Abstract
Background
Hospitals facing financial uncertainty have sought to reduce nurse staffing as a way to increase profitability. However, nurse staffing has been found to be important in terms of quality of patient care and nursing related outcomes. Nurse staffing can provide a competitive advantage to hospitals and as a result better financial performance, particularly in more competitive markets
Purpose
In this study we build on the Resource-Based View of the Firm to determine the effect of nurse staffing on total profit margin in more competitive and less competitive hospital markets in Florida.
Methodology/Approach
By combining a Florida statewide nursing survey with the American Hospital Association Annual Survey and the Area Resource File, three separate multivariate linear regression models were conducted to determine the effect of nurse staffing on financial performance while accounting for market competitiveness. The analysis was limited to acute care hospitals.
Findings
Nurse staffing levels had a positive association with financial performance (β=3.3; p=0.02) in competitive hospital markets, but no significant association was found in less competitive hospital markets.
Practice Implications
Hospitals in more competitive hospital markets should reconsider reducing nursing staff, as these cost cutting measures may be inefficient and negatively affect financial performance.
Keywords: nurse staffing, hospital competition, financial performance, resource based view
Introduction
Over the past few decades, hospitals have experienced financial uncertainty due to lower reimbursements from payers, higher acuity patients and growing competition from rival organizations and as a result, hospitals are continually seeking ways to reduce costs (Carey, Burgess, & Young, 2011; McCue, Mark, & Harless, 2003; Kane, Shamliyan, Mueller, Duval, & Wilt, 2007). Given the fact that registered nurse wages and benefits constitute a substantial portion of overall hospital costs, hospitals have attempted to reduce nurse staffing as a means to reduce costs and increase profitability (Rivers, Tsai, & Munchus, 2005). However, empirical studies have shown that adequate nurse staffing leads to better outcomes for both patients and nurses without adversely affecting financial performance for hospitals (McCue et al., 2003). Using the Resource-Based View of the Firm (Barney, 1991), this study compares the effect of nurse staffing on financial performance between more competitive and less competitive hospital markets in Florida. Findings from this study could assist managers and hospital administrators in differentiating between efficient and inefficient hospital cost reductions (McKay & Deily, 2005). For instance, if nurse staffing is contributing to higher profitability, reducing the nurse-to-patient ratios could negatively impact both quality of care and overall profitability.
Effect of Nurse Staffing on Patient, Nurse and Financial Outcomes
Registered nurses (RNs) constitute the largest group of health care professionals in the United States and adequate nurse staffing has been linked to measures of both patient and nurse satisfaction, and quality of care provided to patients (Shi & Singh, 2008; Unruh, 2008). The relationship between nurse staffing and measures of patient outcomes (e.g. failure to rescue, mortality, and falls) and nurse outcomes (e.g. satisfaction and turnover) has received significant attention in the literature with often similar conclusions regarding patient and nursing related outcomes. Aiken and colleagues (2002) found that the risk adjusted 30-day mortality and failure-to-rescue rates of hospital surgical patients increased by 7% for every one patient increase in nurse workload. A higher proportion of nurses was associated with lower patient mortality rates (Needleman et al., 2011), lower rates of adverse hospital events, including pressure ulcers, urinary tract infections and falls (Unruh, 2003), as well as lower rates of other adverse patient outcomes (Mark Harless, McCue, & Xu, 2004; Lankshear, Sheldon, & Maynard, 2005; Unruh, 2008). A meta-analysis conducted by Kane and researchers (2007) concluded that higher RN staffing is associated with decreased risk of hospital-related mortality, hospital acquired pneumonia and other adverse patient outcomes. Overall, the majority of literature on nurse staffing and patient outcomes suggests that greater levels of nurses lead to overall better patient outcomes.
Other relevant nurse staffing studies found a significant effect of higher nurse to patient ratios on nurse outcomes, including turnover, burnout, job dissatisfaction and intent to leave (Larrabee et al., 2003; Shaver & Lacey, 2003; Geiger-Brown et al., 2004; Kovner, Brewer, Wu, Cheng, & Suzuki, 2006). Much of the research on job satisfaction focused on how low staffing levels and heavy workloads may lead to nurse dissatisfaction and an increased likelihood nurses will leave their jobs. According to Aiken and colleagues (2002), high patient-to-nurse ratios had a negative impact on nurse job satisfaction; nurses with higher patient loads reporting higher levels of dissatisfaction.
The effects of nurse staffing on patient and nurse outcomes are well established in the literature. However, when considering the impact of nurse staffing on hospital financial outcomes, there are only a few articles that have examined this relationship (Flood & Diers, 1988; Hadley, Zuckerman, & Iezonni, 1996; Cho, Kefetan, Barkauskas, & Smith, 2003; McCue et al., 2003; Dall, Chen, Seifert, Maddox & Hogan, 2009). Specifically, hospital financial performance measures were limited to overall costs while excluding other important measures such as operating and total profit margin (Flood & Diers, 1988; Hadley et al., 1996; Cho et al., 2003). McCue et al. (2003) linked nurse staffing, quality of care and financial performance in a longitudinal study between 1990 and 1995. While this study found increased operating costs with higher levels of registered nurses, there were no significant effects of nurse staffing on profit margins, which questions hospital management practices of reducing nursing staffing during times of financial hardship (McCue et al., 2003). In addition, Rothberg, Abraham, Lindenauer and Rose (2005) performed a cost-effectiveness analysis on patient-to-nurse ratios, and they found that lowering the nurse workload decreased mortality rates and led to overall cost savings. Similarly, Dall and colleagues (2009) determined that hospitals with greater nurse staffing levels resulted in cost savings due to reductions in hospital acquired infections, shorter lengths of stay and improved productivity. However, there is a paucity of research examining the effect of nurse staffing ratios on hospital performance while controlling for market characteristics. Since market structure, and competition specifically, affects the performance of organizations in a given industry (Porter, 1980), we investigate the impact of nurse staffing on financial performance in competitive versus less competitive markets. This study addresses these gaps in the nurse staffing literature. Findings from this study may be useful for managers and hospital administrators to differentiate between efficient and inefficient cost cutting measures (McKay & Deily, 2005) contingent on the competition in their market.
