Abstract
Purpose
To evaluate the quantity and perceived quality of Ophthalmology resident surgical experience with surgical astigmatism management, new technology IOL implantation, and corneal refractive surgery.
Setting
US ACGME Ophthalmology Residency current members and recent graduates via electronic survey.
Methods
A 43-question survey was emailed to all resident members of ASCRS, ASCRS members in practice for 5 years or less, and to residency program directors of 118 U.S. ACGME accredited ophthalmology programs in June 2010. The surveys were performed electronically using Survey Monkey, a commercially available Internet-based survey web service.
Results
Two hundred and seventy-six surveys were included. Most of the respondents (88.7%) served as primary surgeon in over 100 cataract surgeries, and 89.4% of respondents felt their exposure to cataract surgery was either “adequate” or “excessive”. Fifty-two percent of respondents had not performed corneal relaxing incisions and 60% of respondents had no experience implanting a toric IOL. Twenty-two percent of respondents had experience implanting a presbyopia-correcting IOL, while most (??%) felt that this training should begin in residency. Over 75% of respondents had not performed LASIK or surface ablation procedures; while most (80.9%) felt that this training should begin in residency.
Conclusions
While total cataract case numbers appear adequate, there are significant perceived deficiencies in current resident training models in preparing future surgeons for procedures and techniques they are likely to utilize after residency.
Cataract and corneal refractive surgery are the most common ophthalmic surgical procedures performed in the United States and worldwide. These fields are rapidly evolving in terms of techniques, available technology, and patient expectations. Over the past ten years a multitude of new intraocular lens (IOL) styles with unique optical properties have become available, including toric, multifocal, and pseudoaccommodative IOLs. Corneal refractive surgical techniques continue to evolve as well, including the advent of femtosecond laser technology for LASIK flap creation. The addition of these refractive surgical technologies has changed the landscape of ophthalmic practice, with increasing numbers of patients desiring the lifestyle benefits these technologies can provide.
The ophthalmology Residency Review Committee (RRC) and the Accreditation Council for Graduate Medical Education (ACGME) have established minimum requirements for operative experience for residents (http://www.acgme.org/acWebsite/navPages/nav_240.asp). The current requirements include residents serving as primary surgeon for 86 cataract surgeries and as either primary or assistant surgeon for 6 corneal refractive surgeries (Figure 1). These requirements, however, do not specify refractive surgical technique or specific exposure to new technology IOLs
Figure 1.
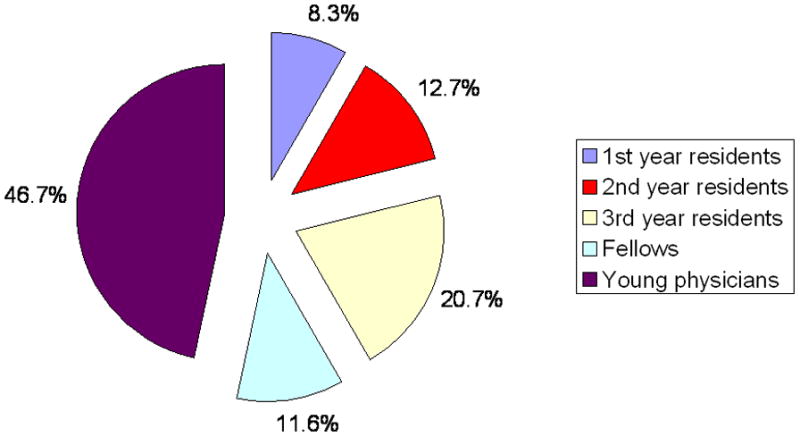
Pie chart shows the percentage of respondents at each training level.
