Abstract
Eagle's syndrome (ES) sometimes called styloid or stylohyoid syndrome is defined as the symptomatic elongation of the styloid process or mineralisation of the stylohyoid ligament. The symptoms related to this condition can be confused with those attributed to a wide variety of facial neuralgias. We report a 34-year-old male patient who presented with a recurrent neck pain and dysphagia. He was diagnosed to have an elongated styloid process. An intraoral transtonsillar shortening of the styloid process was done. We discuss the clinical presentation, diagnosis and treatment of ES as well as a review of the literature.
Background
Eagle's syndrome (ES) is a rare entity that is not commonly suspected in clinical practice.1 The prevalence of individuals with an elongated styloid process in the adult population is estimated to be 4% with a very small percent of these individuals reported to be symptomatic.2 3 The styloid process normally measures 2.5–3 cm in length; when its length exceeds 3 cm, it is said to be elongated.3 (The distance is measured along the posterior aspect of the process between its base and apex). Abnormal angulation rather than elongation of the styloid process may be responsible for the patient's symptoms.3 4 Patients with ES may present with a neck pain, facial pain, ear pain, dysphagia, sore throat or with foreign body symptoms in the pharynx.3 4 Since the symptoms are variable and non-specific, patients seek treatment in several different clinics such as otolaryngology, family practice, neurology, neurosurgery, psychiatry and dentistry.
Case presentation
A 34-year-old male patient presented to the otolaryngology clinic with a complaint of pain in the upper neck region of 6 months duration. The pain was insidious in onset, dull in character and intermittent in nature. The intensity of pain was exacerbated by movements such as looking up and turning the face to the left side. In addition, patients also had a sensation of foreign body in throat on swallowing and sometimes dysphagia. No previous history of trauma. Previous medical and social histories were not helpful.
Physical examination of the neck revealed a tender, fixed, hard bony projection in the left submandibular area at the anterior border of sternocleidomastoid muscle, circular in shape and ∼2×2 cm in size with intact overlying skin. Intraorally, soft and hard tissues looked normal. On palpation of the left tonsillar fossa there was a hard mass consistent with the extraoral finding. Bimanual palpation exacerbated the patient's symptoms.
The patient underwent a chair-side infiltration of 2% lignocaine in the left tonsillar fossa which resulted in immediate relief from the symptoms. The patient was given a primary diagnosis of ES.
Investigations
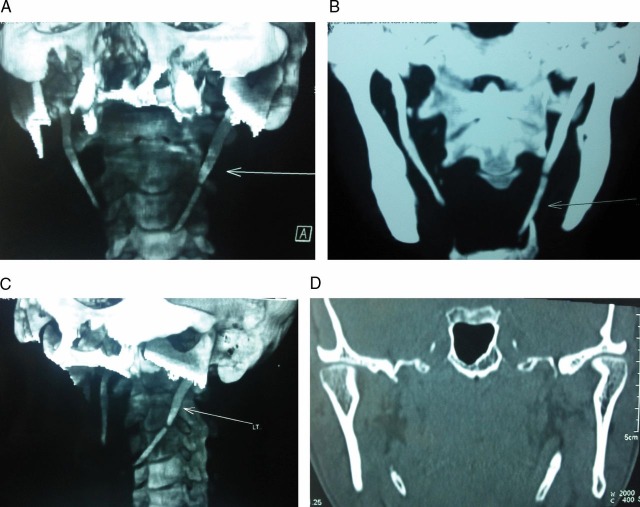
The elongation of the styloid process is confirmed radiologically using conventional radiographs or CT scan. Lateral views are the best to show the length of the styloid process, but antero-posterior views are also needed to determine whether there is bilateral involvement and the presence of lateral deviation. CT scans of the patient head and neck were taken for better defining length, angulation and anatomical relationships of the styloid process. CT showed an elongated left styloid process measuring 5.5 cm (figure 1). The medial angulation of the styloid process was measured as the angle between the vertical line and the body of the process on antero-posterior views. It measures 25° on the left side and 15° on the right side. Anterior angulation was measured on lateral skull x-ray. It measures 40° on the left side and 20° on the right.
Figure 1.
CT showed an elongated left styloid process measuring 5.5 cm.
Differential diagnosis
Since the symptoms of ES are variable and non-specific, it may be readily confused with a wide range of conditions affecting the facial and cervical spine regions. It should be considered in the differential diagnosis of a patient presenting with recurrent neck pain, facial pain, ear pain, dysphagia, sore throat or the sense of foreign body in the pharynx. Differential diagnosis includes laryngopharyngeal dysesthesia, dental malocclusion, temporomandibular arthritis, neuralgia of sphenopalatine ganglia, glossopharyngeal and trigeminal neuralgia, chronic tonsillo-pharyngitis, hyoid bursitis, Sluder's syndrome, histamine cephalgia, cluster type headache, oesophageal diverticula, temporal arteritis, cervical vertebral arthritis, benign or malignant neoplasms and migraine-type headache.
