Abstract
Purpose
Ventricular repolarization is assessed using the QT interval corrected by the heart rate (QTc) via an electrocardiogram (ECG). Prolonged QTc is associated with an increased risk of arrhythmias and cardiac mortality. As there have been few reports regarding the effects of hyperthyroidism on ventricular repolarization, we studied the association between serum free thyroxine (free T4 [fT4]) and thyroid stimulating hormone (TSH) levels and the QTc interval.
Methods
Thirty-eight patients with hyperthyroidism (<30 years old) were included, and we used their clinical records and available ECGs (between August 2003 and August 2011) to evaluate the association between their fT4 and TSH levels and their QTc interval. In addition, we studied the ECGs of 72 age-matched patients with no hyperthyroidism (control group) and compared their data with that from the patients group.
Results
The QTc duration in patients with hyperthyroidism was significantly prolonged compared to that in the control subjects (P<0.001). In addition, the number of hyperthyroid patients with abnormal prolonged QTc was significantly higher than that in the control group (P<0.001). Among the patients with hyperthyroidism, patients with prolonged QTc and borderline QTc had higher fT4 levels and there was positive correlation between their fT4 levels and their QTc interval (P<0.05). However, no correlation was observed between their TSH levels and their QTc interval.
Conclusion
We report that hyperthyroidism is associated with QTc prolongation. The correlation between the fT4 levels and the QTc interval suggests that thyroid status is associated with QTc values and the risk of cardiac mortality.
Keywords: Hyperthyroidism, Long QT syndrome, Cardiac arrhythmias
Introduction
Hyperthyroidism is a common metabolic disorder in childhood and adolescence. It is associated with serious cardiovascular problems. The effects of thyroid hormone on the cardiovascular system have been widely studied in patients with hypothyroidism or hyperthyroidism1). Ventricular repolarization is assessed with QT interval corrected by heart rate (QTc) in electrocardiogram (ECG). A prolonged QTc is related to an increased risk of sudden arrhythmic cardiac mortality. While it is known that hypothyroidism is associated with QTc prolongation, relatively little is known about the effect of hyperthyroidism on ventricular repolarization. Since the correlation between hyperthyroidism and the duration of the QTc interval has not been extensively investigated, we examined the association of the serum free thyroxine (free T4 [fT4]) and thyroid stimulating hormone (TSH) with the QTc interval.
Materials and methods
1. Study population
We retrospectively examined the clinical records from August 2003 to August 2011 at the Hallym University Hospital in Chuncheon and Hangang of 109 patients with hyperthyroidism who were <30 years of age. After the exclusion of patients for whom no ECG was available, we studied 65 patients. The clinical history, blood chemistry and ECG of all the patients were assessed. We excluded patients with hypokalemia (n=3), since electrolyte abnormalities such as hypokalemia can lengthen the QT interval. We also excluded patients who were taking drugs (propranolol) that could interfere with the cardiovascular system (n=2)2). Due to various technical reasons, the fT4 and TSH levels could only be assessed in 38 of these patients. Additionally, we studied ECG of 72 age-matched patients with no hyperthyroidism at the Hallym university hospital in Chuncheon and Hangang. None of these patients had underlying medical conditions that could affect thyroid status or cardiovascular system. Data from the control group were compared with those from patients with hyperthyroidism. The reference range of the serum fT4 level and the TSH level was 0.7-1.48 ng/dL and 0.35-4.94 ulU/mL, respectively.
2. QTc prolongation
The QT interval was measured as the duration of time between the onset of the QRS complex and the end of the T wave as it returns to baseline2). The length of the QT interval is inversely proportional to heart rate3). To remove the effect of heart rate, the Bezett's formula was used [QTc=QT/(√RR)]4).
European regulatory guidelines were used to categorize the QTc interval into three categories: normal, borderline, and prolonged. For men, the cutoff points were <430 msec (normal), 430-450 msec (borderline), and >450 msec (prolonged), and for women <450 msec (normal), 450-470 msec (borderline), and >470 msec (prolonged)1).
3. Statistical analysis
Statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). The association between the QTc interval and age, gender, fT4 level and TSH level was assessed using the Student t test and the one-way analysis of variance. Pearson correlation analysis was used to assess the correlation between variables. P value <0.05 was considered statistically significant.