Competitive Hospital Markets
The acute care hospital market environment is generally characterized as hospitals competing for patients, physicians, medical staff and other vital resources, as well as seeking ways to control costs and maintain a high level of quality (Thomson, 1993; Morrisey, 2001). Hospitals are expected to operate like other providers of multifaceted medical services, “differentiating themselves on the basis of services provided, quality of care and other amenities” (Morrisey, 2001, p. 194). However, hospitals in competitive markets face differing challenges and constraints, including competition for scarce resources among competing hospitals and other health care providers. Hospitals with a significant share of the market in a certain geographic region may be better positioned to attract quality medical staff, including registered nurses (Clement, 1987). In the nursing home industry, Starkey, Weech-Maldonado and Mor (2005) found that markets with higher levels of competition require nursing homes to practice more competitive strategies compared to markets with lower levels of competition. This assumption holds true for hospitals where the competitive market structure influences the strategies hospitals pursue in order to thrive financially. For instance, studies on hospital competition have shown that hospitals in more competitive markets will compete on the basis of quality and more extensive services instead of competing solely on price (Keeler, Melnick, & Zwanziger, 1999). Nurse staffing is an integral part of this strategy. Therefore, using the Resource-Based View of the Firm, we argue that given the importance of nurses in the overall delivery of healthcare, hospitals in markets with higher levels of competition must successfully recruit and retain nurses to achieve a competitive advantage over other hospitals in the market. This will have a significant positive effect on overall hospital financial performance. Conversely, hospitals in markets with lower levels of competition do not face the same challenges for scarce resources and the need to compete on quality. For this reason, nurse staffing might not have a significant impact on financial performance in less competitive markets. By maintaining a higher nurse-to-patient ratio, hospitals will gain a competitive advantage and achieve higher overall financial performance in a competitive hospital market.
Theoretical Framework
According to Barney (1991), a firm’s resources includes “all assets, capabilities, organizational processes, firm attributes, information, knowledge, etc. controlled by a firm that enable the firm to conceive of and implement strategies that improve its efficiency and effectiveness” (p. 101). For the purposes of this study, we define firm resources as nurse staffing ratios: nurse staffing is part of the human capital resources of a hospital (Hitt, Bierman, Shimizu, & Kochhar, 2001). Because RNs constitute a majority of the overall health care workforce in hospitals, nurse wages and benefits on average account for a large proportion of hospitals’ total costs (Rivers et al., 2005). As a result, their contribution to the human capital resource is a vital part of the efficiency and effectiveness of hospital operations (McCue et al., 2003). In addition, a positive association between the human capital resources of education, experience and skills and organizational outcomes, including financial performance has been found in earlier studies (Hitt et al, 2001; Huselid, 1995).
Barney’s (1991) seminal work on the Resource-Based View of the Firm predicts that the strategy of an organization is dependent upon the valuable resources and capabilities it possesses, and these resources may assist in establishing a competitive advantage over rival firms. Several assumptions must be met in order to achieve a competitive advantage, including resource heterogeneity and imperfect immobility across firms (Barney, 1991). Hospitals vary in their nurse staffing strategies based on differing levels of nurse “training, experience, judgment, intelligence, knowledge, relationships and insight of the workers in the firm” (Barney, 1991 p. 101), as well as different cultural and social complexities among the nursing staff in various departments within the hospital (Hitt et al., 2001; Barney, 1986). These characteristics represent a barrier to entry and mobility for other firms to replicate their strategy. As a result, the human capital resource of nurse staffing in this case is both causally ambiguous and socially complex, and the ability to comprehend the social phenomena is unknown between hospitals (Barney, 1991). Using the Resource-Based View, Weech-Maldonado, Meret-Hanke, Neff, and Mor (2004) found a positive association between nurse staffing and quality of care in nursing homes. Therefore, using the Resource-Based View, we posit that hospitals with higher nurse staffing are better able to recruit and retain nurses, and will have a competitive advantage in more competitive markets when compared to hospitals with lower nurse staffing.
Also, for a firm to have a sustained competitive advantage, four additional assumptions must be met, in that the resource must be valuable, rare, imperfectly imitable and not substitutable (Barney, 1991). As previously mentioned, nurse staffing affects patient, nurse and financial outcomes, and they are a valuable resource for hospitals and other health care facilities. Because of the predicted U.S. nurse shortage and a fixed amount of nursing education programs to increase the supply, hospitals must compete with rival firms for this valuable resource (Shi & Singh, 2008). Although hospitals can replicate standardized nurse-to-patient ratios, they would be unable to replicate the interactions among the nursing staff and aspects of their work environment. Therefore, in addition to nurse-to-patient ratios, we incorporate work environment as a covariate in our model, as well as an interaction term between nurse staffing, satisfaction and work environment. This 3-way interaction will test the joint moderating effect of nurse staffing, satisfaction and work environment on financial performance of a hospital (Dawson & Richter, 2006). Lastly, although hospitals have tried to substitute RNs as a means of reducing costs, studies have shown that the quality of RNs’ work is not substitutable by licensed practical nurses, nursing aides or other nursing health care providers because of the more rigorous educational requirements and higher level of clinical skills of RNs (Weech-Maldonado et al., 2004). As a result, based on the theoretical framework presented in this paper, we seek to test the following hypothesis:
H1: Hospitals with higher RN-to-patient ratios that are located in more competitive markets will have better financial performance compared to those in less competitive markets.
