Abstract
The neuropeptide substance P (SP) exhibits cytokine-like properties and exerts different effects in autoimmune inflammation. Various immune cells express SP and its neurokinin-1 receptor (NK1R) isoforms. A role for SP has been demonstrated in a number of autoimmune conditions, including multiple sclerosis (MS). In this work, we studied the role of SP and NK1R in human immune cells with a focus on their relationship with IL-12/IL-23 family cytokines and the associated IFN-γ/IL-17. AIMS: (1) To determine the role of SP mediated effects on induction of various inflammatory cytokines in peripheral blood mononuclear cells (PBMC); (2) to investigate the expression of SP and its receptor in T cells and the effects of stimulation with IL-12 and IL-23. Quantitative real-time PCR, flow cytometry, ELISA, promoter studies on PBMC and primary T cells from healthy volunteers, and Jurkat cell line. Treatment with SP significantly increased the expression of IL-12/IL-23 subunit p40, IL-23 p19 and IL-12 p35 mRNA in human PBMC. Expression of NK1R and SP in T cells was upregulated by IL-23 but a trend was observed with IL-12. The IL-23 effect likely involves IL-17 production that additionally mediates IL-23 effects. Mutual interactions exist with SP enhancing the cytokines IL-23 and IL-12, and SP and NK1R expression being differentially but potentially synergistically regulated by these cytokines. These findings suggest a proinflammatory role for SP in autoimmune inflammation. We propose a model whereby immunocyte derived SP stimulates Th1 and Th17 autoreactive cells migrating to the central nervous system (CNS), enhances their crossing the blood brain barrier and perpetuates inflammation in the CNS by being released from damaged nerves and activating both resident glia and infiltrating immune cells. SP may be a therapeutic target in MS.
Electronic supplementary material
The online version of this article (doi:10.1007/s11481-015-9589-x) contains supplementary material, which is available to authorized users.
Keywords: Substance P, Neurokinin-1 receptor, Human, IL-12, IL-23, Tachykinins, Human, PBMC
Introduction
Substance P (SP) is an ubiquitously found 11-amino acid peptide with a number of biological functions. It belongs to the family of tachykinins, which also includes neurokinin A, neurokinin B, neuropeptide K, neuropeptide Y, and hemokinin-1. SP is generated through the enzymatic cleavage of pre-pro-tachykinin A, which is encoded by the TAC1 gene. Splice variants of TAC1 also generate neurokinin A and neuropeptide K. The role of SP in pain pathways and neurogenic inflammation has been well established, including effects of vasodilatation and plasma extravasation. With its effects on smooth muscle, SP is known to be involved in motility of different organ tracts as well as stimulation of glandular secretion and modulating autonomic reflexes.
SP originates from several cellular sources. It is released by peripheral nerve endings and central terminals of sensory neurons in the central nervous system (CNS). In addition, it is produced by a variety of cells of the immune system. This, and the presence of its receptor, the neurokinin-1 receptor (NK1R) on cells of the immune system, suggest a role for SP in immune responses. Immunomodulatory properties and its role in autoimmune inflammation have only recently been investigated in more detail. A role for SP has been demonstrated in neuroimmune and systemic autoimmune/inflammatory conditions, including multiple sclerosis (MS), rheumatoid arthritis and inflammatory bowel disease (Goode et al. 2000; Kostyk et al. 1989; Lotz et al. 1987; O’Connor et al. 2004; Weinstock 2014), as well as in infections and cancer.
NK1R is a widely expressed G-protein coupled receptor, which can be expressed as a full length receptor in neuronal and non-neuronal cells, and a recently studied truncated isoform (NK1R-T), expressed in monocytes and other peripheral cells (Douglas and Leeman 2011). There is evidence that the proportion of the full length and truncated receptor varies by cell type and in disease states, such as inflammation and cancer (Chernova et al. 2009; Douglas and Leeman 2011).
In this article we discuss the interactions of SP and NK1R with the IL-12/IL-23 family of inflammatory cytokines with emphasis on the role of these molecules in neuroinflammatory conditions, including MS and its animal model, experimental autoimmune encephalomyelitis (EAE).
SP and NK1R are involved in neuroimmune communication, being abundantly expressed in the nervous system and its sensory nerve projections into peripheral immune organs, and immune cells themselves (lymphocytes, cells of monocyte lineage, dendritic cells, eosinophils, mast cells etc.). SP is involved in both innate and adaptive immune responses. The functions of SP involve induction of cytokines (see below), activation of immune cells (Nio et al. 1993; Scicchitano et al. 1988), modulation of T helper phenotype commitment (Brogden et al. 2005; Cunin et al. 2011; Levite 1998), chemotaxis (Ahluwalia et al. 1998; Ruff et al. 1985; Schratzberger et al. 1997), expression of adhesion molecules and effects on the blood–brain barrier (Matis et al. 1990; Vishwanath and Mukherjee 1996). A number of these effects have been linked to NK1R dependent activation of NFκB.
The effects include stimulation of the production of IL-1, IL-6, IL-8, IL-10, TNF-α from monocytes and macrophages (Ho et al. 1996; Kincy-Cain and Bost 1997; Laurenzi et al. 1990; Lotz et al. 1988), and IL-1, IL-2, IFN-γ, IL-4, IL-6, TNF-α and IL-10 from T cells (Blum et al. 1993; Calvo et al. 1992; Delgado et al. 2003).
Induction of IL-12 by SP has been demonstrated in the murine immune system (Kincy-Cain and Bost 1997) but until now not in the human immune system. IL-23 induction by SP has been reported in human monocytes (Cunin et al. 2011). In murine models, IL-12 has been shown to induce SP precursor mRNA in macrophages via STAT4 pathway (Arsenescu et al. 2005) and NK1R expression by both IL-12 and IL-18 stimulation via NFκB in T cells (Weinstock et al. 2003). Recently, IL-12 and IL-23 have been found to induce SP synthesis in murine T cells and macrophages, which can be regulated by IL-10 and TGF-β respectively (Blum et al. 2008).
EAE is a widely used model of MS with which it shares pathological, immunological, neurobiological, and clinical similarities (‘tHart et al. 2011; Constantinescu et al. 2011).
IL-12-induced IFN-γ production is the hallmark of the Th1 immune responses, whereas IL-17 is the signature cytokine of the Th17 proinflammatory pathway. Of note, studies showing SP induction of IFN-γ suggest that direct stimulation of NK1R is sufficent and the process does not require IL-12 (Blum et al. 2003). Moreover, although IL-23 is still thought to be an important cytokine for the stimulation and maintenance of the Th17 pathway, in particular in the human immune system, studies have shown that TGF-β in a proinflammatory environment that includes IL-6 and possibly IL-1, is responsible for Th17 differentiation (Bettelli et al. 2006). Although some discrepancies are still unresolved (Jagessar et al. 2012; Sanvito et al. 2010), a great number of studies are congruent in indicating a role for both Th1 and Th17 cells in MS and EAE (Edwards et al. 2010).
Studies in EAE have shown suppression of the disease in NK1R knockout mice and amelioration of T cell transfer EAE by NK1R antagonist CP-96345 (Nessler et al. 2006; Reinke et al. 2006). Additionally, the role for SP in the pathogenesis of MS has been suggested by genome-wide linkage studies highlighting SP precursor protein encoding TAC1 gene as a possible susceptibility gene for MS (Cunningham et al. 2005; Vandenbroeck et al. 2002).
In this work, we investigate the reciprocal regulation of substance P and NK1R and the IL-12/23 family with their associated inflammatory cytokines in the human immune system. Our findings show many similarities with those seen in a murine immune system, with relvance to many inflammatory diseases. We offer a perspective of how these interactions place SP as an important mediator of neuroinflammatory disease.