Results
1. Clinical characteristics
Clinical characteristics of patients with hyperthyroidism and control subjects were presented in Table 1. In patients with hyperthyroidism, the mean age was 20.34 years. One patient had Down syndrome and 2 patients had Behcet disease. In control group, the mean age was 21.01 years. There was no significant difference in mean age between the two groups.
Table 1. Clinical characteristics of the study groups.
| Characteristic | Hyperthyroidism | Controls |
|---|---|---|
| No. of subjects | 38 | 72 |
| Age (yr), mean±SD | 20.34±6.74 | 21.01±4.26 |
| Gender, male:female | 10:28 | 30:42 |
| Use of drugs causing long QTc interval | 0 | 0 |
SD, standard deviation; QTc, corrected QT.
2. QTc interval of patients with hyperthyroidism and control subjects
We used cutoff points of the European regulatory guidelines mentioned above to categorize patients. There were 7 patients with QTc prolongation, 7 patients with borderline QTc interval, 24 patients with normal QTc interval in the patients group and 1 subject with QTc prolongation, 4 subjects with borderline QTc interval and 67 subjects with normal QTc interval in the control group (P<0.001). The mean QTc interval of hyperthyroid patients and control subjects were 434.16 msec and 411.31 msec, respectively. The QTc duration in patients with hyperthyroidism was significantly prolonged compared to controls (P<0.001) (Table 2).
Table 2. QTc interval and laboratory findings of the study groups.
| Variable | Hyperthyroidism (n=38) | Controls (n=72) | P value |
|---|---|---|---|
| QTc interval (msec) | 434.16±31.98 | 411.31±21.57 | <0.001 |
| TSH (µlU/mL) | 0.09±0.29 | 1.31±0.77 | <0.001 |
| Free T4 (ng/dL) | 4.55±2.75 | 1.19±0.16 | <0.001 |
| QTc interval | <0.001 | ||
| Normal | 24 (63.2) | 67 (93.1) | |
| Borderline | 7 (18.4) | 4 (5.6) | |
| Prolongation | 7 (18.4) | 1 (1.4) |
Values are presented as mean±standard deviation or number (%).
QTc, corrected QT; TSH, thyroid stimulating hormone; Free T4, free thyroxine.
3. Association of the fT4 and TSH levels with the QTc interval in patients with hyperthyroidism
We investigated the association of the fT4 and TSH levels with the QTc interval in hyperthyroid patients. When patients with QTc prolongation and borderline QTc interval were compared with patients with normal QTc duration, the mean fT4 level was 5.86 and 3.78 ng/dL respectively.
The patients with QTc prolongation and borderline QTc had a higher serum fT4 level and there was statistically significant difference (P<0.05). Although the mean TSH level in patients with QTc prolongation and borderline QTc was slightly higher when compared to patients with normal QTc duration, there was no significant difference between the two groups (Table 3).
Table 3. Association between the free thyroxine and thyroid stimulating hormone levels and the QTc interval in patients with hyperthyroidism.
| Prolonged QTc (n=14) | Normal QTc (n=24) | P value | |
|---|---|---|---|
| Free T4 (ng/dL) | 5.86±2.74 | 3.78±2.49 | 0.022 |
| TSH (µlU/mL) | 0.14±0.41 | 0.06±0.19 | 0.408 |
Values are presented as mean±standard deviation
QTc, corrected QT; Free T4, free thyroxine; TSH, thyroid stimulating hormone.
