Abstract
Vitreoretinal interface alterations leading to vitreopapillary and vitreomacular traction in a 29-year case of proliferative Eales’ disease is described for the first time. On fundus examination, an ellipsoid area of vitreomacular traction was noted temporal to the optic disc. A triangular-shaped infolding of the retina was observed superior to the fovea. Epiretinal membrane was seen temporal to the disc involving the macula. Imaging by spectral domain optical coherence tomography in the papillomacular bundle region revealed retinoschisis at the level of the outer nuclear layer and confirmed the presence of retinal infolding and epiretinal membrane in the macular area. Three-dimensional imaging documented vitreoretinal interface alterations exquisitely.
Background
Eales’ disease is an idiopathic obliterative vasculopathy that primarily affects the peripheral retina of young adult men.1 The predominant age of onset of symptoms is 20–30 years. The disease is rare in developed countries. However, it is commonly reported from the Indian subcontinent with an incidence of one in 200–250 ophthalmic patients.2 Retinal changes are characterised by periphlebitis, peripheral capillary non-perfusion and neovascularisation.3 4 Visual loss is characteristically caused by recurrent vitreous haemorrhage and its sequelae.5 The disease is categorised by inflammatory and proliferative stages.6
Macular involvement has been reported in Eales’ disease.7 However, vitreoretinal interface alterations leading to vitreopapillary and vitreomacular traction are reported for the first time.
Case presentation
The authors confirm adherence to the tenets of the Declaration of Helsinki. A written informed voluntary consent was taken. A 29-year-old man of Asian origin presented to the outpatient department of our tertiary care centre with complaints of gradually progressive painless diminution of vision in the left eye since 1 year. On examination, the vision in the right eye was 20/20 and in the left eye was counting finger close to face. Anterior segment examination of both the eyes was unremarkable. Stereoscopic slit lamp biomicroscopic examination of the fundus of both the eyes was done. The right eye revealed no abnormality. On fundus examination of the left eye, the patient was diagnosed as Eales’ disease stage 3A.6 The fundus showed extensive perivascular sheathing. A fibrous traction band was seen projecting anteriorly from the surface of the disc leading to tractional retinal detachment nasal to the disc. A well-defined ellipsoid area of traction was seen temporal to the disc, involving the macula. Pigmentary alterations were present on the macula. A triangular shaped infolding of the retina was observed superior to the fovea. The epiretinal membrane (ERM) was seen temporal to the disc involving the macula and demonstrated vitreomacular traction (figure 1). Spectral domain optical coherence tomography (SD-OCT) (Cirrus high definition OCT (Carl Zeiss Meditec Inc, California, USA)) over the disc and macula was performed. In the horizontal and vertical OCT scans, vitreoretinal surface alterations were discerned. The retinal layers were elevated in the papilomacular bundle region with retinoschisis occurring at the level of the outer nuclear layer. Over the macula, the retina was infolded on itself. A cleavage plane of the infolded retina corresponding to the dip seen over the internal limiting membrane (ILM) map was seen. ERM was seen over the surface of the retina. The retinal pigment epithelium was hyperplastic (figure 2). The internal limiting membrane-retinal pigment epithelium map showed regions of retinal elevation over the macula and the peripapillary region. Three-dimensional SD-OCT showed, vitreopapillary and vitreomacular traction. Retinal fold in the papillomacular bundle and macular area was appreciated (figure 3). The patient was not on any medication and had not undergone any surgical or laser intervention for the same. He did not show tuberculin skin test reactivity. Systemic disorders such as diabetes mellitus, tuberculosis, sickle cell haemoglobinopathy, blood dyscrasias, sarcoidosis and collagen vascular diseases were ruled out after proper history, examination and investigations (fasting and postprandial blood sugar, chest x-ray, sickle cell preparation, haemoglobin, haematocrit, total red and white blood cell count, differential count, erythrocyte sedimentation rate, serum ACE inhibition and antinuclear antibody, respectively). The patient was advised surgery, but did not opt for the same. The fundi remained stable during the 5 month observational follow-up.