Methods
Cell Preparations and Cultures
PBMC were isolated from whole blood by standard density gradient centrifugation. For T cell activation, PBMC were cultured for 72 h with 10 μg/ml phytohemagglutinin (PHA-P, Sigma-Aldrich) in 10 % FCS/RPMI media. After media change, cells were stimulated with 1000 U/ml IL-2 (PeproTech) at 37 °C for 24 h. The resulting cells “blasts” are typically >95 % CD3+.
CD4+ cells were magnetically isolated using the human CD4+ T cell Isolation Kit (Miltenyi Biotec, USA), following the manufacturer’s protocol. These cells were then transferred into a 24-well plate pre-coated overnight with 0.5 ml/well of a mixture of anti-CD3 (0.5 μg/ml) (BD Pharmingen) and anti-CD28 (2.5 μg/ml) (BD Pharmingen) in PBS. The coated wells were washed with 1 ml RPMI medium prior to CD4+ cells transfer (106 cells/well).
The Jurkat T cell line (kindly donated by Professor David Heery, School of Pharmacy, University of Nottingham, UK) was used for NK1R promoter-reporter assay.
Stimulation of Cell Cultures
PBMC 106/ml were stimulated for 24 and 48 h with 10−6–10−12 M SP (Sigma-Aldrich) with and without the presence of NK1R antagonist CP-96345 (Pfizer) 10−5–10−6 M, its inactive enantiomer CP-96344 (Pfizer) 10−5–10−6 M, anti-NK1R antibody (Chemicon International Inc) 1:500 or 1:1000, lipopolysaccharide (LPS, E. coli serotype 0111:B4, Sigma-Aldrich) 1 μg/ml. After stimulation, the supernatants were removed and stored at -80 °C for ELISA. Stimulations with cytokines were carried out at the following final concentrations: 10 ng/ml IL-12 (R&D Systems) with and without 2.5 μg/ml anti-IFN-γ antibody (PeproTech EC), 10 ng/ml IL-23 (R&D Systems) with and without 2.5 μg/ml anti-IL-17 antibody (PeproTech), 10 ng/ml IL-17 (PeproTech), 10 ng/ml IFN-γ (PeproTech) for 8 and 24 h for mRNA-level, and 24 and 48 h for protein-level expression.
Flow Cytometry
Flow cytometry was performed for protein level expression of NK1R in PHA-stimulated PBMC (T cell blasts). After overnight incubation, stimulated T cell blasts were transferred into FACS tubes and 20 μl EDTA 100 mM (Sigma-Aldrich) were added to each tube and incubated for 5 min at room temperature, the cells were then fixed using formaldehyde 4 % (1 ml/tube) and left for 5–10 min at room temperature prior to washing three times, each with 1 ml PBA (Phosphate Buffered Albumin, containing 0.5 % bovine serum albumin in phosphate buffered saline), stained with 2.5 μl of monoclonal surface antibodies (anti-CD3-ECD, clone UCHT1, Beckman Coulter; anti-CD8-PeCy7, clone SFCI21Thy2D3, Beckman Coulter; and anti-CD56-PE, clone HCD56, Biolegend, and isotype control-PE, clone P3.6.2.8.1, eBioscience) and incubated for 40 min in the dark at 4 °C. The cells were then washed once with PBA and twice, each with 1 ml perm/wash buffer (BD Biosciences), stained with 10 μl anti-NK1R-APC antibody (R&D Systems, Clone 694501) and its isotype control (mouse IgG3-APC, clone 133316, R&D Systems) and incubated in the dark at room temperature for 30 min. Cells were washed once with perm/wash buffer, fixed with 0.4 ml of 0.5 % formaldehyde and analysed.
Regarding CD4+ cells staining, 20 μl EDTA (100 mM) and 1 ml formaldehyde 4 % were added as above. The cells were washed three times with 1 ml perm/wash buffer and 10 μl anti-NK1R-APC antibody were added. The cells were incubated for 30 min in the dark at room temperature, washed once with 1 ml perm/wash buffer, and fixed with 0.4 ml formaldehyde 0.5 %. For flow cytometry experiments, FC500 (Beckman Coulter) flow cytometer and Weasel 3.1 software were used. For data presentation, GraphPad Prism 6.0 software was used. The quadrants were set in flow cytometry plots using single colour control tubes, fluorescence minus one (FMO) tubes, and isotype control tubes.
ELISA
Commercial kits were used for measuring concentrations of IL-1β (R&D Systems) and the different IL-12 and IL-23 subunits in stimulated PBMC culture supernatants, as well as SP in T blast supernatants. IL-12p40 (Diaclone), IL-12p70 (eBioscience) and IL-23 p19/p40 (eBioscience) kits were used following manufacturer’s instructions with assay sensitivities specified as follows: below 2.58 pg/ml for IL-1β, below 20 pg/ml for IL-12p40, below 15 pg/ml for IL-23 p19/p40 and 4 pg/ml for IL-12p70. For measuring SP in T blast supernatants, Parameter™ SP ELISA kit (R&D Systems) was used according to the instructions with 31.5 pg/ml as the mean minimum detectable concentration of SP.
Quantitative Real-Time Polymerase Chain Reaction (PCR)
Quantitative real-time reverse transcriptase PCR was used to assess mRNA abundance of IL-12, IL-23 subunits in PBMC on stimulation with SP, and mRNA abundance of SP precursor and NK1R isoforms in PHA/IL-2 T blasts that had been stimulated with IL-12, IL-23, IL-17, IFN-γ. Total-RNA was extracted by column extraction using RNeasy Miniprep Kit® (Qiagen) following the manufacturer’s instructions: the homogenization step was performed by needle homogenization. First strand cDNA synthesis was initiated from 0.5 μg total RNA using random primers (Promega, USA) and MMLV reverse transcriptase (Promega) using conditions specified by the manufacturer in a final volume of 25 μl. The following specific primer sequences were used for IL-23p19 sense: 5′ctccctgatagccctgtg3′, antisense: 5′gactgaggcttggaatct3′; for IL-12p40 sense: 5′ggagtaccctgacacctg3′, antisense: 5′agatgaccgtggctgagg3′; for IL-12p35 sense: 5′ccactccagacccaggaatg3′, antisense: 5′gacggccctcagcaggt3′; for NK1R-F (full length): sense 5′gaatgaggacagtgacgaac3′, antisense 5′ttgtggaacttgcagtagaac3′; for NK1R-T (truncated): sense 5′tcttcttcctcctgccctacatc3′; antisense 5′tggagagctcatggggttggatcct3′; for TAC1: sense 5′tcaatgggcaatgacaggta3′, antisense 5′tccgcagtagctgacacaac3′. As an internal standard, β2-microglobulin (β2MG) with the following primers was used: sense 5′ctccgtggccttagctgtg3′, antisense 5′tttggagtacgctggatagcct3′ (primers from MWG Biotech, Germany). For primer design Primer 3 software was employed. Real-time PCR reactions were carried out using the SYBR Green fluorescence method with SYBR Green Mastermix (Stratagene) as specified by the manufacturer. All real-time PCR reactions were carried out in triplicate on multiplex qPCR system Mx4000® (Stratagene) using default thermal cycling conditions. Dissociation curves were included routinely for each reaction for assessing product homogeneity. For quantitation of transcripts, the relative standard curve method, described by Applied Biosystems (AppliedBiosystems 1997), was used. For the set of standards, equal aliquots of undiluted cDNA from each sample were pooled together and serially diluted (neat, 1:2, 1:5, 1:10, 1:20). Using the standard curve, the comparative threshold cycle value was converted to nanograms of total RNA equivalent, used for first strand synthesis for both the target gene transcript and the housekeeping gene, β2MG. Subsequently, the values of individual sample mRNA abundance for the target gene were normalized with the corresponding values of β2MG. The reaction efficiency was optimal with template in 1:5 dilution and primer concentrations 10 pmol/μl; for TAC1 reaction the concentration of primers 2 pmol/μl and 1:5 template dilutions were used for optimal efficiency.