Several prior publications have evaluated the objective surgical practice patterns and outcomes of residents for cataract and refractive surgeries in the United States1–7 demonstrating adequate competency for basic surgical techniques. The adaptation of core competencies7, structured surgical curriculums8, microsurgical labs9 and surgical simulation devices10–13 are all currently utilized to varying degrees to help solidify basic surgical techniques.14 However, previous surveys have also identified advanced cataract techniques and corneal refractive surgery as areas of perceived underexposure in residency15, 16 (possibly also Lee/Koch- don’t know, waiting on article). Further, Kwon, et. al., recently demonstrated that at least forty-five percent of U.S. residencies do not offer any resident-performed LASIK experience.15 It therefore seems plausible that residents may need and could effectively gain additional exposure to more advanced refractive corneal and cataract surgical techniques during residency without compromising any primary training competency.
In order to better understand the current resident refractive surgical experience, the American Society of Cataract and Refractive Surgery Young Physicians and Residents Committee created a survey of current residents, fellows and physicians in practice five years or less. To the best of our knowledge, this is the first direct survey of residents to evaluate both the objective quantity and perceived quality of resident surgical experiences with the management of new technology IOL implantation, and corneal refractive surgery.
Materials and Methods
A comprehensive 43-question survey, created by the American Society of Cataract and Refractive Surgery (ASCRS) Young Physicians and Residents (YPR) committee, was emailed to all resident members of ASCRS (postgraduate years 2–4), ASCRS members identified as being in practice for 5 years or less, and to residency program directors of 118 ACGME accredited ophthalmology programs throughout the United States in June 2010. The surveys were sent and collected electronically using Survey Monkey, a commercially available Internet-based survey web service. Only one survey submission per YPR section member was allowed. Survey questions were designed to determine the objective quantity of surgical procedures performed in residency, as well as the perceived adequacy of training (inadequate, adequate or excessive) for particular surgical skills. The Survey questions are shown as appendix 1.
Statistical Analysis
Responses to the survey were coded in the Microsoft Excel (Microsoft Office 2007) for analysis. Frequency data were tabulated and used for descriptive statistics. Analyses were done in the whole group and subgroups stratified by respondent training level.
Results
A total of 2279 emails were sent to ASCRS young physicians and residents and to the residency program directors of all the ACGME-accredited ophthalmology programs in June 2010, which corresponded to the last month of an academic year. A total of 285 surveys (12.5%) were completed. The data was collected between June 10, 2010 and July 6, 2010. A total of 276 surveys (96.8% of completed surveys) were included for data analysis; nine surveys were excluded for being duplicates (7) or because they contained no information (2). Of the respondents, there was a relatively even distribution between members in the second or third year of residency and those in the first 5 years of their practice (Figure 1)
First exposure as primary surgeon to phacoemulsification surgery
Eighteen percent of respondents started phacoemulsification surgery (49/275) during their first year of residency, 61.1% (168/275) either began performing or planned to start phacoemulsification surgery during their second year of residency, and 21.1% (58/275) of respondents in their third year.
Number of phacoemulsification cases performed during residency and quality of exposure
Most respondents performed more than 100 surgeries as primary surgeon; 89.4% (245/274) respondents felt their exposure was either “adequate” or “excessive” (Figure 2).
Figure 2.
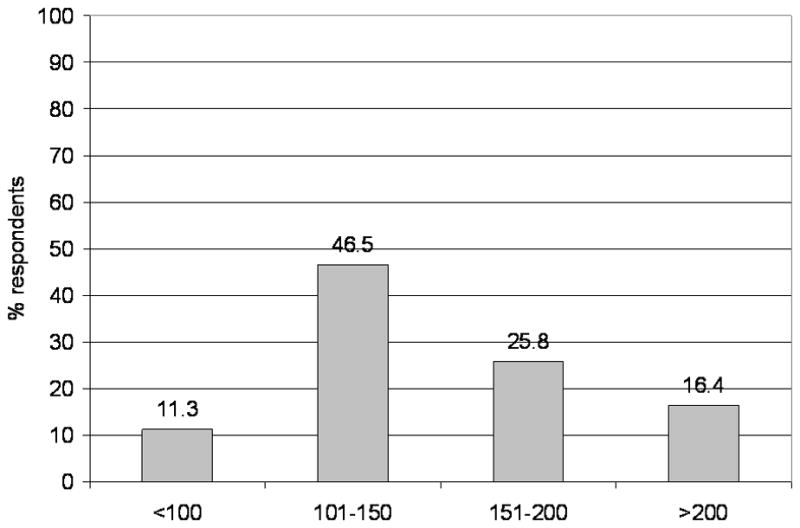
Number of phacoemulsification cases performed during residency.
