Abstract
Objective
The objective was to examine the trajectory of five types of negative affect (global negative affect, fear, guilt, hostility, sadness) prior to and following three types of eating episodes (overeating in the absence of loss of control [OE-only], loss of control eating in the absence of overeating [LOC-only], and binge eating) among obese adults using ecological momentary assessment (EMA).
Method
Fifty obese adults (84% female) completed a two-week EMA protocol during which they were asked to record all eating episodes and rate each episode on continua of overeating and loss of control. Momentary measures of global negative affect, fear, guilt, hostility, and sadness were assessed using an abbreviated version of the Positive and Negative Affect Schedule (PANAS). Trajectories for each of the five types of negative affect were modeled prior to and following episodes of OE-only, LOC-only, and binge eating.
Results
Consistent with previous findings, global negative affect and Guilt increased prior to and decreased following binge eating episodes (all ps<.05). Guilt also decreased following OE-only episodes (p<.05).
Discussion
These results are consistent with the affect regulation model of binge eating and suggest that binge eating may function to regulate global negative affect, and more specifically, guilt among obese adults. These data suggest that the relationship between negative affect and binge eating may not be unique to individuals with clinical eating disorders and indicate that targeting negative affect may be an effective strategy for the treatment of binge eating in the context of obesity.
Binge eating, the consumption of an objectively large amount of food and a subjective feeling of loss of control during the eating episode1, has been linked to severe medical and psychiatric comorbidities2-4. Of particular concern is the association between binge eating and obesity. Although binge eating and obesity are not inextricably linked, individuals who binge eat are more likely to be obese than individuals without an eating disorder2 and binge eating is substantially more common among adolescents and adults with obesity than in the general population2,5,6. Furthermore, compared to either individual condition, the co-occurrence of binge eating and obesity appears to be particularly problematic as it is associated with more frequent weight fluctuations, greater consumption of calories, less exercise, and more severe psychopathology, including greater body dissatisfaction and disinhibition7-13.
The development of psychological treatments for binge eating in the context of obesity has burgeoned in the past decade, with multiple outcome studies devoted to cognitive behavioral guided self-help, cognitive behavioral therapy, behavioral weight loss, and low-energy-density dietary counseling14-17. Unfortunately, for some treatments like behavioral weight loss, the results appear mixed17 and even in the most promising of these treatments, 25% to 64% of the patients remained symptomatic14-16. As such, swift and marked improvements to the treatment of binge eating in the context of obesity are essential. There is a growing consensus that the enhancement of existing treatments as well as the innovation of novel treatments will depend on the identification of mechanisms that maintain binge eating over time18.
Affect Regulation Model of Binge Eating
An association between negative affect and binge eating in the context of obesity has been well-established in the extant literature. The affect regulation model19 posits that this observed association represents a functional relationship in which binge eating is triggered by and serves to mitigate high levels of negative affect. The affect regulation model further hypothesizes that because binge eating is an effective strategy for reducing negative affect, it is a learned behavior and is maintained through negative reinforcement (for a review of operant conditioning, please see Staddon & Cerutti, 2003). As described previously20, support for the affect regulation model of binge eating hinges on data demonstrating relatively high or increasing levels of negative affect prior to binge eating as well as relatively low or decreasing levels of negative affect following binge eating.
In gathering evidence for the affect regulation model of binge eating, ecological momentary assessment (EMA) has proven to be particularly useful. It allows for the real-time assessment of variables of interest (minimizing the risk of retrospective response bias21), the collection of data in the natural environment (as opposed to a laboratory setting), and the repeated assessment of key variables multiple times per day over relatively long periods of time (e.g., weeks or months). Perhaps most importantly, recent technological advances have made it possible to time- and date-stamp EMA assessments, providing the opportunity to more accurately delineate the temporal relationships between variables.
Negative Affect prior to Binge Eating
There is ample data suggesting that negative affect is relatively high prior to binge eating in the context of obesity. A recent meta-analysis of EMA studies found that, among individuals with binge eating disorder (BED), ratings of negative affect were higher before binge eating episodes than average ratings of negative affect (d=.77) as well as ratings of negative affect before regular eating episodes (d=.75)20. Although not all participants included in these studies were obese, given the high association between BED and obesity, these data suggest that negative affect may be elevated prior to binge eating in the context of obesity. More recently, EMA data that were specifically collected in an obese sample (the same dataset as the current study) suggest that binge eating in the context of obesity is more frequent on days characterized by high or increasing levels of negative affect22. However, these analyses did not examine the timing of binge eating; thus, conclusions about the temporal relationship between binge eating and negative affect cannot be made from these data. Non-EMA data (e.g., retrospective data, experimental data) have also examined the relationship between binge eating and negative affect, finding that negative affect is elevated prior to binge eating and is often cited as a trigger for binge eating23,24. The overall consistency of these results suggests that binge eating in the context of obesity may be triggered by high or increasing negative affect. However, these data do not provide any information about the relationship between negative affect and binge eating after binge eating occurs.