Treatment
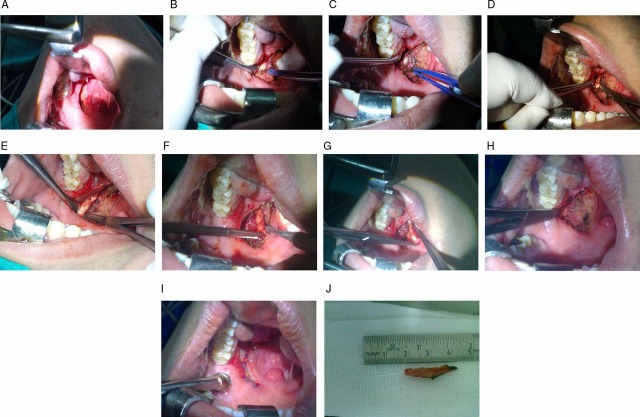
The elongated styloid process of the left side was shortened surgically by an intraoral transtonsillar approach under general anaesthesia. First we removed the palatine tonsil on the left side (figure 2A). The muscles of the pharyngeal wall were dissected, separated and retracted.
Figure 2.
Intraoral transtonsillar shortening of styloid process on the left side. First the palatine tonsil was removed on the left side (A). The muscles of the pharyngeal wall were dissected, separated and retracted. Then, an incision was made on the periosteum of the styloid process. The periosteum was stripped and the styloid process was exposed and caudal part was excised (B–H) and the pharyngeal wall was sutured (I).
Then, an incision was made on the periosteum of the styloid process. The periosteum was stripped and the styloid process was exposed and caudal part was excised (figure 2B–H) and the pharyngeal wall was sutured (figure 2I). The patient's recovery was uneventful.
Ceftriaxone and ibuprofen were administered postoperatively. The patient was discharged on the third postoperative day. The patient's pain was relieved and he remains asymptomatic at follow-up at 6 months.
Outcome and follow-up
The patient remains asymptomatic at follow-up at 6 months and does not have any complains.
Discussion
Eagle's syndrome (ES) is a clinical condition in which there is abnormal ossification of the stylohyoid apparatus, consisting of the styloid process, the attached stylohyoid ligament and the lesser cornu of the hyoid bone.1 Anatomically, the styloid process arises from the temporal bone and passes downwards, forward and medially. Embryologically, it is derived from the Reichert's cartilaginous component of the second branchial arch. Ossification of the styloid process and the stylohyoid ligament leads to an increase in the thickness and length of the styloid process, which then presses on the adjacent structures like the internal jugular vein, carotid artery, facial nerve, vagal nerve, glossopharyngeal nerve and hypoglossal nerve, resulting in various pressure symptoms.4 The styloid process normally measures 2.5–3 cm in length; when the length exceeds 3 cm, it is said to be elongated.3 5 6
The cause of this elongation of the styloid process is not well understood.4 5 It can be idiopathic, congenital (because of the persistence of cartilaginous elements of precursors of the styloid process) or acquired (because of the proliferation of osseous tissue at the insertion of the stylohyoid ligament).4–6
Although Eagle's syndrome is thought to be caused by an elongated styloid process or calcified stylohyoid ligament, many patients with incidental findings of an elongated styloid process are asymptomatic. Abnormal angulation rather than elongation of the styloid process may be responsible for the irritation of a number of structures coursing through the parapharyngeal space.7 There have been studies investigating the angulation and length of the styloid process of the patients without symptoms of the elongated styloid process with three-dimensional CT.7 Anterior angulation of the styloid process is responsible for the symptoms rather than medial angulation.7
The symptoms that patients complain of have varied pathophysiological explanations;1 2 4 5 8 for example, symptoms may be because of: (1) fracture of the styloid process leading to granulation tissue proliferation, which results in pressure on surrounding structures. In a number of cases, ES has developed after fracture of the styloid process. Most fractures result from trauma, though several publications have reported characteristic symptoms after spontaneous avulsion fractures caused by sudden laughter, coughing and epileptic seizures; (2) compression of adjacent nerves, for example, the glossopharyngeal, the lower branch of the trigeminal or the chorda tympani; (3) irritation of the pharyngeal mucosa due to direct compression, or post-tonsillectomy scarring. Contracture of post-tonsillectomy scar tissue towards the elongated styloid process may result in the impingement of one or more of the cranial nerves and impingement of the carotid vessels with irritation of the sympathetic nerves in the arterial sheath and (4) degenerative and inflammatory changes at the tendinous portion of the stylohyoid insertion, which is known as insertion tendonitis.
Eagle primarily described two syndromes:1 3 4 9 10
Classic styloid syndrome: it frequently follows tonsillectomy and is characterised by pain localised in the tonsillar fossa and sometimes accompanied by dysphagia, odynophagia, sore throat, foreign body sensation in the pharynx and rarely temporary voice changes.
The stylo-carotid syndrome: it is not correlated with tonsillectomy. In this condition, the stylohyoid apparatus compresses the internal and/or the external carotid arteries and especially their perivascular sympathetic fibres, resulting in a persistent pain irradiating in the carotid territory.