Transfection of Jurkat Cells With NK1R Promoter-Reporter Construct and Luciferase Reporter Assay
The vector for the NK1R promoter activation assay was prepared by transforming E coli DH5α –T1 competent cells (Invitrogen) with human NK1R gene promoter 1,837-bp fragment, cloned into luciferase expression vector pGL3-Basic (Promega) . For incorporation of the vector into Jurkat cells, 2 × 107 cells/400 μl ice-cold PBS were transferred into each electroporation cuvette (Invitrogen) and kept on ice for 10 mins. Subsequently, 3 μg prepared NK1R promoter-reporter plasmid (containing Photinus pyralis luciferase) and 0.3 μg Renilla reniformis luciferase reporter vector (Promega) as an incorporation control were added per cuvette and pulsed on Gene Pulser X cell™ (Biorad) with 250 V and 950 μF. After electroporation, cells were kept in 10 % FCS/RPMI overnight at 37 °C, 5 % CO2. Following stimulation of transfected cells with cytokines as above for 24 h, cells were washed with PBS and passively lysed according to the Dual-Luciferase Reporter Assay protocol (Promega), whilst kept on a shaker for 15 min. The lucifearase activities of each lysate were sequentially read on TD-20/20 single-sample luminometer (Turner Designs) by adding initiation/stop reagents (Promega) per protocol. Background luminescence of non-transfected control was subtracted from individual sample values and ratios of Photinus/Renilla luciferase signals were calculated.
Statistical Analysis
Data were analysed using nonparametric tests: Friedman test for comparisons of means of ordinal data, or Wilcoxon test for continuous variables. SPSS 16.0 software was employed for analysis. Differences were considered statistically significant when p was ≤0.05.
Results
Protein-Level Expression of IL-1β and IL-12p40 in PBMC Stimulated with SP
PBMC (106/ml) were stimulated with SP 10−6, 10−9 and 10−12 M, and IL-1β and IL-12p40 were measured by ELISA after 36–48 h. SP alone was unable to induce detectable IL-1β, unless co-stimulation with bacterial lipopolysaccharide (LPS) was used (data not shown). SP 10−6 M enhanced IL-12p40 from 53 (±36) pg/ml to 135 (±2) pg/ml (p = 0.02). Lower concentrations of SP failed to induce IL-12p40 in the absence of co-stimulation with LPS (data not shown). Because the amounts of IL-12p40 are likely to be too low to correspond to detectable levels of IL-12p70 or IL-23 protein by ELISA, we measured the mRNA expression of the IL-12 family cytokines.
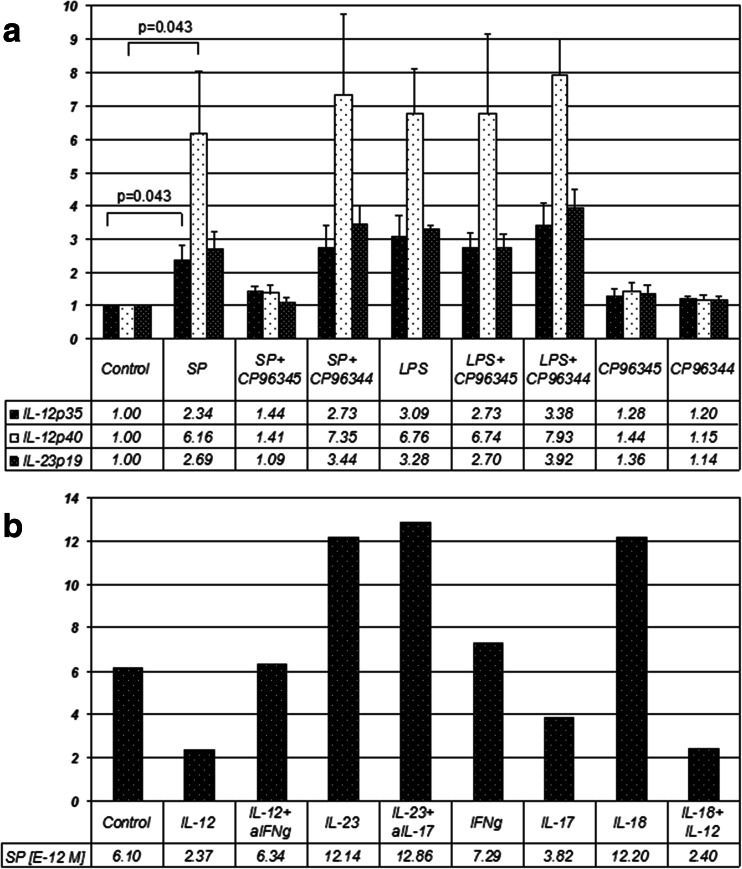
mRNA-Level Expression of IL-12 and IL-23 Subunits in PBMC on Stimulation with SP
To assess IL-12 and IL-23 induction by SP in PBMC, experiments with a 24-h induction of the IL-12/23p40, IL-12p35 and IL-23p19 subunit mRNA were done on 5 healthy volunteers. The expression of the three IL-12 and IL-23 subunits showed a similar response to stimulation with SP and suppression by CP-96345 (specific NK1R antagonist), but not by CP-96344 (control with no antagonist properties). SP strongly upregulated the expression of the subunits to a degree similar to LPS (Fig. 1a). The induction of the p40 subunit by SP was greatest with a 6.2-fold increase (p = 0.043), followed by p19 and p35 induction with a 2.7-fold (p = 0.068) and 2.3-fold (p = 0.043) increase in their expression respectively.
Fig. 1.
a Quantitative PCR results showing IL-12p35, IL-12/23p40 and IL-23p19 mRNA abundance in PBMCs in response to 24 h incubation with different stimuli. The values represent arbitrary units after normalization with corresponding values of β2MG as an internal standard. Each bar represents averages of 5 different healthy donors, error bars indicate SEM; b representative results from one healthy donor showing molar concentrations of SP (times 10−12 M) in cell culture supernatants on ELISA, following a 24 h stimulation of T blasts with different stimuli. The concentrations are converted from mass concentrations (pg/ml) given on ELISA
The product homogeneity and size for each of the conditions was confirmed on agarose gel electrophoresis with a product size of 131 bp for IL-12/23p40, 62 bp for IL-12p35, 109 bp for IL-23p19 and 148 bp for β2MG.
Expression of NK1R and SP in Lymphocyte Populations and Effects of IL-12 and IL-23
The expression of the NK1R receptor on subgroups of human immune cells is not well known. We determined this expression by flow cytometry using a directly conjugated antibody. The percentages of NK1R+ cells in PHA-stimulated T cells (“blasts”), and subgroups of blasts based on expression of cell surface markers CD3, CD8, and CD56, unstimulated or stimulated with IL-12 or IL-23 for 24 h, and gated for CD3 (CD3-PC7, NK1R-PE) can be found in supplemental Table 1 online. In addition, the percentages of NK1R+ cells among the magnetically separated CD4+ T cells grown on anti-CD3/anti-CD28-coated plates and stimulated as above are shown in the table.
Both IL-12 and IL-23 appeared to modestly (not statistically significantly) increase NK1R in PHA-stimulated T cells (“blasts”), and subgroups expressing CD3, CD8, and CD56 (Table 1 and Supplemental Figure 1 Online). Similar slight but not statistically significant trends towards increased NK1R expression were observed with 24 and 48 h stimulation with IL-12 plus IL-18, IL-18, IL-23, IL-17 and IFN-γ (not shown).