Management of astigmatism during cataract surgery and quality of exposure
Of the 272 respondents, 51.8% had not performed any corneal relaxing incisions, and 37.1% of the respondents were graduating residency without having any experience with these (Figure 3). Sixty-nine percent of respondents expressed that their training with corneal relaxing incisions was “inadequate.”
Figure 3.
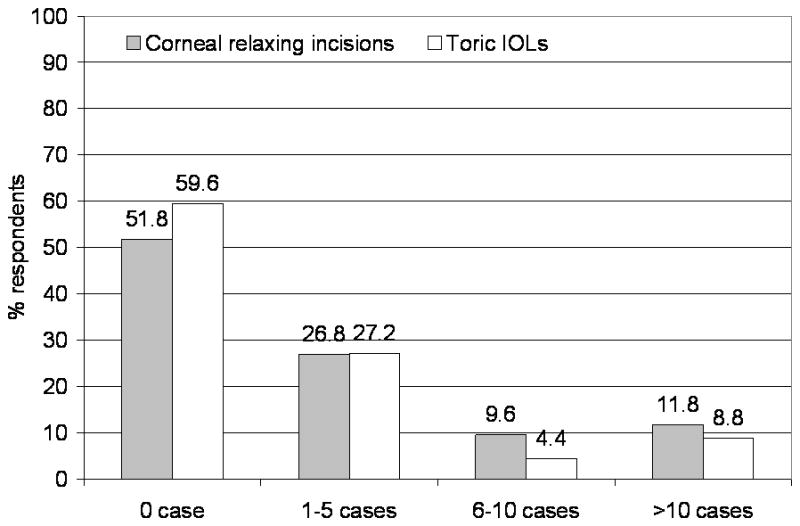
Number of astigmatism management cases performed during cataract surgery.
Sixty percent of respondents had no experience implanting a toric IOL (Figure 3) and 66.1% of the respondents believed that the exposure to toric IOL technology was “inadequate.” Accordingly, a vast majority of respondents (86.7%) believed that this training for toric IOL implantation should begin in residency.
Experience with presbyopia-correcting IOLs
Seventy-eight percent of respondents had not implanted a presbyopia-correcting IOL (Figure 4) and 77% felt that their exposure to this technology was “inadequate”. When asked about the appropriate timing for such training, 61% stated “during residency” (Figure 5).
Figure 4.
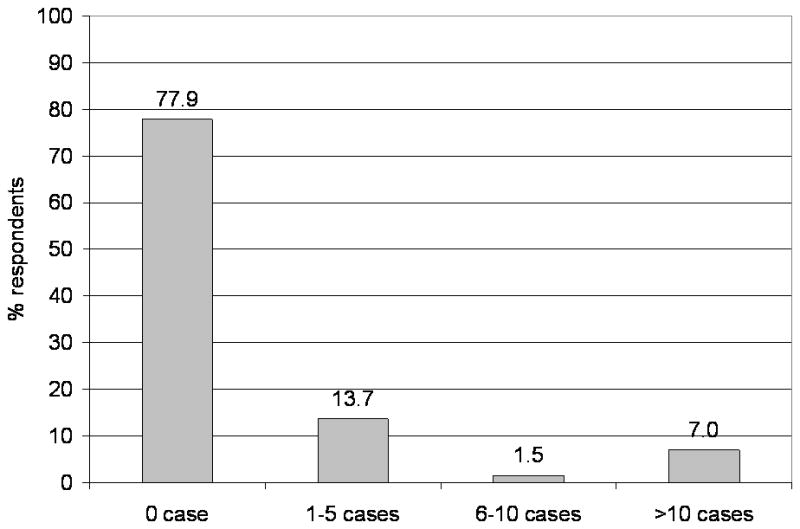
Number of presbyopia-correcting IOLs performed during cataract surgery.