Methodology
This study linked data from the American Hospital Association (AHA) Annual Survey, the Florida Hospital Uniform Reporting System (FHURS), the Area Resource File (ARF), and the Florida Statewide Nurse Survey for 2008. The AHA Annual Survey Database contains national data on hospitals operating in the U.S. and covers the following areas: demographic information, organizational structure, facilities and services, utilization data, community orientation indicators, physician arrangements, managed care relationships, expenses and staffing. The FHURS contains hospital financial data reported to the Florida Agency of Health Care Administration, including hospital profile data, all balance sheet accounts, daily hospital services and case mix data. ARF contains national county-level data on more than 6000 variables related to health professions, health care facilities, and population data. It is collected from more than 50 sources, such as: the American Medical Association, AHA, U.S. Census Bureau, Centers for Medicare and Medicaid Services, Bureau of Labor Statistics, and the National Center for Health Statistics.
The Florida Statewide Nurse Survey was conducted in 2008 using a 25% random sample of registered nurses (49,385) licensed and residing in the state as of 2007. The sample was obtained from a publicly available mailing list provided by the Florida Board of Nursing, This sampling strategy, employed successfully by other researchers, is described by Aiken et al. (2002) and Neff and colleagues (2011). The survey yielded a response rate of 39% (N=19,471). For the analytical purposes of this study, the sample was restricted to hospital RNs who identified themselves as employed in hospital settings, (of the 19,471 nurses: 2% were retired, 18% reported as not employed, and 55% worked outside of hospital settings). In addition, we used responses from nurses who reported their age between 21 and 65 years: of the total sample, 22% of total sample reported being outside this age range and were not included in the study sample. Therefore, 8,853 nurse surveys were included in the study sample. Although nurses may work in more than one setting, they were instructed to identify their primary hospital work setting from a list of all Florida hospitals present in the survey.
Nurse and hospital level data from Florida in 2008 were merged in this study. There are 251 hospitals in Florida, and we included only acute care hospitals for which there was complete information on structural characteristics (bed size, for-profit status, length-of-stay, and nurse staffing) from the 2008 AHA Annual Survey. We excluded any hospital with 1) less than ten nurse respondents from a statewide nurse survey and 2) if they reported aggregated multihospital systems data. Also, we removed all U.S. Department of Veterans Affairs and rehabilitation and psychiatric facilities because their financial reporting and market are not comparable to acute care hospital systems. Finally, hospitals that did not report nurse staffing data were excluded. After accounting for these exclusion criteria, the total number of hospitals included in this study is 121. The final sample constitutes 45% for-profit and 55% of not-for-profit hospitals in Florida, and this is comparable to 47% for-profit and 53% not-for-profit in the total sample of Florida hospitals in the 2008 AHA dataset.
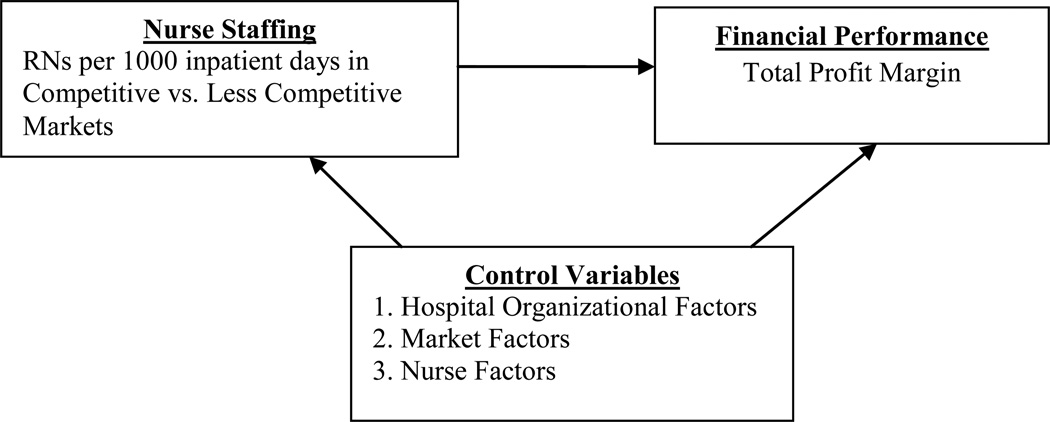
Figure 1 provides a description of the study model examining the association between nurse staffing and financial performance depending on the competition in the market.
Figure 1.
Study Model
VARIABLES AND MEASUREMENT
Table 1 outlines study variables, operational definitions and sources of data.
Table 1.
