Abstract
A 45-year-old Afro-Caribbean woman attended the emergency department with worsening dysphagia, abdominal distension, abdominal pain, shortness of breath and generalised weakness. She enjoyed preparing and eating cows-feet stew and preferred to cook the meat with the hair and skin intact. On admission she had a severe microcytic anaemia and was malnourished. Abdominal x-ray and CT revealed a large gastric bezoar. At gastrotomy a foul-smelling 2.42 kg mass of hair, leathery skin and altered food were evacuated from the lesser curvature of the stomach. She had undergone the same procedure 8 years earlier to remove a similar trichobezoar.
Following psychiatric review it was deemed that the patient had no underlying psychiatric condition and had full insight into why her trichobezoar had re-occurred. She made a good postoperative recovery and stopped eating cows-feet stew.
Background
Gastric trichobezoar is a rare but well-described clinical disorder characterised by the presence of foreign body composed of hair within the digestive tract. As a result of its rarity, it may be diagnosed after the occurrence of complications such as intestinal obstruction, strangulation and perforation. Trichobezoar is commonly associated with trichotillomania and trichophagia, usually relating to an underlying psychiatric disorder.1 There are no previous reports of human trichobezoar due to the consumption of animal hair as part of a perceived normal diet in the absence of a psychiatric condition. We present the case of a patient who presented with recurrence of trichobezoar due to the regular consumption of cows-feet stew, a dish prepared in various countries, including Jamaica, Nigeria and Vietnam. Unlike other reports of trichobezoar, the patient did not suffer from an underlying psychiatric disorder.
Case presentation
A 45-year-old Afro-Caribbean woman presented to the accident & emergency (A&E) department in December 2010 complaining of vomiting following consumption of solids and liquids. She described a 5-week history of increasing difficulty with food consumption and worsening postprandial vomiting. She had intermittent abdominal pain, abdominal distension, shortness of breath and generalised weakness.
She had been admitted to hospital under the medical team 3 months previously with severe iron deficiency anaemia, significant menorrhagia and cachexia. Her anaemia was attributed to her menorrhagia; she was transfused and discharged after 3 days with no further follow-up. Oesophagogastroduodenoscopy (OGD) was not performed on this occasion because there were no upper gastro-intestinal symptoms. The patient presented to her general practitioner (GP) 3 months later with dysphagia. The GP arranged a direct entry OGD and colonoscopy. OGD revealed a large gastric bezoar (nature unknown) and she was discharged home with advice to see her GP for an urgent surgical referral. Her dysphagia worsened and she presented to A&E 2 days later.
The patient had a medical history of gastric bezoar, treated via laparotomy and gastrotomy in 2003. She was also treated for menorrhagia and dysmenorrhoea under the gynaecologists in September 2009. At that time an MRI had shown multiple uterine fibroids, a left-sided haematosalpinx and ovarian cyst.
She enjoyed having cows-feet soup, a dish that had been introduced to her by her Nigerian father. She had the soup frequently (more than once a week), and preferred to prepare the dish with the animal's hair and skin intact (usually removed). On examination, the patient appeared malnourished and anaemic. There was a large hard mass in her upper abdomen, she had generalised mild abdominal tenderness, and a fullness in the epigastrium.
Investigations
On admission, the patient's full blood count revealed a severe microcytic anaemia (haemoglobin 3.8 and mean corpuscular volume 58.8), and her liver function tests demonstrated evidence of malnourishment (albumin 16 and total protein 51). Abdominal x-ray (figure 1) and CT (figure 2) showed gastric distension and extensive content. On CT the duodenum and remainder of the small bowel were not dilated and contrast was seen to pass through into the small bowel loops. There was no perforation.
Figure 1.
Abdominal radiograph.
Figure 2.
Abdominal CT.
Treatment
The patient was transfused with four units of red blood cells to correct her anaemia. She was reviewed by the dietician for preoperative nutritional optimisation. This was achieved enterally.
She underwent laparotomy and gastrotomy 4 days after presentation; a foul-smelling ball of hair, leathery skin and altered food weighing 2.42 kg were removed (figures 3–5). Part of the trichobezoar was sitting in a large ulcer at the lesser curvature of the stomach (figure 5). It seemed very likely that the ulcer was caused by pressure effect from the trichobezoar; it was oversewn at the time of surgery but follow-up was arranged to surveil and biopsy the ulcer. The stomach was washed with saline and closed in two layers using 2-0 polydioxanone (absorbable) sutures. The patient was started on oral fluids the same day and had a full meal 2 days later.