Figure 5.
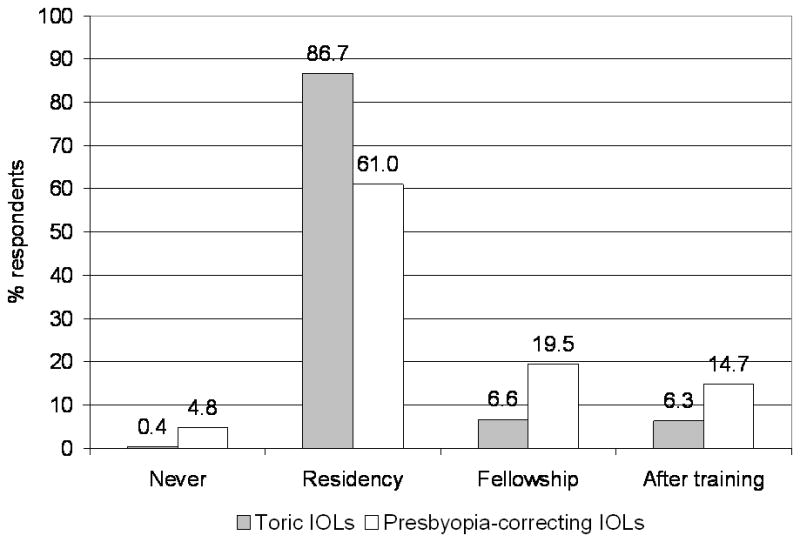
Appropriate timing to start training of toric IOLs and presbyopia-correcting IOLs.
Experience with laser corneal refractive surgery
Of the respondents, only 55.5% stated they had a formal refractive surgery component to their curriculum, while 45% did not have any opportunities to become certified on an excimer laser platform, 59.7% did not have any microkeratome training opportunities available during residency, and only 29% had the opportunity to receive femtosecond laser certification (Figure 6).
Figure 6.
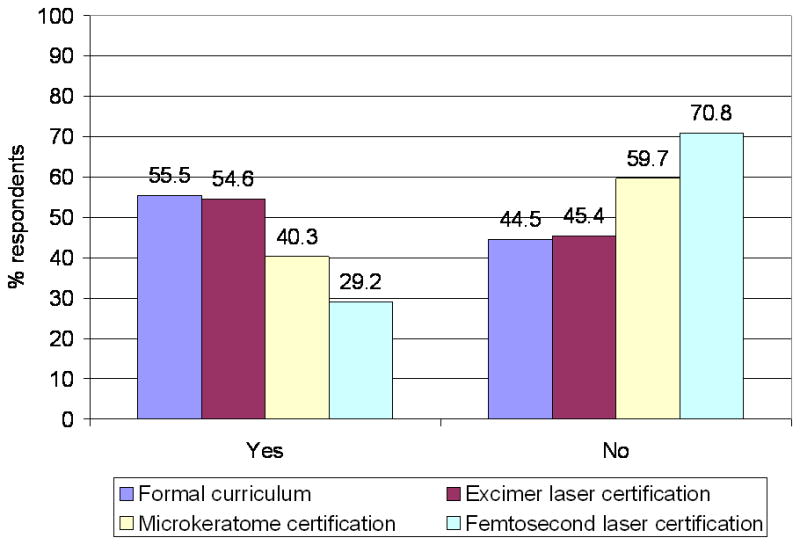
Formal refractive surgery curriculum, excimer laser, microkeratome and femtosecond laser certification opportunities.
Seventy-six percent (208/274) surveyed stated they had not performed any LASIK procedures and 77% (207/269) had no experience with surface ablation procedures (Figure 7). Similarly, seventy-five percent (204/272) felt their exposure to excimer laser surgery was “inadequate” and 80.9% (220/272) of respondents felt this training should occur during residency.
Figure 7.