Variable Descriptions
| Variable | Definition | Source of Data* |
|---|---|---|
| Dependent variable: | ||
| Financial Performance | Total Profit Margin | 2008 FHURS |
| Independent Variable: | ||
| RN staffing ratio | RNs per 1000 inpatient days | 2008 AHA |
| Control Variables: | ||
| Hospital Factors | ||
| Ownership status | Hospital ownership status (For Profit =1, Not For Profit=0) | 2008 AHA |
| Case Mix | Overall hospital case mix | 2008 FHURS |
| Length of Stay | Average length of stay in hospitals | 2008 FHURS |
| Hospital Bed Number | Number of hospital beds | 2008 FHURS |
| Lagged total margin | The total hospital margin reported in 2007 | 2007 FHURS |
| RN – others | Ratio of fulltime RNs to fulltime LPNs and nurse aides | 2008 AHA |
| Market Factors | ||
| Herfindhal index | The sum of the market share squared of hospitals in a county | ARF/AHA |
| Per capita income | Per capita income in the community | ARF |
| Nurse Factors | ||
| Nurse Degree | Nurse reported highest level of education | 2008 Statewide Nurse Survey |
| Nurse Satisfaction | Nurse reported levels of satisfaction (very satisfied =1, All others=0) | 2008 Statewide Nurse Survey |
| Work Environment | Nurse reported hospital work environment (poor, mixed, better) | 2008 Statewide Nurse Survey |
| Intend to Stay | Nurse reported intent to stay at hospital | 2008 Statewide Nurse Survey |
| 3-Way Interaction Term | Interaction between work environment, satisfaction and nurse staffing (categorical variable) | 2008 Statewide Nurse Survey |
AHA – American Hospital Association
FHURS – Florida Hospital Uniform Reporting System
ARF – Area Resource File
Dependent Variable
The dependent variable is total profit margin, which is an overall measure of financial performance in the literature (Gapenski, 1999; Weech-Maldonado et al., 2012). Total profit margin takes into account all revenues (operating and non-operating) and all expenses (operating and non-operating) in an organization, and it measures the percentage of profit a company earns in relation to total sales (Weech-Maldonado et al., 2012). This profitability measure is useful when comparing similar organizations, such as hospitals (Gapenski, 1999). Additionally, net income is used to calculate total profit margin, and this is defined as total revenues minus total costs (including taxes in the case of for-profit hospitals) (Gapenski, 1999). Both net income and total revenues were obtained from the 2008 FHURS data. As a result, the dependent variable of total profit margin used in this study was calculated by dividing net income by the total revenues, as depicted below:
Total Profit Margin = Net Income/Total Revenues
Independent Variable
The independent variable is the ratio of FTE RNs per 1000 inpatient days. This variable was calculated from the AHA survey data. The ratio of RNs per patient day is commonly used in the literature as a proxy measurement of nurse staffing (Unruh, 2008).
Control Variables
Additional covariates in this study describe hospital organizational factors, the market environment in which the hospitals operate, and nurse factors within the hospitals.
Hospital Organizational Factors
The organizational control variables incorporated in this model are ownership status, overall case mix, average patient length of stay, number of hospital beds, lagged total margin performance and the ratio of fulltime RNs to fulltime LPNs and nurse aides. In empirical studies, hospital ownership influences quality of care, costs and overall nurse staffing (McKay & Deily, 2005). Hospitals that operate with a for-profit status are more motivated by increasing shareholder value, and they may have structure and process differences that would impact total margin. Overall case mix measures the complexity of patient conditions in a given hospital’s patient population and a higher case mix indicates a higher acuity of patients, which has an impact on hospital costs and profitability. Average patient length of stay is a measure of hospital efficiency and number of hospital beds reflects hospital staffing capabilities, which can result in economies of scale. The 2007 FURS total margin was included as a lagged variable to control for past financial performance. Lastly, the ratio of RNs to LPNs/nurse aides, calculated from AHA data, accounts for differences in nurse staffing mix (McCue et al., 2003).
Market Factors
Florida county market factors were abstracted from the Area Resource File. Hospital competition was measured by the Herfindhal-Hirschman Index (HHI), an indicator of market concentration that is calculated by taking the sum of hospitals’ market shares squared in a county (Baker, 2001). Market share, which is the proportion of hospitals’ average inpatient days in relation to the total inpatient days in a given market, was calculated from the AHA hospital dataset. Per capita income is a predictor of a hospitals’ ability to collect revenues and make a profit. Hospitals located in areas with lower per capita income typically treat more uninsured individuals and their ability to generate a profit is reduced (McCue et al., 2003). Location of hospital in an urban or rural setting was not added to the models due to high correlation with hospitals in more competitive and less competitive hospital markets.
Nursing Factors
Nurse control characteristics abstracted from the Florida Nurse Survey were aggregated to the hospital level and these include nurse reported measures of level of education, satisfaction, hospital work environment, and intent to stay with current employer. These variables have a significant impact on the overall staffing levels and financial performance of hospitals. Higher educational attainment affects overall quality of patient care (Aiken, Clarke, Sloane, Sochalski, & Silber, 2003) and financial performance of the hospital (McCue et al., 2003). Level of education is measured as the proportion of RNs with a Bachelor of Science in Nursing (BSN) or higher compared to nurses with an Associate Degree or lower.
As previously mentioned, variations in nurse satisfaction can have an impact on turnover and overall profitability of the hospital. Nurses who are more satisfied may be more likely to stay with their current employer, and this would reduce the costs of hiring and training new nurses (Rivers et al., 2007). In the 2008 Florida Statewide Nurse Survey, nurses self-reported job satisfaction via a single item scale “How satisfied are you with your job?” with one of the 4-point likert scale responses “very satisfied, moderately satisfied, a little dissatisfied and very dissatisfied.” This variable was dichotomized to determine the overall level of very satisfied RNs (1 = very satisfied and 0 = all others) because we were most interested in nurses who are very satisfied with their jobs. The percent of very satisfied nurses in the hospital is included as a covariate.