For SP peptide induction, two separate ELISAs were run on supernatants of stimulated T cells from 5 control subjects (Fig. 1b). Peptide level SP expression showed a great deal of variability between subjects. None of the stimulation conditions studied, i.e. IL-12, IL-12 plus anti-IFN-γ, IL-23, IL-23 plus anti-IL-17, IL-18, or IL-12 plus IL-18 showed effects that were statistically significant at the protein level.
mRNA Level Induction of NK1R and SP in T Cells
The results shown so far, regarding NK1R, refer to the full-length transcript. We have examined the NK1R isoform expression in T cell blasts with similar expression of the truncated (NK1R-T) versus full-length NK1R (NK1R-F; “NK1R” in this article refers to NK1R-F) isoform in unstimulated T cell blasts (ratio of 1.13; 53 % versus 47 %, respectively, p = 0.95).
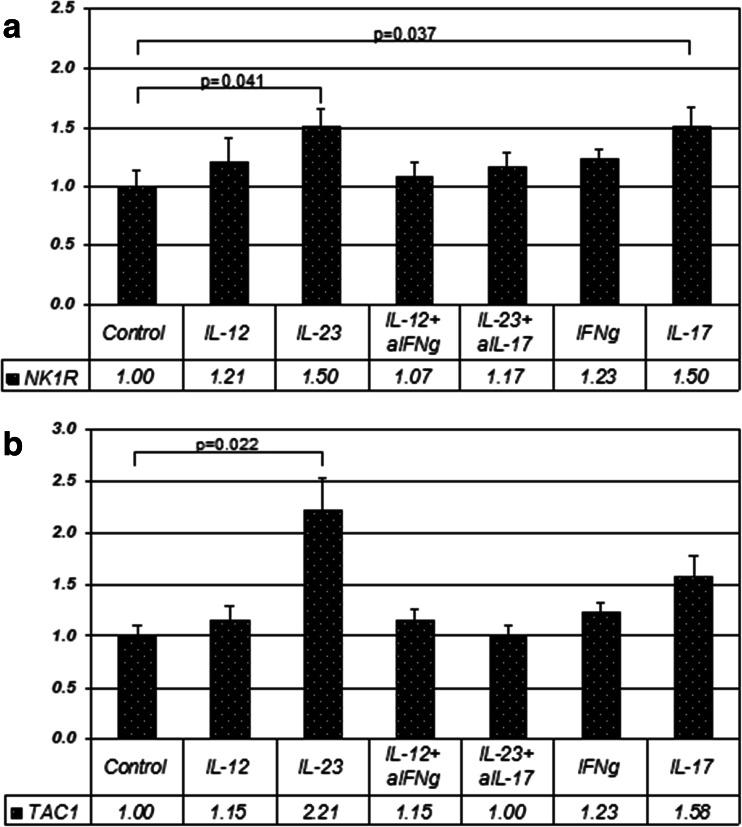
The effects of different cytokine stimuli on SP precursor and NK1R mRNA level expression were studied in PHA/IL-2-stimulated T cell blasts from 10 healthy volunteers. IL-23 significantly upregulated both NK1R (p = 0.041) and TAC1 transcripts (p = 0.022) (Fig. 2a and b). There was a trend to upregulation of TAC1 and NK1R by IL-12 (Fig. 2). Therefore, we restricted the NK1R-T analysis to the IL-23 stimulation. We observed a preferential induction of NK1R-T upon stimulation with IL-23 compared to NK1R-F (ratio 4:1; p = 0.007).
Fig. 2.
a Quantitative PCR was used to assess mRNA-level expression of NK1R relative to internal standard β2MG. Each bar represents an average of 10 stimulation assays on T cell blasts from 10 different healthy donors +/- SEM. The results of individual assays were expressed in arbitrary units of mRNA abundance, normalised with the corresponding values of β2MG; b mRNA-abundance of TAC1 relative to internal standard β2MG: mean ratios of stimulation assays on T blasts from 10 different healthy donors +/- SEM
NK1R (p = 0.037) but not TAC1 (p = 0.203) expression was also significantly upregulated by IL-17A (here referred to as IL-17). Anti-IL-17 abolished the effects of IL-23 in inducing TAC1 (p = 0.041), but not NK1R (p = 0.262) (Fig. 2). On the other hand, anti-IFN-γ did not block IL-12 effects in these experiments.
The above effects were studied over different stimulation periods as IL-12 and IL-23 responses may prevail at different stages of inflammation (Thakker et al. 2007). Stimulation for 8 and 24 h was used, as possible induction of secondary cytokines to IL-12 and IL-23 stimuli may take time to initiate, however, no differences were found in T cell blasts between 8 and 24 h. The results from a 4 h-stimulation as used by Weinstock et al. (Weinstock et al. 2003) and Arsenescu et al. (Arsenescu et al. 2005) were also not significantly different from the effects at 8 and 24 h.
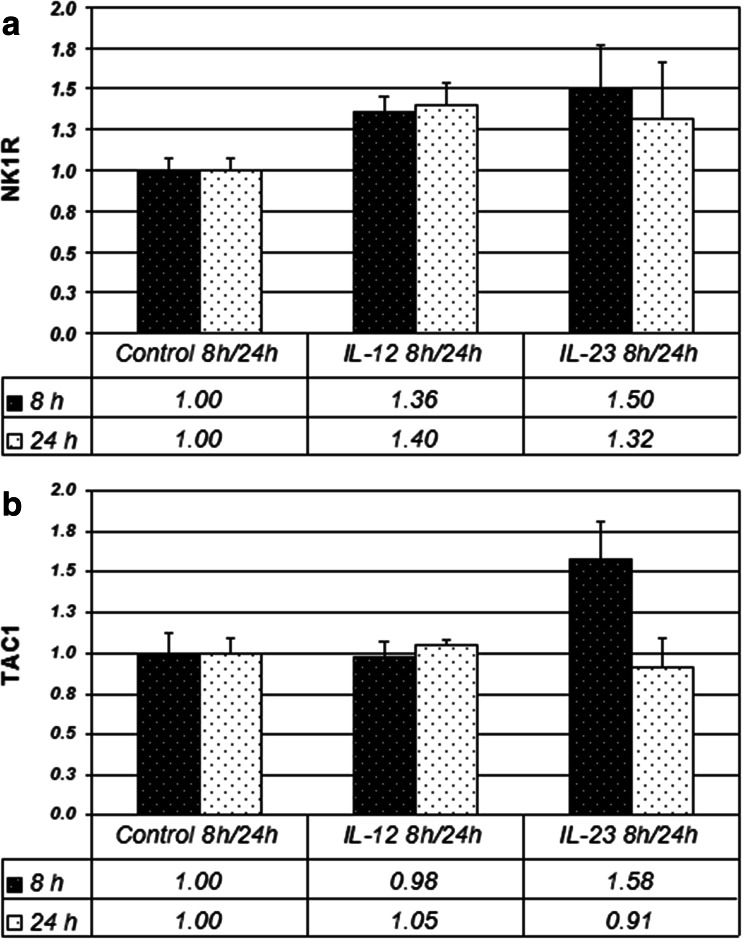
However, in the experiments done on CD4+ cells, a slightly greater tendency for NK1R induction by IL-12 was seen at 24 h as compared to 8 h, and in SP induction by IL-23 at 8 h as opposed to 24 h (Fig. 3). With the 8 and 24 h sets combined, NK1R induction by IL-23 in CD4+ cells was significant (p = 0.043), and induction by IL-12 showed only a trend (p = 0.063).
Fig. 3.