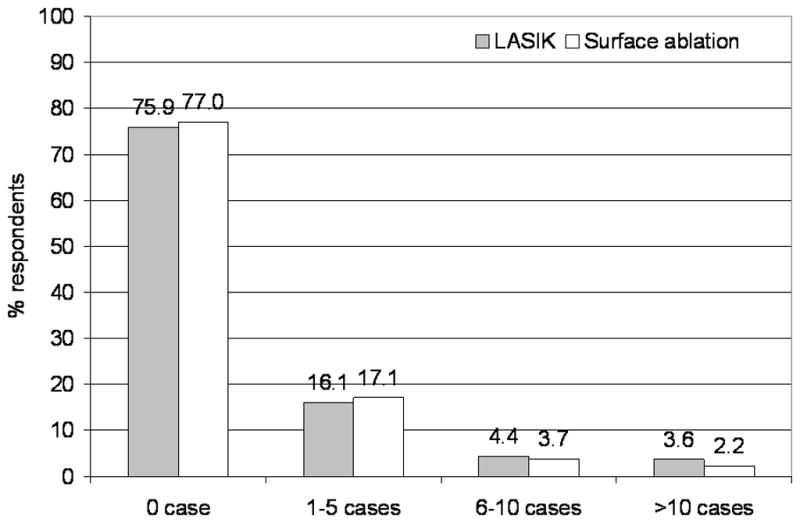
Number of refractive surgery procedures performed during residency.
Discussion
The results of this survey suggest that, while total cataract case numbers appear subjectively adequate, there are significant perceived deficiencies in current resident training models in preparing future surgeons for many of the more advanced procedures and techniques they are likely to utilize immediately after completing residency. Encouragingly, 89% of the respondents had performed over 100 cataract extractions, which was well above the minimum RRC/ACGME requirement. Further, the above average cataract volume suggests that most residents are exposed to a sufficient number of “average” cases, so that the later stages of their resident training could have increased focus on more advanced techniques without compromising core training.
The current RRC/ACGME cataract surgery requirement of a finite number of cases without regard to technique does not address the nuances of modern cataract surgery, which is increasingly becoming refractive in nature. Most respondents complete their training without real or perceived exposure to presbyopia or astigmatism correction strategies, and most surgeons, regardless of stage of training, felt that this exposure should occur during residency.
The responses to the questions regarding refractive surgery training also demonstrate a large deficit in overall resident training in this field. Despite the increasing role of refractive surgical education in the curriculum, with a American Academy of Ophthalmology Basic and Clinical Sciences book devoted specifically to the subject and inclusion minimum requirements for surgical practice or observation, only half of the residents reported having a formal refractive surgery component in their surgical curriculum, and only one-quarter had any actual surgical experience with LASIK or surface ablation procedures. Accordingly, 75% felt their exposure to excimer laser surgery training was inadequate and almost 81% of respondents felt this training should occur during residency.
Given the data of this survey, what options should be explored in order to implement a more expansive surgical education that would more adequately prepare residents in lens and corneal refractive surgery? The surgical management of astigmatism, premium IOL implantation and basic corneal refractive surgery should be considered a vital component of the Ophthalmology resident surgical training process. We recommend including increased requirements within the curriculum, with the incorporation of formal didactics and wet lab exposure as the first step. Additionally, we propose that basic lens and corneal refractive surgical operative skill requirements should be expanded by the RRC/ACGME to better prepare residents in these deficiencies. Skills courses and computer simulation training could further enhance the training to help increase confidence in these techniques.
The responsibility to expand surgical education should be shared by individual residency programs and supplemented by national organizations, such as the American Academy of Ophthalmology (AAO), the American Society of Cataract and Refractive Surgeons (ASCRS), and the International Society of Refractive Surgery (ISRS).
There are some inherent limitations to this study. First, although there were 275 responses to this survey, there is a weakness in sampling methodology since this only represents a small percentage of total number of residents and young physicians. Secondly, the survey relied on self-reported data, and subject to recall bias.