The nurse practice environment measure was assessed using the Practice Environment Scale of the Nursing Work Index (PES-NWI), an extensively validated instrument (Lake 2002). Five subscales, using 31 NWI items, describe the practice environment of registered nurses in hospitals: Nurse Participation in Hospital Affairs (e.g., “staff nurses have the opportunity to participate on hospital and nursing committees”); Nursing Foundations for Quality of Care (e.g., “active in-service/continuing education programs for nurses”); Nurse Manager Ability (e.g. “supervisors are supportive of nurses”; Leadership, and Support of Nurses (e.g., “a supervisory staff that is supportive of the nurses”); Staffing and Resource Adequacy (e.g., “enough registered nurses to provide quality patient care”); and Collegial Nurse–Physician Relations (e.g., “physicians and nurses have good working relationships”). A Likert-type scale indicates the degree (1=strongly disagree to 4=strongly agree) to which various organizational features are present in the practice setting. The PES-NWI subscales were computed for each hospital by averaging the items of each subscale for all the nurses. The Staffing and Resources subscale was excluded in our analysis because it was highly correlated with our measure of staffing – ratio of fulltime RNs per 1000 inpatient days. Hospitals were then stratified into tertiles based on the average across subscales. PES-NWI scores where the lowest tertile is referred to as a ‘poor’ practice environment, the middle tertile as ‘mixed’, and the highest tertile is termed a ‘better’ environment.
To account for the relationship between nurse satisfaction, work environment and nurse staffing, a 3-way interaction term is incorporated to assess the moderating effect of these covariates on hospital financial performance. This variable was operationalized by multiplying nurse work environment, RN staffing, and percent nurses very satisfied, which resulted in a categorical variable (1= better environment/RN staffing/very satisfied; 2= mixed environment/RN staffing/very satisfied; and 3= poor/RN staffing/very satisfied). Finally, we include the proportion of nurses that report an intent to stay with current employer, and this was measured by surveying RNs on whether they planned to be with their current employer one year from now.
Estimation Approach
The unit of analysis is the hospital level and all analyses were conducted using STATA version 11. First, descriptive statistics were conducted to determine the distribution of the variables in the model. A correlation matrix was used to exclude highly correlated variables and reduce the threat of multi-collinearity. To assess the impact of nurse staffing on hospital financial performance for all hospitals in the study, multivariate linear regression was used. When comparing more and less competitive hospital markets, two regression models were estimated from the 121 facilities. To determine whether hospitals were located in more competitive or less competitive markets, the median Herfindahl-Hirschman Index (HHI) was calculated (median HHI is 0.25), and hospitals with an HHI score below the median were considered to be in the more competitive market (n=60 hospitals) and hospitals above the median HHI index were considered to be in a less competitive hospital market (n=61). Multivariate linear regression was performed on these two models to ascertain the effect of nurse staffing on financial performance in more competitive and less competitive hospital markets.
Findings
Descriptive findings of nurse responses to the nurse survey questions are presented in Table 2 for all 121 hospitals. Only an average of 26% of nurses surveyed were reported to be ‘Very satisfied’ with their current job. A mean proportion of 39% of nurses in our survey indicated they had at least a Bachelors degree or higher. While a mean proportion of 25.6% of nurses indicated a ‘Better’ work environment, 43.8% indicated a ‘Poor’ work environment. In addition, nearly 80% of RNs responded that they intend to stay with their current employer.
Table 2.
Descriptive Statistics for Nurse Survey Control Variables (N=121)
| Percentages | Mean(%) | SD(%) | Range(%) |
|---|---|---|---|
| RNs with BSN or higher | 38.94 | 13.47 | 0 – 70.89 |
| RNs surveyed as Very Satisfied | 26.02 | 10.31 | 3.23 – 57.14 |
| RNs surveyed work environment as Better | 25.62 | 43.83 | 0 – 100 |
| RNs surveyed work environment as Mixed | 30.57 | 46.27 | 0 – 100 |
| RNs surveyed intend to stay with current employer | 79.81 | 10.16 | 40 – 100 |
Table 3 shows the descriptive statistics of the outcome, predictor and hospital/market control variables in the model for all 121 hospitals. The mean ratio of fulltime RNs per 1000 inpatient days for our sample was 5.5, and this is comparable to the total hospitals in Florida (n=251) with a mean of 5.6. The mean number of beds per hospital in our sample was 304, and the mean patient length of stay was 4.68 days. The mean calculation for HHI in this sample was 0.26, and the mean overall case mix was 1.31, and this is slightly lower than the average severity of patients’ conditions in the total sample in the AHA hospital dataset of 1.34.
Table 3.
Descriptive Statistics for Outcome, Predictor and Hospital Control Variables (N=121)
| Mean | SD | Range | |
|---|---|---|---|
| Total Profit Margin1 | 1.68 | 7.32 | −21.03 – 18.95 |
| Ratio of Fulltime RNs per 1000 inpatient days2 | 5.5 | 2.5 | 1.5 – 38 |
| Overall case mix | 1.31 | 0.19 | 0.92 – 2.14 |
| Average length of stay | 4.68 | 0.76 | 3.08 – 7.42 |
| Lagged Total Margin Rate | 3.98 | 7.72 | −33.20 – 19.64 |
| Total Hospital Beds | 304.03 | 291.64 | 15 – 2186 |
| Ratio of Fulltime RNs to other fulltime nurses | 3.27 | 1.44 | 1.33 – 11.97 |
| County Competition Index (HHI) | 0.29 | 0.25 | 0.07 – 1 |
| County Per Capita Income | $37,055 | $8,964 | $22332 – 57446 |
Indicates Outcome variable
Indicates Predictor variable
Table 4 displays the comparison between the three regression models, including all facilities model (N=121), the more competitive model (N=60) and the less competitive hospital model (N=61). The adjusted R-squared, which measures the variation in the outcome variable that can be explained by the model, is 0.43 for all facilities, 0.36 for the more competitive model and 0.59 for the less competitive model.
Table 4.