NK1R and TAC1 mRNA abundance in CD4+ cells following 8 and 24 h stimulation (10 ng/ml IL-12 or 10 ng/ml IL-23), normalized with β2MG as internal standard. The values represent mean ratios of 4 healthy donors +/- SEM
NK1R Promoter Construct Activation in Jurkat Cells
IL-23 appears to be a potent inducer of the NK1R promoter region with an average 6-fold increase in the reporter signal ratio compared to the unstimulated cells (Supplemental Figure 2 online). In both of these experiments, anti-IL-17 in IL-23 stimulated samples showed strong reduction of NK1R expression, compared to the IL-23 stimulus alone. IL-12 and IFN-γ showed little activation in these assays. IL-17, IL-18 and the combination of IL-12 and IL-18 showed moderate effects with 2.1, 2.3 and 2.8-fold average increase from the baseline respectively.
Discussion
While evidence exists for a potential role of SP in experimental and human autoimmune neuroinflammatory disease, and the role of the IL-12 family and related inflammatory cytokines is convincing, little is known to date about the induction of the IL-12 family cytokines by SP in human immune cells or about the effects of proinflammatory cytokines on the expression of NK1R in human immune cells (Weinstock 2014). In animal models, SP induced or stimulated Th1 type and Th17 immune responses (Beinborn et al. 2010), or inhibited anti-inflammatory cytokines as recently shown in murine dendritic cells (Janelsins et al. 2013).
In our study on human PBMC, a small degree of induction of IL-12p40 by SP was observed at the protein level. The small amounts of IL-12p40 suggested that sensitivity of the ELISA would be too low to detect the heterodimeric cytokines IL-12p70 and IL-23. The sensitivity of the Cytometric Bead Array (CBA), lower than the individual ELISA, had been also tested before ELISA measurements and found insufficient to detect the heterodimeric cytokines in our series (data not shown). Small effects of SP on IL-12 secretion are consistent with the published report (Janelsins et al. 2013).
When studying mRNA-level expression of the individual subunits, induction of all subunits is detectable. The highest values were seen with p40, consistent with the role of p40 as part of both IL-12 and IL-23. The common p40 may also be found in free monomer and in homodimers form in the mouse immune system. The mRNA abundance of both IL-12p35 and IL-23p19 was lower than that of p40, whereas the abundance of p19 was slightly higher than that of p35. The results suggest potentially distinct molecular mechanisms for IL-12 and IL-23 induction by SP, possibly involving distinct signalling pathways and downstream regulatory factors (Goodridge et al. 2003) at translational level or post-translational processing level as known for p35 (Murphy et al. 2000).
IL-12 induction by SP has been previously shown at mRNA level in murine macrophages (Kincy-Cain and Bost 1997). In that study, SP agonist concentrations as low as 10−9 M were bioactive, while 10−6 M had an effect in our study. In the study by Kincy-Cain, both IL-12p40 and IL-12p35 mRNA were potently induced; however, an increase in IL-12p70 expression was not detected. At the protein level at 24 h, IL-12p40 was induced, however, no detectable secretion of p70 occurred (Kincy-Cain and Bost 1997). We have not tested p70 in our study. Additive effects of SP on LPS in IL-12 induction were observed as were also seen in our experiments on PBMC.
IL-23 upregulates both NK1R and SP precursor mRNA and appears to be a stronger stimulus than IL-12 in human T cells. Whereas IL-12 can act on both naïve and activated cells, mainly activated cells are considered responsive to IL-23 (Parham et al. 2002).
In protein-level experiments, SP did not show consistent induction by the cytokines used. However, too much significance cannot be put on detected SP concentrations in cell culture supernatants as SP is quickly inactivated in aqueous solutions near physiological pH. The discrepancies between the protein and mRNA level induction will be discussed further below.
There was more pronounced inter-individual variability in TAC1 than in NK1R expression. This is expected as there are more factors known in TAC1 transcriptional and post-transcriptional regulation, providing a source for variation. These factors include transcriptional silencers repressing TAC1 transcription in non-neuronal cells (Greco et al. 2007). Within exon 1 in TAC1 promoter region, adjacent to NFκB site, two RE-1 silencer of transcription (REST) binding sites have been identified (Greco et al. 2007). Additionally, RNA-binding proteins and microRNAs regulate SP synthesis (Greco and Rameshwar 2007; Murthy et al. 2008). Although TAC1 mRNA is found ubiquitously in human non-neuronal tissues (Pinto et al. 2004), some studies suggest the importance of preconditioning non-neuronal cells with inflammatory stimuli for TAC1 expression. For example, IL-1α has been shown to induce TAC1 and particularly SP translation in non-neuronal cells (Greco and Rameshwar 2007).
Interestingly, we show that IL-23 stimulation increases the proportion of NK1R-T transcript in T cells. This truncated receptor has been implicated in the mechanisms whereby chronic inflammation transits to malignancy, a mechanism in which the IL-23/IL-17 pathways seems to play a role (Chernova et al. 2009).
Both NK1R and the TAC1 promoter regions have NFκB binding sites (Simeonidis et al. 2003; Takahashi et al. 1992). Here we have shown that NK1R promoter is activated by IL-23 and, as suggested by anti-IL-17 blocking effects, also by IL-17. Both IL-23 and IL-17 are known to signal via NFκB, consistent with our findings. Additionally, IL-18 showed similar moderate effects as IL-17 on the promoter level. In the work by Weinstock and colleagues (Weinstock et al. 2003) and Arsenescu and colleagues (Arsenescu et al. 2005), NK1R expression was induced by IL-12 and IL-18 in murine T cells via NFκB, whereas SP induction in murine macrophages was responsive only to IL-12 via STAT4. In our study, the effects of IL-18 and co-stimulation of IL-12 and IL-18, activating NK1R promoter, were less than the effects of IL-23. IL-12 alone showed no activation of NFκB-containing NK1R promoter, and it is known to act via STAT4. SP synthesis has been previously shown to be STAT4 independent (Blum et al. 2008).
IL-12 has previously been shown to induce SP which can mediate IFN-γ production, potentiating IL-12 effects in murine cells (Blum et al. 1993, 2001). Thus, SP has been so far suggested to be part of the Th1 pathway. In a more recent study, IL-12 was shown to induce SP in murine T cells, whereas IL-23 induced SP in macrophages (Blum et al. 2008). In our study, we also show evidence for SP pro-inflammatory effects on IL-23 and IL-17 pathways in humans, and a prominent effect of IL-17A and IL-23 on NK1R. Although less prominent, the effects of IL-12/IFN-γ and their interaction with SP and NK1R seem to follow the same directions as those seen in the murine immune system and to indicate a synergistic effect to the IL-23/IL-17 cytokines. In the stimulation of NK1R for induction of IFN-γ, IL-12 may be in part redundant, as it has been shown that NK1R ligation by SP directly induces IFN-γ.
The role of SP can be best summarized as of a pleiotropic immune regulator. SP signalling involves activation of NFκB, which underlies the regulation of various inflammatory genes, explaining SP effects on chemotaxis and other inflammatory mechanisms. One of the important mechanisms is SP participation in regulating cytokine pathways.
There are important proinflammatory cytokines such as IL-6 that may be even more important for the development of Th17 responses than IL-23. It is known that SP induces IL-6 (Blum et al. 1993; Calvo et al. 1992; Delgado et al. 2003). Our preliminary multiple cytokine assays performed by cytometric bead arrays (not shown) showed little or no induction of IL-6 by SP in PHA-stimulated PBMC. This paper focused primarily on the IL-12 family of heterodimeric cytokines, in particular since some of the IL-12-SP regulation reports preceded the discovery of IL-23.