Figure 1.
Fundus photograph of the left eye shows perivascular sheathing (solid arrow). A fibrous traction band is seen projecting anteriorly from the surface of the disc leading to tractional retinal detachment nasal to the disc. A triangular-shaped infolding of the retina is seen superior to the fovea (arrow). Epiretinal membrane is seen temporal to the disc involving the macula. A well-defined ellipsoid area of traction is appreciable temporal to the disc and involving the macula (arrow heads).
Figure 2.
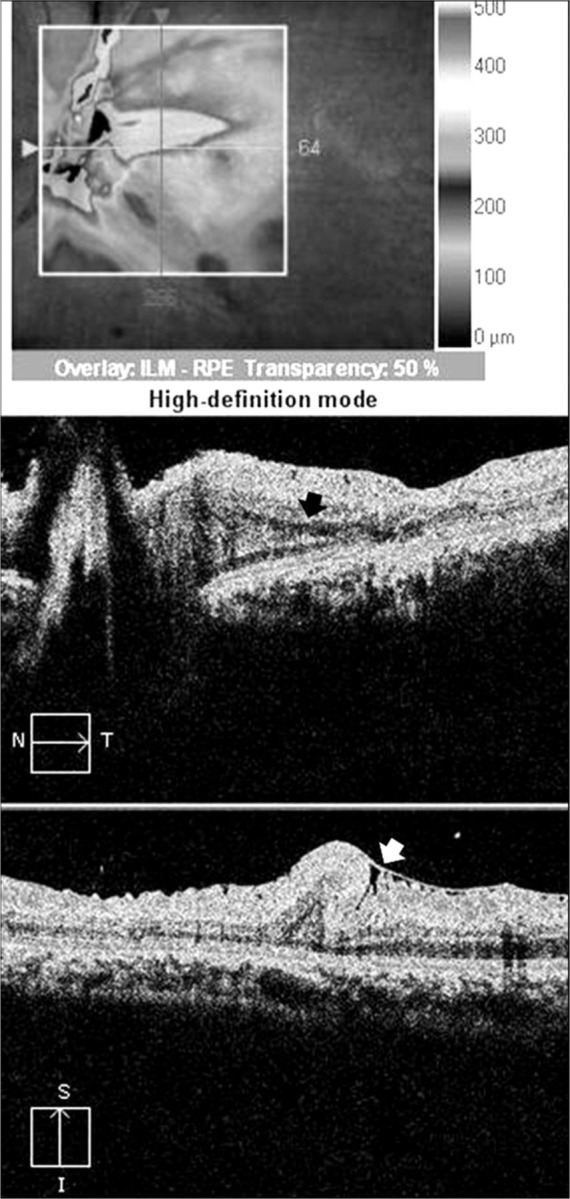
Spectral domain optical coherence tomography scans with overlay map show elevated retinal layers in the peripapillary region with retinoschisis (black arrow) occurring at the level of the outer nuclear layer. Over the macula, the retina is infolded on itself. Epiretinal membrane is seen over the surface of the retina (white arrow). The retinal pigment epithelium is hyperplastic.
Figure 3.
Three-dimentional optical coherence tomography shows vitreopapillary traction (solid arrow) due to residual fibrous proliferation (arrow head) and vitreomacular traction highlighted on the ILM (grey tone). Retinal fold in the papillomacular bundle area can be appreciated well (arrow).
Discussion
Eales’ disease is generally bilateral. However, unilateral cases are frequently seen. Macular involvement in Eales’ disease has been described by Saxena et al,7 in a large series. However, vitreoretinal surface alterations in Eales’ disease have not been reported. Vitreopapillary and vitreomacular tractions with ERM leading to vitreomaculopathy have been described in diabetic retinopathy.8–10 Their presence in Eales’ disease is reported for the first time. Anomalous posterior vitreous detachment (PVD) is known to cause vitreomacular and vitreopapillary traction which promotes optic disc and retinal neovascularisation.11 However, in this case no PVD was observed. Vitreopapillary adhesion may influence the vectors of force at the vitreoretinal interface causing a centrifugal tangential contraction which can result in idiopathic ERM.12–13 An ellipsoid area of vitremacular traction was seen temporal to the disc. The traction at the macula led to infolding of the retina. Peripapillary traction leading to retinoschisis in the papillimacular bundle area was noted on OCT but could not be discerned on stereoscopic biomicroscopic examination of the fundus. Vitreoschisis in Eales’ disease has been described by Badrinath et al14 Retinoschisis in Eales’ disease is reported for the first time.