Figure 3.
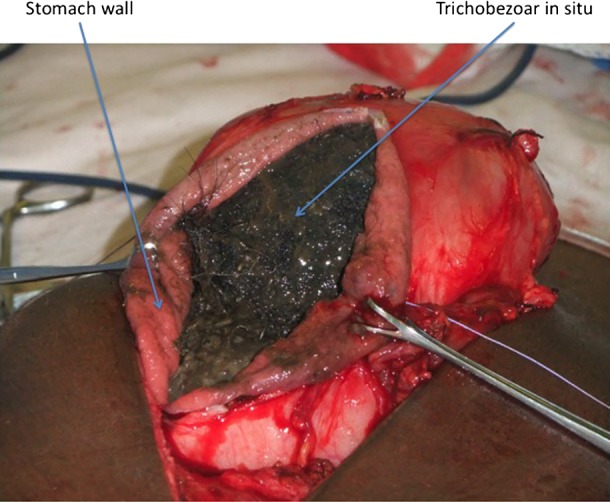
Gastrostomy and tichobezoar in situ prior to evacuation.
Figure 4.

Evacuated trichobezoar.
Figure 5.
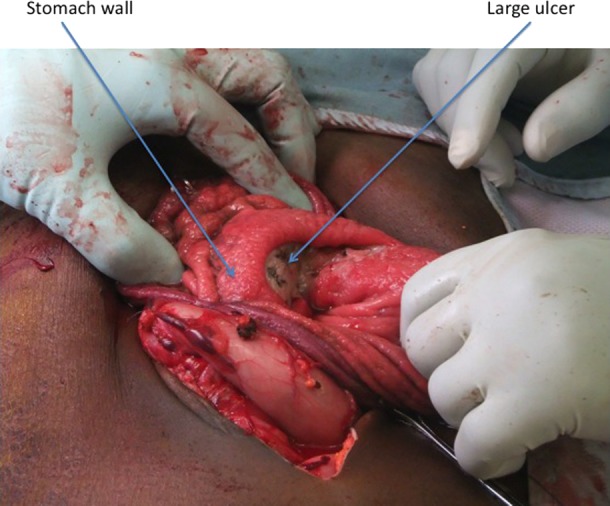
Ulcer at lesser curvature of stomach.
The patient was reviewed by the psychiatric team as it was not clear at the outset that the cause of the bezoar was consumption of food that was culturally normal in the patient's diet. The psychiatric team deemed that the patient did not suffer from trichotillomania and had good insight into how her bezoar had reformed. She had restarted eating cow's feet following surgery for her previous bezoar because she thought that the surgical team caring for her lacked cultural understanding. She was adamant that she would stop eating cows-feet soup, given that the trichobezoar had reoccurred. She was discharged home a week after surgery.
Outcome and follow-up
Surgical follow-up at 4 weeks showed the patient to have recovered well from her gastrotomy; she was re-gaining weight and returning to her premorbid level of fitness. She had stopped eating cows-feet soup and was enjoying a healthy and balanced diet. At 10 months, the patient had made a full recovery and was at a healthy weight. She had not consumed cow's feet since the removal of her trichobezoar.
With respect to the patient's gastric ulcer, she was invited for follow-up OGD with four-quadrant biopsies to ensure resolution, and to exclude malignancy. Despite the surgical team explaining the importance of the investigation to the patient, she did not attend her appointment. The importance of OGD was re-inforced by post and telephone but the patient subsequently failed to attend two further OGD appointments scheduled for her. She declined further investigation. In hindsight, despite the fact that it seemed clear that the ulcer was caused by pressure effect from the trichobezoar (the trichobezoar was sitting in the ulcer crater forming an imprint), it would have been beneficial to biopsy the ulcer at the time of surgery. It is best practice to biopsy all gastric ulcers to exclude malignancy. Follow-up OGD to ensure resolution would have still been required.