SP modulation of immune activities is characterized by mutual regulation. As SP regulates a multitude of cytokines and its pathway is also regulated by inflammatory activity, the reciprocal interactions between SP and its receptor and the IL-12/IL-23 cytokines are unlikely to be specific to this family of cytokines but more likely to be part of a wider interactive network. Preconditioning of cells may be important for optimal SP effects, and similarly, priming of cells with SP can enhance cytokine effects. Protein-level effects largely depend on these multiple stimulatory conditions which are likely to be present and undergo dynamic changes in vivo. In particular in the context of inflammation, multiple inflammatory signals may synergise to produce a powerful inflammatory effect. The positive feedback loop between SP and proinflammatory cytokines may be essential for the augmentation of the inflammatory response and various sites. In addition, this interaction may play a role not only in augmenting, but also in maintaining inflammation, leading to a chronic inflammatory state, where recent evidence suggest the truncated NK1R (NK1R-T) may play a role.
Role of SP and its Interaction With IL-12/IL-23 and Related Cytokines in Autoimmune Neuroinflammation
As pointed out in a recent review on SP (Weinstock 2014), the immunoregulatory effects of SP are wide, and this can mean different or even opposite effects in different infections or inflammatory diseases: a protective role in some and a detrimental role in others. Even in conditions with similar etiologies, the regulation of and by SP and NK1R can be different. In inflammatory bowel disease, for example, there is initial strong activation of innate immune responses, and SP and NK1R are involved in this process. Thus blocking them could be of benefit.
MS is an autoimmune disease mediated predominantly by T cells (of Th1, Th17, and GM-CSF producing variety) (Constantinescu and Gran 2014). Both innate and adaptive immune responses play an essential role in MS (Podda et al. 2013)..
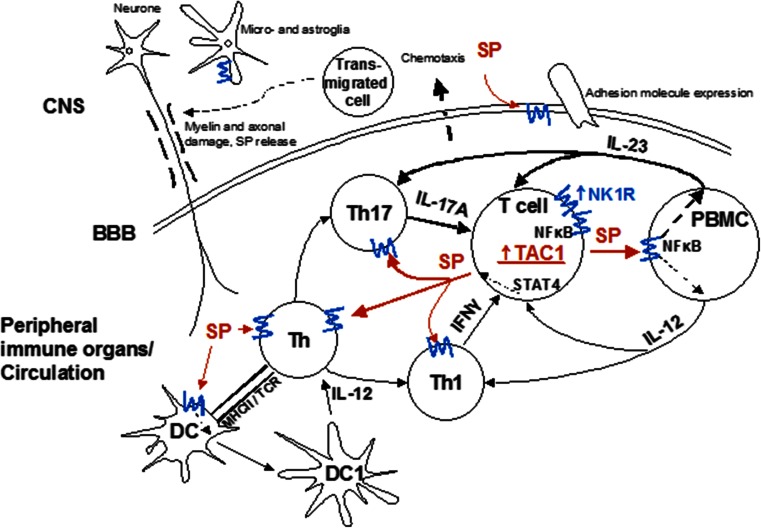
Where can the interaction of SP and NK1R with inflammatory cytokines investigated here occur in the autoimmune neuroinflammation of MS? In the prevailing model, autoreactive T cells become activated in the periphery through a variety of stimuli. SP plays an important role at this level, by enhancing proinflammatory cytokine production by these T cells, which can themselves produce more SP, up-regulate NK1R, and stimulate antigen presenting cells to produce further T cell stimulatory cytokines. This leads to an up-regulation of Th17 and Th1 responses, and enhanced penetration of the blood brain barrier (through up-regulation of NK1R and adhesion molecules on endothelial cells, among other mechanisms). In the CNS, SP stimulating cytokines, produced by infiltrating T cells and monocytes, and SP itself further stimulate both CNS-intrinsic cells with immune functions such as microglia and astrocytes. Consistent with this, SP-immunoreactive astrocytes are found in MS lesions (Kostyk et al. 1989), and CNS astrocyes and microglia express both IL-12 and IL-23 (Constantinescu et al. 2005). These processes facilitate perpetuation of inflammation, and a chronically activated microglia, as shown in progressive stages of MS (Lassmann et al. 2012) (Fig. 4).
Fig. 4.
Schematic diagram illustrating substance P (SP) and cytokine interactions in autoimmune demyelinating disease (e.g. MS). For clarity, only the main effects on pro-inflammatory Th17 and Th1 pathways have been depicted with thicker arrows representing stronger responses suggested by our study. Blue lines indicate NK1R. SP effects are shown in red. CNS central nervous system; BBB blood–brain barrier; DC dendritic cell; PBMC peripheral blood mononuclear cell; MHCII major histocompatibility complex II; TCR T cell receptor
A recently discovered mechanism may shed light on the complex role of TGF-β, which, in an inflammatory environment, induces Th17 responses. TGF-β reduces the otherwise rapid internalization of NK1R, not only increasing its availability to SP generated in CNS inflammation, with subsequent enhancement of IFN-γ and IL-17 production, but also leading to further Th17 differentiation of naive T cells (Bettelli et al. 2006).
The above proposed model indicates that blocking SP and its receptor can have a beneficial effect in autoimmune inflammation of the CNS such as occurs in MS, and that the effect may persist in the chronic stages of the condition. In the well-established MS model, EAE, the genetic absence of NK1R or its suppression using a synthetic antagonist was beneficial in the chronic stages of the disease (Reinke et al. 2006). In another study, a different antagonist also had therapeutic effects (Nessler et al. 2006). Notably, suppression of IFN-γ and of adhesion molecules were associated with the beneficial effects.
Given the similarity of the results presented here with those from the murine experiments, we conclude that SP, in part through its interaction with proinflammatory cytokines of the IL-12/IL-23, contributes to the development and perpetuation of autoimmune inflammation in the CNS, and it is a strong candidate as a therapeutic target in MS.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Expression of NK1R in various subsets of PBMCs from healthy human volunteers (n=3). The results are given as means and SEM of the percentage of cells expressing NK1R. (DOCX 13 kb)
NK1R expression in: PHA/IL-2 stimulated PBMCs (“blasts”) (Histograms A-H) and magnetically isolated CD4+ lymphocytes (Histogram I). Cells Gating: (A), non-gated; (B), CD56+ cells; (C), CD3+CD8- lymphocytes; (D), CD3+CD8+CD56-lymphocytes; (E), CD3-CD56+ cells; (F), CD3+CD56+ lymphocytes; (G), CD3+ lymphocytes; (H), CD8+ lymphocytes; (I), Lymphocytes. Colour legend: Black: Unstimulated cells; Red: IL-12-stimulated; Blue: IL-23-stimulated; Pink: Isotype control-bound cells. NK1R-APC: Allophycocyanin-conjugated mouse monoclonal anti-human NK1R (GIF 299 kb)
(TIFF 320 kb)
Dual-luciferase reporter assay with activation of NK1R promoter-reporter construct in Jurkat cells. The results represent mean ratios of Photinus/Renilla luminescence of two experiments after 24 h stimulation with different conditions. (GIF 104 kb)
(TIFF 36 kb)
Acknowledgments
We thank Professor Susan Leeman for helpful and inspiring discussions. This study was supported in part by the MS Society of Great Britain and Northern Ireland to CSC, and the NIH grant NIDDK R01 DK047343 to CP.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Ahluwalia A, De Felipe C, O’Brien J, Hunt SP, Perretti M. Impaired IL-1beta-induced neutrophil accumulation in tachykinin NK1 receptor knockout mice. Br J Pharmacol. 1998;124:1013–1015. doi: 10.1038/sj.bjp.0701978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AppliedBiosystems . User bulletin #2 ABI PRISM 7700 sequence detection system. Foster City: Applied Biosystems; 1997. [Google Scholar]