Regression Analysis indicating significant effects of nurse staffing on total profit margin with three models - all facilities (N=121), more competitive (N=60) and less competitive (N=61)
| All Facilities | More Competitive |
Less Competitive |
||||
|---|---|---|---|---|---|---|
| Dependent Variable - Total Profit Margin |
Coef | P>|t| | Coef. | P>|t| | Coef. | P>|t| |
| Adjusted R-squared | 0.43 | 0.36 | 0.59 | |||
| Fulltime RNs per 1000 inpatient days1 | 0.37 | 0.22 | 3.32 | 0.02** | 0.15 | 0.61 |
| Ownership Status | 2.63 | 0.04** | 4.54 | 0.052* | 1.81 | 0.23 |
| Overall Case Mix | 1.49 | 0.65 | 5.70 | 0.27 | 3.11 | 0.54 |
| Average Length of Stay | 0.09 | 0.93 | −0.95 | 0.56 | −0.54 | 0.69 |
| Lagged Total Margin (2007) | 0.61 | 0.00 | 0.36 | 0.00 | 0.88 | 0.00 |
| Total Hospital Beds | 0.00 | 0.91 | 0.001 | 0.69 | −0.004 | 0.10* |
| Ratio of Fulltime RNs to other nurses | −0.51 | 0.22 | −0.49 | 0.42 | −0.42 | 0.55 |
| County Per Capita Income | 0.00 | 0.08* | 0.00 | 0.12 | 0.00 | 0.42 |
| RNs with BSN or higher | −0.04 | 0.40 | −0.02 | 0.82 | −0.08 | 0.13 |
| RNs Surveyed as 'Very Satisfied' | −0.18 | 0.01** | 0.14 | 0.49 | −0.11 | 0.2 |
| Work Environment - Better | 5.11 | 0.05* | 13.67 | 0.01** | 4.75 | 0.12 |
| Work Environment - Mixed | −0.01 | 0.99 | 6.84 | 0.13 | 1.62 | 0.6 |
| Intend to Stay | −0.08 | 0.25 | −0.14 | 0.26 | −0.04 | 0.58 |
| 3-way Interaction (Nurse work environment, RN staffing, and nurse satisfaction) | ||||||
| Mixed/RN Staff/Very Satisfied3 | 0.47 | 0.69 | −0.69 | 0.07* | −0.14 | 0.5 |
| Better/RN Staff/Very Satisfied3 | −0.19 | 0.16 | −1.02 | 0.01** | −0.17 | 0.25 |
| County Competition Index (HHI)2 | −2.24 | 0.35 | ||||
Indicates Predictor Variable
Because competition dichtomized, HHI not included in competitive and non-competitive models
Asterisks denote significance,
prob <=.10,
prob<=0.05
3-Way interaction term reference group is ‘Poor/RN Staffing/Very Satisfied’
Hypothesis 1 stated that a higher ratio of RNs per inpatient day in more competitive hospital markets will be positively associated with overall firm performance, and this was supported by the data. The relationship between nurse staffing and hospital financial performance was significant at the p< 0.05 level in the more competitive model (β=3.3; p=0.02). In other words, an increase in 1 RN per 1000 inpatient days in a competitive market is associated with an increase in the total profit margin. However, RN staffing ratios were not significantly associated with financial performance in less competitive markets.
Other relevant findings from the analyses include the association of the control variable work environment on financial performance. There was a consistent positive relationship between self-reported better work environment and hospital financial performance in the all facilities model (β=5.11; p< 0.05) and the more competitive model (β=13.67; p< 0.01).
Discussion & Practice Implications
Consistent with the Resource-Based View of the Firm (Barney, 1991), findings from this study indicate that registered nurse staffing levels have a significant impact on hospital financial performance in more competitive markets. These findings suggest that registered nurses are valuable resources for hospitals in more competitive markets, and higher levels of nurse staffing contribute to overall firm performance. Therefore, there are several implications for managers and policy-makers. First, these findings may provide additional evidence highlighting the economic value of nursing services (Dall et al., 2009). Although a greater proportion of RNs may initially contribute to increasing operating costs in hospitals, cost savings and profitability in the long-run are achieved through improved productivity, such as reductions in adverse events (e.g. nosocomial infections), decreased length of stay and more efficient care processes (Dall et al., 2009). Given the importance of nurse staffing on financial performance in competitive markets, managers should be cautious about reducing nurse staffing during times of increasing financial pressures. Also, managers and administrators should develop strategies for both retaining and recruiting nurses, as well as balancing cost containment strategies in competitive hospital markets. Reductions in nurse staffing may not only affect financial performance, but hospitals must also consider the impact on quality of patient care and the nursing work environment, especially in competitive markets where hospitals are competing on quality and price (Keeler et al., 1999). However, these findings do not diminish the importance of nurse staffing in less competitive markets. The non-significant findings in less competitive markets could indicate that there are other factors influencing profitability in these hospitals. Therefore, it is important for managers and administrators to continually evaluate nurse staffing levels to maintain adequate staffing ratios for each hospital.
From a policy standpoint, given the scientific evidence on the impact of nursing on both quality of care and financial outcomes, there may be a greater need for governmental agencies to assist in maintaining an adequate supply of nurses in the United States. Although specific nurse-to-patient ratios have not yet been established, recent nursing shortages and ineffective policies to increase the nursing supply necessitate the need for further interventions to ensure improved staffing levels in hospitals and other health care settings (Shi & Singh, 2008). Additionally, the financial benefits of nursing services may also be seen by public and private payers of medical care through prevention of hospital acquired adverse events and reduced length of stay, which could assist in linking quality of care with reimbursement (Dall et al., 2009).