4. Correlations of QTc interval with fT4 and TSH in patients with hyperthyroidism
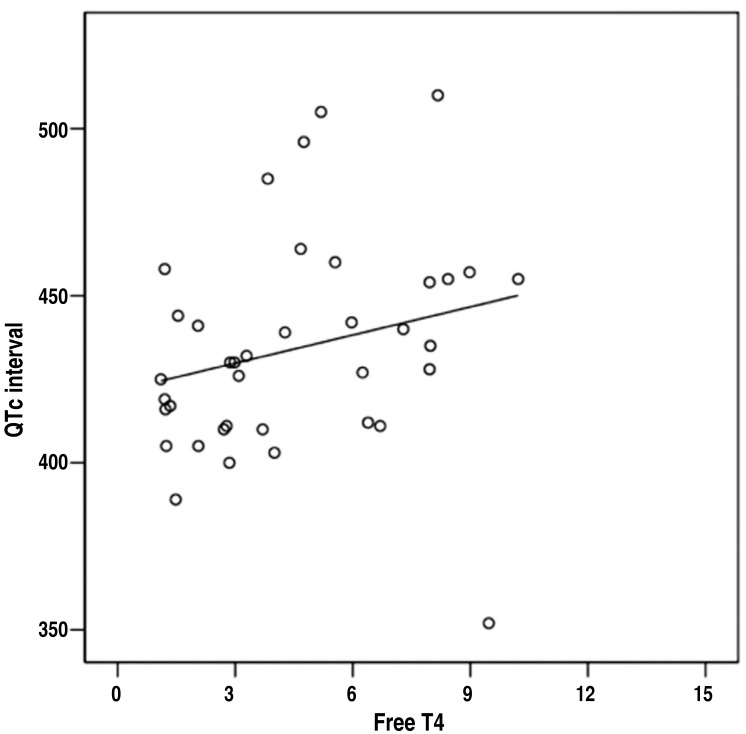
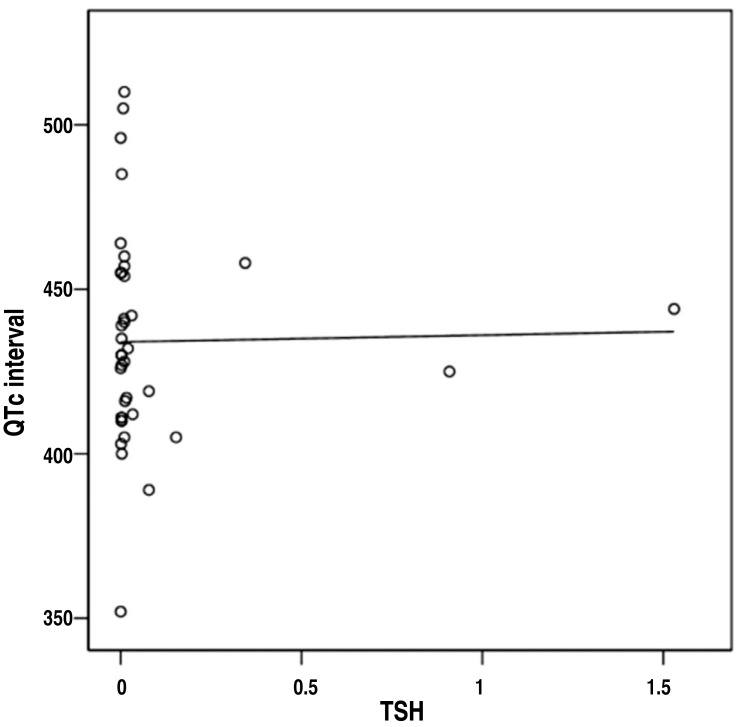
There was a positive correlation between fT4 and QTc interval in patients with hyperthyroidism (Fig. 1). The fT4 was associated with an increased risk of borderline QTc interval or QTc prolongation. No correlation was evident between TSH and QTc interval (Fig. 2).
Fig. 1. Positive correlation between free thyroxine (free T4) levels and the corrected QT (QTc) interval (r=0.389, P=0.016).
Fig. 2. No correlation between thyroid stimulating hormone (TSH) levels and the corrected QT (QTc) interval (r=0.016, P=0.925).
Discussion
In this study, patients with hyperthyroidism showed QTc interval significantly longer than control subjects. QTc prolongation rate was higher in the patients group compared to the control group. In patients with hyperthyroidism, we found that patients with QTc prolongation and borderline QTc had a higher serum fT4 level than patients with normal QTc duration. Furthermore, there was a positive correlation between the fT4 level and QTc interval. A high level of fT4 was associated with a significantly increased risk of borderline QTc interval or QTc prolongation. In contrast, we did not find any correlation of QTc interval with TSH. The mechanism why TSH is not associated with a risk of QTc prolongation is unclear but a possible explanation is that an association between TSH and QTc would be indirect, while fT4 is more directly related to thyroid hormone action on the heart1,5).