- Arsenescu R, Blum AM, Metwali A, Elliott DE, Weinstock JV. IL-12 induction of mRNA encoding substance P in murine macrophages from the spleen and sites of inflammation. J Immunol. 2005;174:3906–3911. doi: 10.4049/jimmunol.174.7.3906. [DOI] [PubMed] [Google Scholar]
- Beinborn M, et al. TGF-beta regulates T-cell neurokinin-1 receptor internalization and function. Proc Natl Acad Sci U S A. 2010;107:4293–4298. doi: 10.1073/pnas.0905877107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettelli E, et al. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- Blum AM, Metwali A, Cook G, Mathew RC, Elliott D, Weinstock JV. Substance P modulates antigen-induced, IFN-gamma production in murine Schistosomiasis mansoni. J Immunol. 1993;151:225–233. [PubMed] [Google Scholar]
- Blum AM, Metwali A, Crawford C, Li J, Qadir K, Elliott DE, Weinstock JV. Interleukin 12 and antigen independently induce substance P receptor expression in T cells in murine schistosomiasis mansoni. FASEB J. 2001;15:950–957. doi: 10.1096/fj.00-0379. [DOI] [PubMed] [Google Scholar]
- Blum A, Metwali A, Elliott D, Weinstock J. T cell substance P receptor governs antigen-elicited IFN-gamma production. Am J Physiol Gastrointest Liver Physiol. 2003;284:G197–G204. doi: 10.1152/ajpgi.00271.2002. [DOI] [PubMed] [Google Scholar]
- Blum A, Setiawan T, Hang L, Stoyanoff K, Weinstock JV. Interleukin-12 (IL-12) and IL-23 induction of substance P synthesis in murine T cells and macrophages is subject to IL-10 and transforming growth factor {beta} regulation. Infect Immun. 2008;76:3651–3656. doi: 10.1128/IAI.00358-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brogden K, Guthmiller J, Salzet M, Zasloff M. The nervous system and innate immunity: the neuropeptide connection. Nat Immunol. 2005;6:558–564. doi: 10.1038/ni1209. [DOI] [PubMed] [Google Scholar]
- Calvo CF, Chavanel G, Senik A. Substance P enhances IL-2 expression in activated human T cells. J Immunol. 1992;148:3498–3504. [PubMed] [Google Scholar]
- Chernova I, et al. Substance P (SP) enhances CCL5-induced chemotaxis and intracellular signaling in human monocytes, which express the truncated neurokinin-1 receptor (NK1R) J Leukoc Biol. 2009;85:154–164. doi: 10.1189/jlb.0408260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantinescu C, Gran B. The essential role of T cells in multiple sclerosis: a reappraisal. Biomed J. 2014;37:34–40. doi: 10.4103/2319-4170.128746. [DOI] [PubMed] [Google Scholar]
- Constantinescu C, et al. Astrocytes as antigen-presenting cells: expression of IL-12/IL-23. J Neurochem. 2005;95:331–340. doi: 10.1111/j.1471-4159.2005.03368.x. [DOI] [PubMed] [Google Scholar]
- Constantinescu C, Farooqi N, O’Brien K, Gran B. Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS) Br J Pharmacol. 2011;164:1079–1106. doi: 10.1111/j.1476-5381.2011.01302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunin P, et al. The tachykinins substance P and hemokinin-1 favor the generation of human memory Th17 cells by inducing IL-1beta, IL-23, and TNF-like 1A expression by monocytes. J Immunol. 2011;186:4175–4182. doi: 10.4049/jimmunol.1002535. [DOI] [PubMed] [Google Scholar]
- Cunningham S, et al. Haplotype analysis of the preprotachykinin-1 (TAC1) gene in multiple sclerosis. Genes Immun. 2005;6:265–270. doi: 10.1038/sj.gene.6364175. [DOI] [PubMed] [Google Scholar]
- Delgado AV, McManus AT, Chambers JP. Production of tumor necrosis factor-alpha, interleukin 1-beta, interleukin 2, and interleukin 6 by rat leukocyte subpopulations after exposure to substance P. Neuropeptides. 2003;37:355–361. doi: 10.1016/j.npep.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Douglas S, Leeman S. Neurokinin-1 receptor: functional significance in the immune system in reference to selected infections and inflammation. Ann N Y Acad Sci. 2011;1217:83–95. doi: 10.1111/j.1749-6632.2010.05826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards L, Robins R, Constantinescu C. Th17/Th1 phenotype in demyelinating disease. Cytokine. 2010;50:19–23. doi: 10.1016/j.cyto.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Goode T, et al. Neurokinin-1 receptor expression in inflammatory bowel disease: molecular quantitation and localisation. Gut. 2000;47:387–396. doi: 10.1136/gut.47.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodridge HS, Harnett W, Liew FY, Harnett MM. Differential regulation of interleukin-12 p40 and p35 induction via Erk mitogen-activated protein kinase-dependent and -independent mechanisms and the implications for bioactive IL-12 and IL-23 responses. Immunology. 2003;109:415–425. doi: 10.1046/j.1365-2567.2003.01689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greco SJ, Rameshwar P. Enhancing effect of IL-1alpha on neurogenesis from adult human mesenchymal stem cells: implication for inflammatory mediators in regenerative medicine. J Immunol. 2007;179:3342–3350. doi: 10.4049/jimmunol.179.5.3342. [DOI] [PubMed] [Google Scholar]
- Greco SJ, Smirnov SV, Murthy RG, Rameshwar P. Synergy between the RE-1 silencer of transcription and NFkappaB in the repression of the neurotransmitter gene TAC1 in human mesenchymal stem cells. J Biol Chem. 2007;282:30039–30050. doi: 10.1074/jbc.M703026200. [DOI] [PubMed] [Google Scholar]
- Ho WZ, Kaufman D, Uvaydova M, Douglas SD. Substance P augments interleukin-10 and tumor necrosis factor-alpha release by human cord blood monocytes and macrophages. J Neuroimmunol. 1996;71:73–80. doi: 10.1016/S0165-5728(96)00132-4. [DOI] [PubMed] [Google Scholar]
- Jagessar S, Gran B, Heijmans N, Bauer J, Laman J, ‘tHart BA, Constantinescu C. Discrepant effects of human interferon-gamma on clinical and immunological disease parameters in a novel marmoset model for multiple sclerosis. J Neuroimmune Pharmacol. 2012;7:253–265. doi: 10.1007/s11481-011-9320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janelsins BM, et al. Neurokinin-1 receptor agonists bias therapeutic dendritic cells to induce type 1 immunity by licensing host dendritic cells to produce IL-12. Blood. 2013;121:2923–2933. doi: 10.1182/blood-2012-07-446054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kincy-Cain T, Bost KL. Substance P-induced IL-12 production by murine macrophages. J Immunol. 1997;158:2334–2339. [PubMed] [Google Scholar]
- Kostyk SK, Kowall NW, Hauser SL. Substance P immunoreactive astrocytes are present in multiple sclerosis plaques. Brain Res. 1989;504:284–288. doi: 10.1016/0006-8993(89)91369-3. [DOI] [PubMed] [Google Scholar]
- Lassmann H, van Horssen J, Mahad D. Progressive multiple sclerosis: pathology and pathogenesis. Nat Rev Neurol. 2012;8:647–656. doi: 10.1038/nrneurol.2012.168. [DOI] [PubMed] [Google Scholar]