Although not the primary focus of this study, another consideration is the impact of perceived work environment on hospital financial performance. As previously mentioned, there was a positive relationship between better work environment and firm financial performance in the all facilities model (β=5.11; p=0.052) and the more competitive model (β=13.67; p=0.012). The results of this study indicate that better nursing work environment in hospitals could be an important factor for overall firm financial performance. This may be due to the fact that if the work environment is poor in a competitive market, nurses have more options to work for a competing firm, as opposed to less competitive markets where nurses may be more constrained by their location. Further research should be conducted to determine the relationship between nursing work environment, nurse staffing and financial performance among hospitals, as this may provide an understanding as to how the work environment can influence the relationship between nurse staffing and financial performance.
There are several limitations that must be considered for this study. First, all hospitals and nurses surveyed were located in Florida, which limits the ability to generalize the findings to other regions. Second, this study was a cross-sectional design with data from 2008, so there is a limited ability to determine overall causality among the variables, and further longitudinal research should be conducted to evaluate the relationship over time. Also, there may be a problem with endogeneity and omitted variable bias that is contributing to overall firm financial performance. However, this is the first study to our knowledge that combines a statewide nurse survey with administrative hospital data to establish the effects of individual nursing factors on hospital performance. Future research could analyze the effects of nurse staffing on financial performance over a longer time period. Additionally, future research could determine the effects of nurse staffing on financial performance in individual hospital units to evaluate hospital staffing patterns within various hospital departments. Another potential area for future inquiry is analyzing the impact of nurse staffing on a firm’s cost and revenue to evaluate the processes that lead to greater profitability in these organizations.
Acknowledgements
This work is a product of resources through the Blue Cross Blue Shield of Florida Center for Health Care Access, Patient Safety and Quality Outcomes at the University of Florida. This Center is a joint research and education center for the Colleges of Nursing and Public Health & Health Professions. It is supported by a generous gift from the Blue Cross Blue Shield of Florida Inc. (BCBSFL) with the ultimate goal of improving health and health care for the citizens of Florida. The Center’s faculty, staff and students are accountable for the quality and integrity of all work conducted in the Center. BCBSFL does not in any way influence or endorse the research, projects, publications or programs of the center, nor does BCBSFL necessarily support findings or recommendations from the Center.
Disclosure of Funding. This study is partially funded by a National Institute of Health (NIH) grant #NIH-NINR-1K01NR011174-01A1.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Damian Everhart, University of Florida - Department of Health Services Research, Management & Policy, 101 S. Newell Drive, Room 4151, P.O. Box 100195, Gainesville, FL 32610-0195, (352)-216-3930, gatoreng@ufl.edu.
Donna Neff, University of Florida - College of Nursing.
Mona Al-Amin, Sawyer School of Business – Healthcare Administration Department, Suffolk University.
June Nogle, University of Florida - College of Medicine, Institute for Child Health Policy.
Robert Weech-Maldonado, University of Alabama-Birmingham, Department of Health Services Administration.
References
- Aiken L, Clarke S, Sloane D, Sochalski J, Silber J. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken L, Clarke S, Cheung R, Sloane D, Silber J. Educational levels of hospital nurses surgical patient mortality. JAMA. 2003;290(12):1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker L. Measuring competition in health care markets. Health Services Research. 2001;36(1):223–251. [PMC free article] [PubMed] [Google Scholar]
- Barney J. Organizational culture: can it be a source of sustained competitive advantage? Academy of Management Review. 1986;11(3):656–665. [Google Scholar]
- Barney J. Firm resources and sustained competitive advantage. Journal of Management. 1991;17(1):99–120. [Google Scholar]
- Carey K, Burgess J, Young G. Hospital competition and financial performance: the effects of ambulatory surgery centers. Health Economics. 2011;20(5):571–581. doi: 10.1002/hec.1617. [DOI] [PubMed] [Google Scholar]
- Choi J, Bakken S, Larson E, Du Y, Stone P. Perceived nursing work environment of critical care nurses. Nursing Research. 2004;53(6):370–378. doi: 10.1097/00006199-200411000-00005. [DOI] [PubMed] [Google Scholar]
- Cho S, Ketefian S, Barkauskas V, Smith D. The effects of nurse staffing on adverse events, morbidity, mortality, and medical costs. Nursing Research. 2003;52(2):71–79. doi: 10.1097/00006199-200303000-00003. [DOI] [PubMed] [Google Scholar]
- Clement J. Does hospital diversification improve financial outcomes? Medical Care. 1987;25:988–1001. doi: 10.1097/00005650-198710000-00007. [DOI] [PubMed] [Google Scholar]
- Dall T, Chen Y, Seifert R, Maddox P, Hagan P. The economic value of professional nursing. Medical Care. 2009;47(1):97–104. doi: 10.1097/MLR.0b013e3181844da8. [DOI] [PubMed] [Google Scholar]
- Dawson J, Richter A. Probing three-way interactions in moderated multiple regression: development and application of a slope difference test. Journal of Applied Psychology. 2006;91(4):917–926. doi: 10.1037/0021-9010.91.4.917. [DOI] [PubMed] [Google Scholar]