This direct survey is the first reported publication to evaluate the quality of cataract surgery, IOL technology and refractive surgery education of young ophthalmologists during residency. This demonstrates that the minimum number of cataract surgeries set by the RRC/ACGME coincides well with overall resident satisfaction with exposure to phacoemulsification cataract extraction. The very low requirements for excimer laser surgery exposure also correlates with the overall dissatisfaction to the lack of such training in residency. The data presented in this study highlight a need for improved residency training in surgical astigmatism management, new technology IOL implantation, and basic corneal refractive surgery skills. With such improvements, graduates will likely feel more prepared for entering current anterior segment practice with its increasing emphasis on refractive and patient lifestyle outcomes.
Synopsis.
Although ophthalmology residency surgical training prepares young ophthalmologists in basic cataract surgery skills, a deficiency exists in the training of surgical astigmatism management, advanced IOL technology, and corneal refractive surgery.
Acknowledgments
Financial Support: Supported in part by Research to Prevent Blindness, Inc. New York, New York, and the National Institutes of Health Core Grant P30 EYO6360, Bethesda, Maryland.
Footnotes
Financial Disclosures: The authors have no financial interests or disclosures for any of the products or topics mentioned in this manuscript
References
- 1.Randleman JB, Srivastava SK, Aaron MM. Phacoemulsification with topical anesthesia performed by resident surgeons. J Cataract Refract Surg. 2004 Jan;30(1):149–54. doi: 10.1016/S0886-3350(03)00491-7. [DOI] [PubMed] [Google Scholar]
- 2.Wiggins MN, Warner DB. Resident physician operative times during cataract surgery. Ophthalmic Surg Lasers Imaging. 2010 Sep-Oct;41(5):518–22. doi: 10.3928/15428877-20100726-07. Epub 2010 Jul 29. [DOI] [PubMed] [Google Scholar]
- 3.Randleman JB, Wolfe JD, Woodward M, Lynn MJ, Cherwek DH, Srivastava SK. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007 Sep;125(9):1215–9. doi: 10.1001/archopht.125.9.1215. [DOI] [PubMed] [Google Scholar]
- 4.LeBoyer RM, Deutsch TA, Rubenstein JB. Results of resident-performed laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:771–5. doi: 10.1016/j.jcrs.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 5.Wagoner MD, Wickard JC, Wandling GR, Jr, Milder LC, Rauen MP, Kitzmann AS, Sutphin JE, Goins KM. Initial resident refractive surgical experience: outcomes of PRK and LASIK for myopia. J Refract Surg. 2011 Mar;27(3):181–8. doi: 10.3928/1081597X-20100521-02. Epub 2010 Jun 1. [DOI] [PubMed] [Google Scholar]
- 6.Surgical outcomes of photorefractive keratectomy and laser in situ keratomileusis by inexperienced surgeons. Yo C, Vroman C, Ma S, Chao L, McDonnell PJ. J Cataract Refract Surg. 2000 Apr;26(4):510–5. doi: 10.1016/s0886-3350(99)00468-x. [DOI] [PubMed] [Google Scholar]
- 7.Taravella MJ, Davidson R, Erlanger M, Guiton G, Gregory D. Characterizing the learning curve in phacoemulsification. J Cataract Refract Surg. 2011 Jun;37(6):1069–75. doi: 10.1016/j.jcrs.2010.12.054. [DOI] [PubMed] [Google Scholar]