The effects of thyroid hormone on the cardiovascular system have been extensively studied6,7,8). While hypothyroidism is associated with a prolongation of the QTc interval, hyperthyroidism is associated with both a decreased and increased repolarization times1,9,10,11,12). In a prospective study comparing 16 patients with Graves disease with a control group, the QTc interval in the patients group was significantly prolonged6). A recent prospective, population-based Rotterdam study of 939 subjects age 55 years and over, that were enrolled and followed up for an average time of 6.7 years, demonstrated an association between hyperthyroidism and QTc prolongation1,3). Additionally, several human studies have reported the same findings13,14,15,16). A likely hypothesis is that excess thyroid hormone may increase the level of cardiac sodium/potassium adenosine triphosphase resulting in an increase in intracellular potassium level and leading to a subsequent membrane hyperpolarization and prolongation of the QTc interval6,17,18).
The majority of the studies performed in the general population have shown that lengthening of QTc interval is associated with an increased risk for arrhythmias and cardiac mortality19). This syndrome may be acquired or congenital3). Congenital prolongation of QT interval is associated with an extremely high incidence of ventricular arrhythmias, including a form of ventricular tachycardia known as torsades de pointes, and sudden death. Drugs that prolong the QT interval are also associated with sudden death resulting from ventricular fibrillation20).with an increased risk for arrhythmias and cardiac mortality19). This syndrome may be acquired or congenital3). Congenital prolongation of QT interval is associated with an extremely high incidence of ventricular arrhythmias, including a form of ventricular tachycardia known as torsades de pointes, and sudden death. Drugs that prolong the QT interval are also associated with sudden death resulting from ventricular fibrillation20).
In conclusion, we report that the level of fT4 is associated with QTc prolongation. The positive correlation between fT4 and QTc interval in patients with hyperthyroidism suggest that thyroid status is associated with QTc values with its risk of cardiac mortality. Colzani et al.6) reported a significantly prolonged QTc in hyperthyroid patients and strong correlation of QTc with serum free triiodothyronine (free T3 [fT3]) and fT4 levels. Free thyroid hormones represents a more useful index of thyroid status than total thyroid hormones, because latter are influenced by variations of thyroid hormone-binding proteins21). Free T3 were not available in this study, we expect that the results may have been more evident if the fT3 level was measured. This study has some further limitations. We studied relatively small number of patients with a limited age. Also, we could not exclude the possibility that prolonged QTc interval was already present in some of the hyperthyroid patients before they developed hyperthyroidism.
Although only a few patients with prolonged QT interval go on to develop malignant dysrhythmias, there still be a possibility of proarrhythmic QTc prolongation in patients with hyperthyroidism3). It is recommended that a regular ECG as well as a serum thyroid index should be considered during follow-up in patients with hyperthyroidism.
Footnotes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.van Noord C, van der Deure WM, Sturkenboom MC, Straus SM, Hofman A, Visser TJ, et al. High free thyroxine levels are associated with QTc prolongation in males. J Endocrinol. 2008;198:253–260. doi: 10.1677/JOE-08-0140. [DOI] [PubMed] [Google Scholar]
- 2.Johnson JN, Ackerman MJ. QTc: how long is too long? Br J Sports Med. 2009;43:657–662. doi: 10.1136/bjsm.2008.054734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradburn P. A case control study to identify and explore association with sudden death and medications that can prolong the QT interval on the electrocardiograph. Birmingham: University of Birmingham; 2009. [Google Scholar]