- Flood S, Diers D. Nurse staffing, patient outcomes, and cost. Nurse Management. 1988;19(5):34–43. [PubMed] [Google Scholar]
- Gapenski LC. Healthcare Finance: An Introduction to Financial and Accounting Management. Chicago: Health Administration Press; 1999. [Google Scholar]
- Geiger-Brown J, Trinkoff A, Nielson K, Lirtmunlikaporn S, Brady B, Vasquez E. Nurses’ perception of their work environment, health, and well-being: a qualitative perspective. AAOHNJ. 2004;52(1):16–22. [PubMed] [Google Scholar]
- Hadley J, Zuckerman S, Iezzoni L. Financial pressure and competition. Medical Care. 1996;34(3):205–219. doi: 10.1097/00005650-199603000-00002. [DOI] [PubMed] [Google Scholar]
- Hitt M, Bierman L, Shimizu K, Kochhar R. Direct and moderating effects of human capital on strategy and performance in professional service firms: a resource-based perspective. Academy of Management. 2001;44(1):13–28. [Google Scholar]
- Huselid M. The impact of human resource management practices on turnover, productivity, and corporate financial performance. Academy of Management Journal. 1995;39(3):635–672. [Google Scholar]
- Kane R, Shamliyan T, Mueller C, Duval S, Wilt T. The association of registered nurse staffing levels and patient outcomes: a systematic review and meta-analysis. Medical Care. 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- Keeler E, Melnick G, Zwanziger J. The changing effects of competition on non-profit and for-profit hospital pricing behavior. Journal of Health Economics. 1999;18:69–86. doi: 10.1016/s0167-6296(98)00036-8. [DOI] [PubMed] [Google Scholar]
- Kovner C, Brewer C, Wu Y, Cheng Y, Suzuki M. Factors associated with work satisfaction of registered nurses. Journal of Nursing Scholarship. 2006;38(1):71–79. doi: 10.1111/j.1547-5069.2006.00080.x. [DOI] [PubMed] [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Research in Nursing and Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lankshear A, Sheldon T, Maynard A. Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Advances in Nursing Science. 2005;28(2):163–174. doi: 10.1097/00012272-200504000-00008. [DOI] [PubMed] [Google Scholar]
- Larrabee J, Janney M, Ostrow C, Withrow M, Hobbs G, Burant C. Predicting registered nurse job satisfaction and intent to leave. Journal of Nursing Administration. 2003;33(5):271–283. doi: 10.1097/00005110-200305000-00003. [DOI] [PubMed] [Google Scholar]
- Mark B, Harless D, McCue M, Xu Y. A longitudinal examination of hospital registered nurse staffing and quality of care. Health Services Research. 2004;39(2):279–300. doi: 10.1111/j.1475-6773.2004.00228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCue M, Mark B, Harless D. Nurse staffing, quality, and financial performance. Journal of Health Care Finance. 2003;29(4):54–76. [PubMed] [Google Scholar]
- McKay N, Deily M. Comparing high and low performing hospitals using risk-adjusted excess mortality and cost inefficiency. Health Care Management Review. 2005;30(4):347–360. doi: 10.1097/00004010-200510000-00009. [DOI] [PubMed] [Google Scholar]
- Morrisey M. Competition in hospital and health insurance markets: a review and research agenda. Health Services Research. 2001;36(1):191–221. [PMC free article] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P, Pankratz V, Leibson C, Stevens S, Harris M. Nurse staffing and inpatient hospital mortality. New England Journal of Medicine. 2011;364(11):1037–1045. doi: 10.1056/NEJMsa1001025. [DOI] [PubMed] [Google Scholar]
- Neff D, Cimiotti J, Heusinger A, Aiken L. News report from the frontlines: analysis of a statewide nurse survey. Nursing Forum. 2011;46(1):4–10. doi: 10.1111/j.1744-6198.2010.00201.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter M. Competitive Strategy: Techniques for Analyzing Industries and Competitors. New York: Free Press; 1980. [Google Scholar]
- Rivers P, Tsai K, Munchus G. The Financial Impacts of the Nursing Shortage. Journal of Health Care Finance. 2005;31(3):52–64. [PubMed] [Google Scholar]
- Rothberg M, Abraham I, Lindenauer P, Rose D. Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Medical Care. 2005;43(8):785–791. doi: 10.1097/01.mlr.0000170408.35854.fa. [DOI] [PubMed] [Google Scholar]
- Shaver K, Lacey L. Job and career satisfaction among staff nurses: effects of job setting and environment. Journal of Nursing Administration. 2003;33(3):166–172. doi: 10.1097/00005110-200303000-00008. [DOI] [PubMed] [Google Scholar]
- Shi L, Singh DA. Delivering Health Care in America: A Systems Approach. 4th edition. Sudbury, Massachusetts: Jones and Bartlett; 2008. [Google Scholar]
- Starkey K, Weech-Maldonado R, Mor V. Market competition and quality of care in the nursing home industry. Journal of Health Care Finance. 2005;32(1):67–81. [PubMed] [Google Scholar]
- Thomson R. Competition among hospitals in the United States. Health Policy. 1993;27:205–231. doi: 10.1016/0168-8510(94)90117-1. [DOI] [PubMed] [Google Scholar]
- Unruh L. Licensed nurse staffing and adverse events in hospitals. Medical Care. 2003;41(1):142–152. doi: 10.1097/00005650-200301000-00016. [DOI] [PubMed] [Google Scholar]
- Unruh L. Nurse staffing and patient, nurse and financial outcomes. American Journal of Nursing. 2008;108(1):62–71. doi: 10.1097/01.NAJ.0000305132.33841.92. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Meret-Hanke L, Neff M, Mor V. Nurse staffing patterns and quality of care in nursing homes. Health Care Management Review. 2004;29(2):107–116. doi: 10.1097/00004010-200404000-00004. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Laberge A, Pradhan R, Johnson C, Zhou Y, Hyer K. Nursing Home Financial Performance: The Role of Ownership and Chain Affiliation. Health Care Management Review. 2012 doi: 10.1097/HMR.0b013e31823dfe13. [DOI] [PubMed] [Google Scholar]