- Laurenzi MA, Persson MA, Dalsgaard CJ, Haegerstrand A. The neuropeptide substance P stimulates production of interleukin 1 in human blood monocytes: activated cells are preferentially influenced by the neuropeptide. Scand J Immunol. 1990;31:529–533. doi: 10.1111/j.1365-3083.1990.tb02801.x. [DOI] [PubMed] [Google Scholar]
- Levite M. Neuropeptides, by direct interaction with T cells, induce cytokine secretion and break the commitment to a distinct T helper phenotype. Proc Natl Acad Sci U S A. 1998;95:12544–12549. doi: 10.1073/pnas.95.21.12544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotz M, Carson D, Vaughan J. Substance P activation of rheumatoid synoviocytes: neural pathway in pathogenesis of arthritis. Science. 1987;235:893–895. doi: 10.1126/science.2433770. [DOI] [PubMed] [Google Scholar]
- Lotz M, Vaughan JH, Carson DA. Effect of neuropeptides on production of inflammatory cytokines by human monocytes. Science. 1988;241:1218–1221. doi: 10.1126/science.2457950. [DOI] [PubMed] [Google Scholar]
- Matis WL, Lavker RM, Murphy GF. Substance P induces the expression of an endothelial-leukocyte adhesion molecule by microvascular endothelium. J Investig Dermatol. 1990;94:492–495. doi: 10.1111/1523-1747.ep12874665. [DOI] [PubMed] [Google Scholar]
- Murphy FJ, Hayes MP, Burd PR. Disparate intracellular processing of human IL-12 preprotein subunits: atypical processing of the P35 signal peptide. J Immunol. 2000;164:839–847. doi: 10.4049/jimmunol.164.2.839. [DOI] [PubMed] [Google Scholar]
- Murthy RG, Greco SJ, Taborga M, Patel N, Rameshwar P. Tac1 regulation by RNA-binding protein and miRNA in bone marrow stroma: implication for hematopoietic activity. Brain Behav Immun. 2008;22:442–450. doi: 10.1016/j.bbi.2007.10.009. [DOI] [PubMed] [Google Scholar]
- Nessler S, et al. Suppression of autoimmune encephalomyelitis by a neurokinin-1 receptor antagonist–a putative role for substance P in CNS inflammation. J Neuroimmunol. 2006;179:1–8. doi: 10.1016/j.jneuroim.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Nio D, Moylan R, Roche J. Modulation of T lymphocyte function by neuropeptides. Evidence for their role as local immunoregulatory elements. J Immunol. 1993;150:5281–5288. [PubMed] [Google Scholar]
- O’Connor TM, et al. The role of substance P in inflammatory disease. J Cell Physiol. 2004;201:167–180. doi: 10.1002/jcp.20061. [DOI] [PubMed] [Google Scholar]
- Parham C, et al. A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R. J Immunol. 2002;168:5699–5708. doi: 10.4049/jimmunol.168.11.5699. [DOI] [PubMed] [Google Scholar]
- Pinto FM, Almeida TA, Hernandez M, Devillier P, Advenier C, Candenas ML. mRNA expression of tachykinins and tachykinin receptors in different human tissues. Eur J Pharmacol. 2004;494:233–239. doi: 10.1016/j.ejphar.2004.05.016. [DOI] [PubMed] [Google Scholar]
- Podda G, Nyirenda M, Crooks J, Gran B. Innate immune responses in the CNS: role of toll-like receptors, mechanisms, and therapeutic opportunities in multiple sclerosis. J Neuroimmune Pharmacol. 2013;8:791–806. doi: 10.1007/s11481-013-9483-3. [DOI] [PubMed] [Google Scholar]
- Reinke EK, et al. Substance P receptor mediated maintenance of chronic inflammation in EAE. J Neuroimmunol. 2006;180:117–125. doi: 10.1016/j.jneuroim.2006.07.010. [DOI] [PubMed] [Google Scholar]
- Ruff M, Wahl S, Pert C. Substance P receptor-mediated chemotaxis of human monocytes. Peptides. 1985;6:107–111. doi: 10.1016/0196-9781(85)90142-1. [DOI] [PubMed] [Google Scholar]
- Sanvito L, Constantinescu C, Gran B, ‘tHar B. The multifaceted role of interferon-gamma in central nervous system autoimmune demyelination. Open Autom J. 2010;2:151–159. doi: 10.2174/1876894601002040151. [DOI] [Google Scholar]
- Schratzberger P, et al. Differential chemotactic activities of sensory neuropeptides for human peripheral blood mononuclear cells. J Immunol. 1997;158:3895–3901. [PubMed] [Google Scholar]
- Scicchitano R, Biennenstock J, Stanisz A. In vivo immunomodulation by the neuropeptide substance P. Immunology. 1988;63:733–735. [PMC free article] [PubMed] [Google Scholar]
- Simeonidis S, et al. Regulation of the NK-1 receptor gene expression in human macrophage cells via an NF-kappa B site on its promoter. Proc Natl Acad Sci U S A. 2003;100:2957–2962. doi: 10.1073/pnas.0530112100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K, Tanaka A, Hara M, Nakanishi S. The primary structure and gene organization of human substance P and neuromedin K receptors. Eur J Biochem FEBS. 1992;204:1025–1033. doi: 10.1111/j.1432-1033.1992.tb16724.x. [DOI] [PubMed] [Google Scholar]
- Thakker P, Leach MW, Kuang W, Benoit SE, Leonard JP, Marusic S. IL-23 is critical in the induction but not in the effector phase of experimental autoimmune encephalomyelitis. J Immunol. 2007;178:2589–2598. doi: 10.4049/jimmunol.178.4.2589. [DOI] [PubMed] [Google Scholar]
- ‘tHart B, Gran B, Weissert R. EAE: imperfect but useful models of multiple sclerosis. Trends Mol Med. 2011;17:119–125. doi: 10.1016/j.molmed.2010.11.006. [DOI] [PubMed] [Google Scholar]
- Vandenbroeck K, et al. Chromosome 7q21-22 and multiple sclerosis: evidence for a genetic susceptibility effect in vicinity to the protachykinin-1 gene. J Neuroimmunol. 2002;125:141–148. doi: 10.1016/S0165-5728(02)00023-1. [DOI] [PubMed] [Google Scholar]
- Vishwanath R, Mukherjee R. Substance P promotes lymphocyte-endothelial cell adhesion preferentially via LFA-1/ICAM-1 interactions. J Neuroimmunol. 1996;71:163–171. doi: 10.1016/S0165-5728(96)00143-9. [DOI] [PubMed] [Google Scholar]
- Weinstock J. Substance P and the regulation of inflammation in infections and inflammatory bowel disease. Acta Physiol. 2014;2014:12428. doi: 10.1111/apha.12428. [DOI] [PubMed] [Google Scholar]
- Weinstock JV, Blum A, Metwali A, Elliott D, Arsenescu R. IL-18 and IL-12 signal through the NF-kappa B pathway to induce NK-1R expression on T cells. J Immunol. 2003;170:5003–5007. doi: 10.4049/jimmunol.170.10.5003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Expression of NK1R in various subsets of PBMCs from healthy human volunteers (n=3). The results are given as means and SEM of the percentage of cells expressing NK1R. (DOCX 13 kb)
NK1R expression in: PHA/IL-2 stimulated PBMCs (“blasts”) (Histograms A-H) and magnetically isolated CD4+ lymphocytes (Histogram I). Cells Gating: (A), non-gated; (B), CD56+ cells; (C), CD3+CD8- lymphocytes; (D), CD3+CD8+CD56-lymphocytes; (E), CD3-CD56+ cells; (F), CD3+CD56+ lymphocytes; (G), CD3+ lymphocytes; (H), CD8+ lymphocytes; (I), Lymphocytes. Colour legend: Black: Unstimulated cells; Red: IL-12-stimulated; Blue: IL-23-stimulated; Pink: Isotype control-bound cells. NK1R-APC: Allophycocyanin-conjugated mouse monoclonal anti-human NK1R (GIF 299 kb)
(TIFF 320 kb)
Dual-luciferase reporter assay with activation of NK1R promoter-reporter construct in Jurkat cells. The results represent mean ratios of Photinus/Renilla luminescence of two experiments after 24 h stimulation with different conditions. (GIF 104 kb)
(TIFF 36 kb)