs. Finally, we did not determine allergic sensitization of the study subjects, which is considered to play a role in the development of wheezing35).
In conclusion, we found that past and parental history of allergic diseases, past history of hospitalization for respiratory illnesses, exposure to secondhand smoke at home, and total eosinophil count were closely associated with the development of wheezing in children less than 2 years of age who required hospitalization for viral LRTIs. Clinicians should take these clinical factors into consideration in treating, counseling, and monitoring young children hospitalized for viral LRTIs.
Footnotes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Kusel MM, de Klerk NH, Kebadze T, Vohma V, Holt PG, Johnston SL, et al. Early-life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol. 2007;119:1105–1110. doi: 10.1016/j.jaci.2006.12.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med. 2000;161:1501–1507. doi: 10.1164/ajrccm.161.5.9906076. [DOI] [PubMed] [Google Scholar]
- 3.Sigurs N, Gustafsson PM, Bjarnason R, Lundberg F, Schmidt S, Sigurbergsson F, et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med. 2005;171:137–141. doi: 10.1164/rccm.200406-730OC. [DOI] [PubMed] [Google Scholar]
- 4.Lemanske RF, Jr, Jackson DJ, Gangnon RE, Evans MD, Li Z, Shult PA, et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol. 2005;116:571–577. doi: 10.1016/j.jaci.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 5.Jackson DJ, Gangnon RE, Evans MD, Roberg KA, Anderson EL, Pappas TE, et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Callaghan-Gordo C, Bassat Q, Diez-Padrisa N, Morais L, Machevo S, Nhampossa T, et al. Lower respiratory tract infections associated with rhinovirus during infancy and increased risk of wheezing during childhood. A cohort study. PLoS One. 2013;8:e69370. doi: 10.1371/journal.pone.0069370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kennedy JL, Shaker M, McMeen V, Gern J, Carper H, Murphy D, et al. Comparison of viral load in individuals with and without asthma during infections with rhinovirus. Am J Respir Crit Care Med. 2014;189:532–539. doi: 10.1164/rccm.201310-1767OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito S, Daleno C, Baggi E, Ciarmoli E, Lavizzari A, Pierro M, et al. Circulation of different rhinovirus groups among children with lower respiratory tract infection in Kiremba, Burundi. Eur J Clin Microbiol Infect Dis. 2012;31:3251–3256. doi: 10.1007/s10096-012-1692-9. [DOI] [PubMed] [Google Scholar]
- 9.Chung HL, Kim SG, Shin IH. The relationship between serum endothelin (ET)-1 and wheezing status in the children with Mycoplasma pneumoniae pneumonia. Pediatr Allergy Immunol. 2006;17:285–290. doi: 10.1111/j.1399-3038.2006.00393.x. [DOI] [PubMed] [Google Scholar]
- 10.The Global Initiative for Asthma. GINA Report, Global strategy for asthma management and prevention [Internet] The Global Initiative for Asthma; c2011. [Updated December, 2011]. [cited 2014 Sep 8]. Available from: http://www.ginasthma.org/guidelines-gina-report-global-strategy-for-asthma.html. [Google Scholar]
- 11.Herr M, Clarisse B, Nikasinovic L, Foucault C, Le Marec AM, Giordanella JP, et al. Does allergic rhinitis exist in infancy? Findings from the PARIS birth cohort. Allergy. 2011;66:214–221. doi: 10.1111/j.1398-9995.2010.02467.x. [DOI] [PubMed] [Google Scholar]
- 12.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1980;92:44–47. [Google Scholar]
- 13.Bellau-Pujol S, Vabret A, Legrand L, Dina J, Gouarin S, Petitjean-Lecherbonnier J, et al. Development of three multiplex RT-PCR assays for the detection of 12 respiratory RNA viruses. J Virol Methods. 2005;126:53–63. doi: 10.1016/j.jviromet.2005.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vabret A, Mouthon F, Mourez T, Gouarin S, Petitjean J, Freymuth F. Direct diagnosis of human respiratory coronaviruses 229E and OC43 by the polymerase chain reaction. J Virol Methods. 2001;97:59–66. doi: 10.1016/S0166-0934(01)00343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vabret A, Mourez T, Dina J, van der Hoek L, Gouarin S, Petitjean J, et al. Human coronavirus NL63, France. Emerg Infect Dis. 2005;11:1225–1229. doi: 10.3201/eid1108.050110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vabret A, Dina J, Gouarin S, Petitjean J, Corbet S, Freymuth F. Detection of the new human coronavirus HKU1: a report of 6 cases. Clin Infect Dis. 2006;42:634–639. doi: 10.1086/500136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herr M, Just J, Nikasinovic L, Foucault C, Le Marec AM, Giordanella JP, et al. Influence of host and environmental factors on wheezing severity in infants: findings from the PARIS birth cohort. Clin Exp Allergy. 2012;42:275–283. doi: 10.1111/j.1365-2222.2011.03933.x. [DOI] [PubMed] [Google Scholar]