- 4.Fossa AA, Zhou M. Assessing QT prolongation and electrocardiography restitution using a beat-to-beat method. Cardiol J. 2010;17:230–243. [PubMed] [Google Scholar]
- 5.Volpe R. Rational use of thyroid function tests. Crit Rev Clin Lab Sci. 1997;34:405–438. doi: 10.3109/10408369709006421. [DOI] [PubMed] [Google Scholar]
- 6.Colzani RM, Emdin M, Conforti F, Passino C, Scarlattini M, Iervasi G. Hyperthyroidism is associated with lengthening of ventricular repolarization. Clin Endocrinol (Oxf) 2001;55:27–32. doi: 10.1046/j.1365-2265.2001.01295.x. [DOI] [PubMed] [Google Scholar]
- 7.Klein I, Ojamaa K. Thyrotoxicosis and the heart. Endocrinol Metab Clin North Am. 1998;27:51–62. doi: 10.1016/s0889-8529(05)70297-8. [DOI] [PubMed] [Google Scholar]
- 8.Sarma JS, Venkataraman K, Nicod P, Polikar R, Smith J, Schoenbaum MP, et al. Circadian rhythmicity of rate-normalized QT interval in hypothyroidism and its significance for development of class III antiarrhythmic agents. Am J Cardiol. 1990;66:959–963. doi: 10.1016/0002-9149(90)90933-r. [DOI] [PubMed] [Google Scholar]
- 9.Johansson C, Koopmann R, Vennström B, Benndorf K. Accelerated inactivation of voltage-dependent K+ outward current in cardiomyocytes from thyroid hormone receptor alpha1-deficient mice. J Cardiovasc Electrophysiol. 2002;13:44–50. doi: 10.1046/j.1540-8167.2002.00044.x. [DOI] [PubMed] [Google Scholar]
- 10.Sharp NA, Neel DS, Parsons RL. Influence of thyroid hormone levels on the electrical and mechanical properties of rabbit papillary muscle. J Mol Cell Cardiol. 1985;17:119–132. doi: 10.1016/s0022-2828(85)80015-8. [DOI] [PubMed] [Google Scholar]
- 11.Binah O, Arieli R, Beck R, Rosen MR, Palti Y. Ventricular electrophysiological properties: is interspecies variability related to thyroid state? Am J Physiol. 1987;252(6 Pt 2):H1265–H1274. doi: 10.1152/ajpheart.1987.252.6.H1265. [DOI] [PubMed] [Google Scholar]
- 12.Gomberg-Maitland M, Frishman WH. Thyroid hormone and cardiovascular disease. Am Heart J. 1998;135(2 Pt 1):187–196. doi: 10.1016/s0002-8703(98)70081-x. [DOI] [PubMed] [Google Scholar]
- 13.Linder MA. Periodic paralysis associated with hyperthyroidism: report of three cases. Ann Intern Med. 1955;43:241–254. doi: 10.7326/0003-4819-43-2-241. [DOI] [PubMed] [Google Scholar]
- 14.Fisher J. Thyrotoxic periodic paralysis with ventricular fibrillation. Arch Intern Med. 1982;142:1362–1364. [PubMed] [Google Scholar]
- 15.Owecki M, Michalak A, Nikisch E, Sowinski J. Prolonged ventricular repolarization measured by QTc interval in hyperthyroidism. Pol Merkur Lekarski. 2005;19:24–27. [PubMed] [Google Scholar]
- 16.Galetta F, Franzoni F, Fallahi P, Tocchini L, Graci F, Gaddeo C, et al. Changes in autonomic regulation and ventricular repolarization induced by subclinical hyperthyroidism. Biomed Pharmacother. 2010;64:546–549. doi: 10.1016/j.biopha.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Polikar R, Burger AG, Scherrer U, Nicod P. The thyroid and the heart. Circulation. 1993;87:1435–1441. doi: 10.1161/01.cir.87.5.1435. [DOI] [PubMed] [Google Scholar]
- 18.Shao Y, Ojamaa K, Klein I, Ismail-Beigi F. Thyroid hormone stimulates Na, K-ATPase gene expression in the hemodynamically unloaded heterotopically transplanted rat heart. Thyroid. 2000;10:753–759. doi: 10.1089/thy.2000.10.753. [DOI] [PubMed] [Google Scholar]
- 19.Guntekin U, Gunes Y, Tuncer M, Simsek H, Gumrukcuoglu HA, Arslan S, et al. QTc dispersion in hyperthyroidism and its association with pulmonary hypertension. Pacing Clin Electrophysiol. 2009;32:494–499. doi: 10.1111/j.1540-8159.2009.02310.x. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz PJ, Wolf S. QT interval prolongation as predictor of sudden death in patients with myocardial infarction. Circulation. 1978;57:1074–1077. doi: 10.1161/01.cir.57.6.1074. [DOI] [PubMed] [Google Scholar]
- 21.Bartalena L, Bogazzi F, Brogioni S, Burelli A, Scarcello G, Martino E. Measurement of serum free thyroid hormone concentrations: an essential tool for the diagnosis of thyroid dysfunction. Horm Res. 1996;45:142–147. doi: 10.1159/000184777. [DOI] [PubMed] [Google Scholar]