- 8.Hosler MR, Scott IU, Kunselman AR, Wolford KR, Oltra EZ, Murray WB. Impact of Resident Participation in Cataract Surgery on Operative Time and Cost. Ophthalmology. 2011 Sep 15; doi: 10.1016/j.ophtha.2011.06.026. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.McDonnell PJ, Kirwan TJ, Brinton GS, Golnik KC, Melendez RF, Parke DW, 2nd, Renucci A, Smith JH, Smith RE. Perceptions of recent ophthalmology residency graduates regarding preparation for practice. Ophthalmology. 2007 Feb;114(2):387–91. doi: 10.1016/j.ophtha.2006.10.027. Epub 2006 Dec 20. [DOI] [PubMed] [Google Scholar]
- 10.Wiggins MN, Warner DB. Resident physician operative times during cataract surgery. Ophthalmic Surg Lasers Imaging. 2010 Sep-Oct;41(5):518–22. doi: 10.3928/15428877-20100726-07. Epub 2010 Jul 29. [DOI] [PubMed] [Google Scholar]
- 11.Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009 Mar;116(3):431–6. doi: 10.1016/j.ophtha.2008.10.028. Epub 2009 Jan 22. [DOI] [PubMed] [Google Scholar]
- 12.Unal M, Yücel I, Altin M. Pain induced by phacoemulsification performed by residents using topical anesthesia. Ophthalmic Surg Lasers Imaging. 2007 Sep-Oct;38(5):386–91. doi: 10.3928/15428877-20070901-05. [DOI] [PubMed] [Google Scholar]
- 13.Unal M, Yücel I, Sarici A, Artunay O, Devranoğlu K, Akar Y, Altin M. Phacoemulsification with topical anesthesia: Resident experience. J Cataract Refract Surg. 2006 Aug; doi: 10.1016/j.jcrs.2006.02.063. [DOI] [PubMed] [Google Scholar]
- 14.Oetting TA. Surgical competency in residents. Curr Opin Ophthalmol. 2009 Jan;20(1):56–60. doi: 10.1097/icu.0b013e328319914f. [DOI] [PubMed] [Google Scholar]
- 15.Rogers GM, Oetting TA, Lee AG, Grignon C, Greenlee E, Johnson AT, Beaver HA, Carter K. Impact of a structured surgical curriculum on ophthalmic resident cataract surgery complication rates. J Cataract Refract Surg. 2009 Nov;35(11):1956–60. doi: 10.1016/j.jcrs.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Henderson BA, Grimes KJ, Fintelmann RE, Oetting TA. J Cataract Refract Surg. Stepwise approach to establishing an ophthalmology wet laboratory. 2009 Jun;35(6):1121–8. doi: 10.1016/j.jcrs.2009.01.027. [DOI] [PubMed] [Google Scholar]
- 17.Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011 Oct;37(10):1756–61. doi: 10.1016/j.jcrs.2011.04.032. Epub 2011 Aug 15. [DOI] [PubMed] [Google Scholar]
- 18.Feudner EM, Engel C, Neuhann IM, Petermeier K, Bartz-Schmidt KU, Szurman P. Virtual reality training improves wet-lab performance of capsulorhexis: results of a randomized, controlled study. Graefes Arch Clin Exp Ophthalmol. 2009 Jul;247(7):955–63. doi: 10.1007/s00417-008-1029-7. Epub 2009 Jan 27. [DOI] [PubMed] [Google Scholar]
- 19.Lee AG, Greenlee E, Oetting TA, Beaver HA, Johnson AT, Boldt HC, Abramoff M, Olson R, Carter K. The Iowa ophthalmology wet laboratory curriculum for teaching and assessing cataract surgical competency. Ophthalmology. 2007 Jul;114(7):e21–6. doi: 10.1016/j.ophtha.2006.07.051. [DOI] [PubMed] [Google Scholar]
- 20.Ament CS, Henderson BA. Optimizing resident education in cataract surgery. Curr Opin Ophthalmol. 2011 Jan;22(1):64–7. doi: 10.1097/ICU.0b013e3283415040. [DOI] [PubMed] [Google Scholar]
- 21.Aaron MM, Aaberg TM. Ophthalmology resident training in refractive surgery. Am J Ophthalmol. 2001;131:241–3. doi: 10.1016/s0002-9394(00)00773-x. [DOI] [PubMed] [Google Scholar]
- 22.Kwon RO, Shah VA, Krishna R, Hausheer J. Resident laser in situ keratomileusis surgical training in United States residency programs. J Cataract Refract Surg. 2009 Sep;35(9):1629–32. doi: 10.1016/j.jcrs.2009.05.011. [DOI] [PubMed] [Google Scholar]
- **.Lee AG, Koch DD. The Baylor survey of Ophthalmology Residency graduates: rationale for reform in residency training. Ophthalmic Surg Lasers. 1998 Aug;29(8):649–57. [PubMed] [Google Scholar]