Careful stereoscopic biomicroscopic fundus evaluation is necessary to look for alterations occurring at the vitreoretinal interface. SD-OCT helps in looking for subtle changes not visualised well on fundus examination as in this case, the retinoschisis. Three-dimensional SD-OCT is further useful in documenting these changes. Identification of such alterations can help in the planning of vitreoretinal surgery and prognosticating the visual outcome.
Learning points
Vitreopapillary and vitreomacular traction can occur in Eales’ disease in the absence of an anomalous posterior vitreous detachment.
Careful stereoscopic slit lamp biomicroscopic fundus evaluation is necessary for planning vitreoretinal surgery and assessing visual prognosis.
Spectral domain optical coherence tomography can help in identifying the subtle changes occurring at the vitreoretinal interface as well as in vivo retinal histology.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Gieser SC, Murphy RP. Eales’ disease. In: Ryan SJ. Retina Vol II. Medical retina. St. Louis: CV Mosby, 1994:1503–7. [Google Scholar]
- 2.Das T, Biswas J, Kumar A, et al. Eales’ disease . Indian J Ophthalmol 1994;42:3–18. [PubMed] [Google Scholar]
- 3.Atmaca LS, Idil A, Gunduz K. Visualization of retinal vasculitis in Eales disease. Ocul Immunol Inflammol 1993;1:41–4. [DOI] [PubMed] [Google Scholar]
- 4.Bali T, Saxena S, Kumar D, et al. Response time and efficacy of oral methotrexate pulsed therapy in idiopathic retinal periphlebitis. Eur J Ophthalmol 2005;15:374–8. [DOI] [PubMed] [Google Scholar]
- 5.Kumar D, Saxena RC, Saxena S. Vitreous haemorrhage in Eales’ disease. Afro-Asian J Ophthalmol 1995;13:109–12. [Google Scholar]
- 6.Saxena S, Kumar D. A new staging system for idiopathic retinal periphlebitis. Eur J Ophthalmol 2004;14:236–9. [DOI] [PubMed] [Google Scholar]
- 7.Saxena S, Kumar D. Macular involvement in Eales disease. Ann Ophthalmol 2000;32:98–100. [Google Scholar]
- 8.Kroll P, Wiegand W, Schmidt J. Vitreopapillary traction in proliferative diabetic vitreoretinopathy. Br J Ophthalmol 1999;83:261–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karatas M, Ramirez JA, Ophir A. Diabetic vitreopapillary traction and macular oedema. Eye 2005;19:676–82. [DOI] [PubMed] [Google Scholar]
- 10.Ophir A, Martinez MR. Epiretinal membranes and incomplete posterior vitreous detachment in diabetic macular edema, detected by spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2011;52:6414–20. [DOI] [PubMed] [Google Scholar]
- 11.Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol 2004;242:690–8. [DOI] [PubMed] [Google Scholar]
- 12.Sebag J. Vitreoschisis. Graefes Arch Clin ExpOphthalmol 2008;246:329–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang MY, Nguyen D, Hindoyan N, et al. Vitreo-papillary adhesion in macular hole and macular pucker. Retina 2009;29:644–50. [DOI] [PubMed] [Google Scholar]
- 14.Badrinath SS, Gopal L, Sharma T. Vitreoschisis in Eales’ disease: pathogenic role and significance in surgery. Retina 1999;19:51–4. [DOI] [PubMed] [Google Scholar]