Discussion
The word Bezoar originates from the Arabic ‘bazahr’ or ‘badzehr’, or from the Persian ‘Panzer’, all meaning antidote or counter-poison. This is a reflection of the 18th century medicinal use of animal bezoars,2 3 indeed they are still used in oriental medicine today.4 5 Bezoars are foreign bodies found within the digestive tract and have been classified according to their composition, with trichobezoar, the most common type, describing a bezoar made up of hair matter. Bezoars can form from any indigestible material including phytobezoar (vegetable matter), trychophysobezoar (hair and vegetable matter), concretions (hardened organic and inorganic minerals) diosphyrobezoar (persimmon), lactobezoar (milk curd) and even honeycomb.3 6 7
Bezoars may form as a result of delayed (gastric) or enhanced (small bowel) gastric emptying; however, trichobezoars usually form in physiologically normal stomachs. Peristalsis is inefficient at propelling hair strands through the stomach due to their smooth surface. Instead the hair becomes impacted in mucosal folds and is retained in the stomach; the bezoar grows as more hair is ingested and becomes enmeshed in a ball that can expand to occupy the entire stomach. The mass is usually confined to the stomach, though may extend into the small bowel (Rapunzel syndrome).7–9
Patients presenting with trichobezoar usually suffer from psychiatric disorders including trichotillomania (pulling one's own hair out) and trichophagia (hair eating). Overall 30% of patients with trichotillomania have trichophagia, and 1% of these will develop trichobezoar requiring surgical treatment.8 Other associated disorders have also been reported such as pica, anorexia nervosa, obsessive compulsive disorder and abuse.10–12 Trichobezoar is predominantly seen in women; it has been suggested that longer hair length may facilitate trichobezoar formation, though this gender discrepancy is more likely imputed by the higher prevalence of trichotillomania in women.8 13 Although long hair may accumulate more quickly, short hair may form a gastric trichobezoar albeit over longer time periods, as demonstrated by this case.
Curiously our patient was not suspected to suffer from trichotillomania or any other psychiatric disorder. A psychiatric assessment deemed her to have full insight into why and how her trichobezoar had formed. It could be suggested that the patient had a food faddism; as this trichobezoar was a recurrence, and given that the patient preferred to prepare cows-feet stew with some of the cow's hair intact (the authors understand that normal practice is to remove the animal's hair) add weight to this argument. On the other hand, she believed that the hair added to the taste of the soup. The patient commented that she had enjoyed consuming bush meat in the past, especially when, in past years, it had been easier to obtain. She said that bush meat often had a lot of hair. She had eaten bush meat on trips to Benin, Nigeria since a young age, though had visited infrequently over the past 10 years and consumed little bush meat both in Nigeria and in the UK. Cow's feet reminded her of some types of bush meat, which is partly why she enjoyed eating it.
Patients with bezoars may remain asymptomatic for many years, and often present with non-specific symptoms such as abdominal pain, nausea and vomiting. As the mass grows, symptoms may become more severe, and patients can experience complications such as obstruction, gastric ulceration, obstructive jaundice, pancreatitis, strangulation and perforation. Malabsorption may lead to anaemia (iron deficiency and megaloblastic), malnutrition and protein losing enteropathy.7
Treatment of trichobezoar must incorporate both elimination of the mass and prevention of recurrence. Non-invasive (enzymatic dissolution and extracorporeal lithotripsy), endoscopic (including endoscopic lithotipsy, laser fragmentation and coca cola irrigation) and surgical techniques have been used in treatment depending on site, size and consistency of the bezoar.14 15 Laparoscopic removal has been reported; however, the benefits of minimal incisions and reduced infection risk must be weighed against prolonged anaesthetic time and problems with retrieval (especially with large trichobezoars requiring piecemeal removal).14 16
The authors consider this case to be unique as there have been no previous reported cases of gastric trichobezoars forming as a result of human consumption of the another species’ hair as a result of perceived ‘normal’ dietary intake. It is rare for trichobezoars to form as a result of eating hair from a source other than the patient's own body. Patients may eat their pet's hair, and there is a reported case of a boy eating his sister's hair.1 There is a further case of a child eating the sleeves of his cardigan (ie, lamb's wool).17 These patients suffered from underlying psychiatric conditions; none involved a perception of normal food preparation and consumption. Although there have been reported cases of bezoar formation in patients eating what they believed to be a healthy diet, this has not involved the consumption of hair and the subsequent formation of trichobezoar.18
Adding to the uniqueness of this case is the fact that this was the second time this patient had presented with gastric bezoar as a result of eating cows-feet soup. She had previously undergone laparoscopic removal of a large bezoar in 2003 under the same surgical team. There is little information regarding the timeframe over which trichobezoars form. It is likely that there are various contributing factors and thus a wide range in development times. There have been reported cases of trichobezoars forming over as little as 4 months,19 and as evidenced by this case, they may form over many years. This fits with the small quantities of hair that would reach the stomach as a result of eating cows-feet soup, compared to, for example, trichotillomania involving scalp hair.