The diagnosis of ES must be based on a good medical history and physical examination.2 6 It should be possible to feel an elongated styloid process by careful intraoral palpation, placing the index finger in the tonsillar fossa and applying gentle pressure. A styloid process of normal length is usually not palpable. If pain is reproduced by palpation and either referred to the ear, face or head, the diagnosis of an elongated styloid process is very likely.2 Injection of local anaesthetic into tonsillar fossa relieves pain and can be used as a diagnostic tool.2 6 8 The elongation of the styloid process can be confirmed radiologically using conventional radiographs or CT scan.2 6 8 Lateral views are the best to show the length of the styloid process, but antero-posterior views are also needed to determine whether there is bilateral involvement and the presence of lateral deviation. CT helps in surgical planning and allows the physician to better explain the lesion and the surgical details to the patient.2 6 8 10 11
ES can be treated by surgical and nonsurgical means.2 5 Nonsurgical treatments involve reassurance to the patient, analgesics and steroid injections.2 Surgical treatment is the treatment of choice in the literature.5 9 Surgery is in the form of styloidectomy or styloid shortening.5 9 It can be performed using one of the two approaches: intraoral transtonsillar or extraoral.5 9 The intraoral transtonsillar approach provides less operative time, less hospital stay, early return to normal life and better cosmetic.5 9 On the contrary, external surgical approach results in cutaneous scars, longer hospitalisation and risks of facial nerve injuries.5 9 11 The treatment's choice usually depends on the experience of the surgeon.9 In our case we took the intraoral transtonsillar approach. The operative time did not exceed 1.5 hours with no complications observed in the postoperative period. The patient was discharged on the third postoperative day.
Learning points.
Eagle's syndrome (ES) is defined as the symptomatic elongation of the styloid process or calcification of the stylohyoid ligament. The styloid process normally measures 2.5–3 cm in length; when the length exceeds 3 cm, it is said to be elongated. Abnormal angulation rather than elongation of the styloid process may be responsible for the patient's symptoms.
ES should be considered in the differential diagnosis of the patient presenting with recurrent neck pain, facial pain, ear pain, dysphagia, sore throat or the sense of foreign body in the pharynx.
The diagnosis of ES depends on a good medical history, physical examination and palpation of the elongated styloid process in the tonsillar fossa. Injection of local anaesthetic into tonsillar fossa relives pain and can be used as a diagnostic tool. The elongation of the styloid process can be confirmed radiologically using conventional radiographs or better CT scan which is more useful in surgical planning.
The treatment of choice of ES is surgical in the form of styloidectomy or styloid shortening. It can be performed using one of the two approaches: intraoral transtosillar or extraoral. The intraoral transtonsillar approach provides less operative time, less hospital stay, better cosmetic compared with the extraoral approach which results in cutaneous scars and risks of facial nerve injuries.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Fini G, Gasparini G, Filippini F, et al. The long styloid process syndrome or Eagle's syndrome. J Cranio-Maxillofac Surg 2000;28:123–7. [DOI] [PubMed] [Google Scholar]
- 2.Mortellaro C, Biancucci P, Picciolo G, et al. Eagle's syndrome: importance of a corrected diagnosis and adequate surgical treatment. J Craniofac Surg 2002;13:755–8. [DOI] [PubMed] [Google Scholar]
- 3.Prasad KC, Kamath MP, Reddy KJM, et al. Elongated styloid process (Eagle's syndrome): a clinical study. J Oral Maxillofac Surg 2002;60: 171–5. [DOI] [PubMed] [Google Scholar]
- 4.Mendelsohn AH, Berke GS, Chhetri DK. Heterogeneity in the clinical presentation of Eagle's syndrome. Otolaryngol Head Neck Surg 2006;134:389–93. [DOI] [PubMed] [Google Scholar]
- 5.Buono U, Mangone GM, Michelotti A, et al. Surgical approach to the stylohyoid process in Eagle's syndrome. J Oral Maxillofac Surg 2005;63:714–16. [DOI] [PubMed] [Google Scholar]
- 6.Basekim CC, Mutlu H, Gungor A, et al. Evaluation of the styloid process by three-dimensional computed tomography. Eur Radiol 2005;15: 134–9. [DOI] [PubMed] [Google Scholar]
- 7.Yavuz H, Caylakli F, Yildirim T, et al. Angulation of the styloid process in Eagle's syndrome. Eur Arch Otorhinolaryngol 2008;365:1393–6. [DOI] [PubMed] [Google Scholar]
- 8.Raina D, Gothi R, Rajan S. Eagle syndrome. Indian J Radiol Imaging 2009;19:107–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hossein R, Kambiz M, Mohammad D, et al. Complete recovery after an intraoral approach for Eagle syndrome. J Craniofac Surg 2010;21:275–6. [DOI] [PubMed] [Google Scholar]
- 10.Lonka MM, Schousboe LP. Unilateral atypical neck pain in Eagle syndrome. Ugeskr Laeger 2012;174:1242–3. [PubMed] [Google Scholar]
- 11.Koivumäki A, Marinescu-Gava M, Järnstedt J, et al. Trauma induced eagle syndrome. Int J Oral Maxillofac Surg 2012;41:350–3. [DOI] [PubMed] [Google Scholar]