- 18.Kurosaka F, Terada T, Tanaka A, Nakatani Y, Yamada K, Nishikawa J, et al. Risk factors for wheezing, eczema and rhinoconjunctivitis in the previous 12 months among six-year-old children in Himeji City, Japan: food allergy, older siblings, day-care attendance and parental allergy history. Allergol Int. 2011;60:317–330. doi: 10.2332/allergolint.10-OA-0246. [DOI] [PubMed] [Google Scholar]
- 19.Brunetti L, Colazzo D, Francavilla R, Tesse R, De Sario V, Lore M, et al. The role of pulmonary infection in pediatric asthma. Allergy Asthma Proc. 2007;28:190–193. doi: 10.2500/aap.2007.28.2964. [DOI] [PubMed] [Google Scholar]
- 20.Fujitsuka A, Tsukagoshi H, Arakawa M, Goto-Sugai K, Ryo A, Okayama Y, et al. A molecular epidemiological study of respiratory viruses detected in Japanese children with acute wheezing illness. BMC Infect Dis. 2011;11:168. doi: 10.1186/1471-2334-11-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bacharier LB, Cohen R, Schweiger T, Yin-Declue H, Christie C, Zheng J, et al. Determinants of asthma after severe respiratory syncytial virus bronchiolitis. J Allergy Clin Immunol. 2012;130:91–100.e3. doi: 10.1016/j.jaci.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Regnier SA, Huels J. Association between respiratory syncytial virus hospitalizations in infants and respiratory sequelae: systematic review and meta-analysis. Pediatr Infect Dis J. 2013;32:820–826. doi: 10.1097/INF.0b013e31829061e8. [DOI] [PubMed] [Google Scholar]
- 23.Piotrowska Z, Vazquez M, Shapiro ED, Weibel C, Ferguson D, Landry ML, et al. Rhinoviruses are a major cause of wheezing and hospitalization in children less than 2 years of age. Pediatr Infect Dis J. 2009;28:25–29. doi: 10.1097/INF.0b013e3181861da0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kieninger E, Fuchs O, Latzin P, Frey U, Regamey N. Rhinovirus infections in infancy and early childhood. Eur Respir J. 2013;41:443–452. doi: 10.1183/09031936.00203511. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-García ML, Calvo C, Falcon A, Pozo F, Perez-Brena P, De Cea JM, et al. Role of emerging respiratory viruses in children with severe acute wheezing. Pediatr Pulmonol. 2010;45:585–591. doi: 10.1002/ppul.21225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saglani S. Viral infections and the development of asthma in children. Ther Adv Infect Dis. 2013;1:139–150. doi: 10.1177/2049936113497202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Macaubas C, de Klerk NH, Holt BJ, Wee C, Kendall G, Firth M, et al. Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet. 2003;362:1192–1197. doi: 10.1016/s0140-6736(03)14542-4. [DOI] [PubMed] [Google Scholar]
- 28.Martinez FD, Stern DA, Wright AL, Taussig LM, Halonen M. Differential immune responses to acute lower respiratory illness in early life and subsequent development of persistent wheezing and asthma. J Allergy Clin Immunol. 1998;102(6 Pt 1):915–920. doi: 10.1016/s0091-6749(98)70328-8. [DOI] [PubMed] [Google Scholar]
- 29.Malinovschi A, Fonseca JA, Jacinto T, Alving K, Janson C. Exhaled nitric oxide levels and blood eosinophil counts independently associate with wheeze and asthma events in National Health and Nutrition Examination Survey subjects. J Allergy Clin Immunol. 2013;132:821–827.e1-5. doi: 10.1016/j.jaci.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 30.Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen Y, Cook DG, et al. Prenatal and passive smoke exposure and incidence of asthma and wheeze: systematic review and meta-analysis. Pediatrics. 2012;129:735–744. doi: 10.1542/peds.2011-2196. [DOI] [PubMed] [Google Scholar]
- 31.Kalliola S, Pelkonen AS, Malmberg LP, Sarna S, Hamalainen M, Mononen I, et al. Maternal smoking affects lung function and airway inflammation in young children with multiple-trigger wheeze. J Allergy Clin Immunol. 2013;131:730–735. doi: 10.1016/j.jaci.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 32.Tsai CH, Huang JH, Hwang BF, Lee YL. Household environmental tobacco smoke and risks of asthma, wheeze and bronchitic symptoms among children in Taiwan. Respir Res. 2010;11:11. doi: 10.1186/1465-9921-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanaka K, Miyake Y, Arakawa M, Sasaki S, Ohya Y. Prevalence of asthma and wheeze in relation to passive smoking in Japanese children. Ann Epidemiol. 2007;17:1004–1010. doi: 10.1016/j.annepidem.2007.07.108. [DOI] [PubMed] [Google Scholar]
- 34.Bradley JP, Bacharier LB, Bonfiglio J, Schechtman KB, Strunk R, Storch G, et al. Severity of respiratory syncytial virus bronchiolitis is affected by cigarette smoke exposure and atopy. Pediatrics. 2005;115:e7–e14. doi: 10.1542/peds.2004-0059. [DOI] [PubMed] [Google Scholar]
- 35.Lodge CJ, Zaloumis S, Lowe AJ, Gurrin LC, Matheson MC, Axelrad C, et al. Early-life risk factors for childhood wheeze phenotypes in a high-risk birth cohort. J Pediatr. 2014;164:289–294.e1-2. doi: 10.1016/j.jpeds.2013.09.056. [DOI] [PubMed] [Google Scholar]