The authors consider that doctors working in hospitals whose catchment demographic includes communities from countries including parts of Africa, the Carribean and Far East should be aware not only of the possibility of consumption of meat that may still have animal hair intact (be this from cow's feet or other sources—including bush meat) as part of a perceived normal diet, but also the potential health implications of such consumption. This case may be most relevant to doctors working in inner city areas with multiethnic populations. The authors’ trust serves a borough whose non-white ethnic groups make up 41% of its population, ranking sixth within London. The Borough's largest ethnic minority groups are black Africans (11.98%) and black Caribbeans (10.29%). There are multiple inner city markets and shops selling meat products such as cow's feet.
Learning points.
Patients may consume meat with the hair still intact as part of a perceived normal diet and trichobezoar may form as a result of this consumption.
In such cases, diet should be altered to avoid occurrence.
Trichobezoar formation does not always relate to an underlying psychiatric condition.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Christenson GA, Mackenzie TB, Mitchell JE. Characteristics of 60 adult chronic hair pullers. Am J Psychiatry 1991;148:365–70. [DOI] [PubMed] [Google Scholar]
- 2.Williams RS. The fascinating history of bezoars. Med J Aust 1986;145:613–4. [PubMed] [Google Scholar]
- 3.Ersoy YE, Ayan F, Ersan Y. Gastro-intestinal bezoars: thirty-five years experience. Acta Chir Belg 2009;109:198–203. [DOI] [PubMed] [Google Scholar]
- 4.Wang C, Zhao X, Mao S, et al. Management of SAH with traditional Chinese medicine in China. Neurol Res 2006;28:436–44. [DOI] [PubMed] [Google Scholar]
- 5.Zheng A, Moritani T. Effect of the combination of ginseng, oriental bezoar and glycyrrhiza on autonomic nervous activity and immune system under mental arithmetic stress. J Nutr Sci Vitaminol (Tokyo) 2008;54:244–9. [DOI] [PubMed] [Google Scholar]
- 6.Katsinelos P, Pilpilidis I, Chatzimavroudis G, et al. Huge gastric bezoar caused by honeycomb, an unusual complication of health faddism: a case report. Cases J 2009;2:7077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res 2009;7:99–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones GC, Coutinho K, Anjaria D, et al. Treatment of recurrent Rapunzel syndrome and trichotillomania: case report and literature review. Psychosomatics 2010;51:443–6. [DOI] [PubMed] [Google Scholar]
- 9.Gorter RR, Kneepkens CM, Mattens EC, et al. Management of trichobezoar: case report and literature review. Pediatr Surg Int 2010;26:457–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birmingham CL, Cardew S, Gritzner S. Gastric bezoar in anorexia nervosa. Eat Weight Disord 2007;12:e28–9. [DOI] [PubMed] [Google Scholar]
- 11.Wadlington WB, Rose M, Holcomb GW., Jr Complications of trichobezoars: a 30-year experience. South Med J 1992;85:1020–2. [DOI] [PubMed] [Google Scholar]
- 12.Cohen LJ, Stein DJ, Simeon D, et al. Clinical profile, comorbidity, and treatment history in 123 hair pullers: a survey study. J Clin Psychiatry 1995;56:319–26. [PubMed] [Google Scholar]
- 13.Bloch MH, Landeros-Weisenberger A, Dombrowski P, et al. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007;62:839–46. [DOI] [PubMed] [Google Scholar]
- 14.Sharma D, Srivastava M, Babu R, et al. Laparoscopic treatment of gastric bezoar. JSLS 2010;14:263–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee BJ, Park JJ, Chun HJ, et al. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol 2009;15:2265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dorn HF, Gillick JL, Stringel G. Laparoscopic intragastric removal of giant trichobezoar. JSLS 2010;14:259–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hassan AA, Panesar KJ. The Rapunzel syndrome: a rare presentation of trichobezoar. Ulster Med J 1989;58:94–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Harries K, Edwards D, Shute K. Hazards of a ‘healthy’ diet. Ann R Coll Surg Engl 1998;80:72. [PMC free article] [PubMed] [Google Scholar]
- 19.Mehta R, El-Baba MF, Poulik JM, et al. How long does it take for a trichobezoar to form? South Med J 2010;103:847–8. [DOI] [PubMed] [Google Scholar]