Negative Affect after Binge Eating
Compared to the data on negative affect prior to binge eating, the data on negative affect after binge eating is more mixed. The same EMA meta-analysis described above found that ratings of negative affect were higher after binge eating episodes than ratings made before binge eating episodes among individuals with unspecified binge eating (d=.46) and BED (d=.51)20. These data suggest that negative affect may continue to increase following binge eating in the context of obesity. However, EMA data from samples of adult women with anorexia nervosa25 and bulimia nervosa26 have demonstrated significant reductions in negative affect after binge eating. Further analyses of the bulimia nervosa sample suggest that the observed reductions in negative affect after binge eating were driven primarily by reductions in guilt and were present even when binge eating was not accompanied by purging27.
Objective
In sum, there is consistent support for the first tenet of the affect regulation model – that negative affect is relatively high or increasing prior to binge eating. However, there are inconsistent results related to the second tenet – that negative affect is relatively low or decreasing after binge eating. Some analyses suggest that negative affect increases after binge eating20 whereas data from other samples suggest that negative affect decreases after binge eating25,26. Determining whether negative affect increases or decreases after binge eating in the context of obesity has enormous clinical implications because these two findings indicate different maintenance mechanisms and consequently, different treatment strategies. Thus, further evaluation of the relationship between negative affect and binge eating in the context of obesity, particularly what happens to negative affect after binge eating occurs, is essential.
Thus, the primary objective of the current study was to examine the trajectory of global negative affect prior to and following three types of eating episodes among obese adults: overeating in the absence of loss of control (OE-only), loss of control eating in the absence of overeating (LOC-only), and binge eating which was defined as the combination of overeating and loss of control eating1, a. Based on the findings in anorexia nervosa25 and bulimia nervosa26, it was hypothesized that global negative affect would increase prior to and decrease following all three types of eating episodes. A secondary objective of the current study was to explore whether facets of negative affect (i.e., fear, guilt, hostility, and sadness) would be differentially associated with the occurrence of the three types of eating episodes. Based on the findings in bulimia nervosa 27, it was hypothesized that fluctuations in negative affect observed relative to the three types of eating episodes would be primarily driven by fluctuations in guilt even after controlling for fear, hostility, or sadness.
METHOD
Participants
Obese (BMI≥30) adults ranging in age from 18 to 65 were recruited to participate in the current study. Exclusion criteria were as follows: (a) current or lifetime criteria for DSM-IV anorexia nervosa (AN) or bulimia nervosa (BN), (b) regular use of compensatory behaviors (e.g., self-induced vomiting, laxative or diuretic misuse, fasting, or excessive exercise), (c) previous gastric bypass surgery, (d) current pregnancy or lactation, (e) current enrollment in treatment for obesity, or (f) inability to read and understand English. The endorsement of binge eating at baseline was not required for participation in the current study for two reasons. First, previous investigations have demonstrated that individuals who deny binge eating retrospectively may endorse binge eating when assessed in the moment28,29. Second, the objectives of the current study included examining momentary trajectories of negative affect relative to episodes of overeating-only and loss of control eating-only, both of which may be present in individuals who do not engage in binge eating.
Fifty obese adults (84% female, n=42) participated in the current study. On average, participants’ BMI was 40.3±8.5 (range=30.6 to 69.7) and all three classes of obesity were represented (Class I: n=11, 22%; Class II: n=22, 44%; Class III: n=17, 34%). Participants ranged in age from 21 to 64 years, with a mean age of 43.0±11.9 years. Most identified themselves as Caucasian (76%, n=38), followed by African American (14%, n=7), and Asian (6%, n=3), with other groups constituting 4% of the sample (n=2). The majority of participants were employed (78%, n=39), all but one had finished high school (98%, n=49), and a substantial minority had earned a 4-year college degree or higher (40%, n=20). Approximately half of the sample identified as being in a monogamous or committed relationship (first marriage, divorced/widowed and remarried, committed relationship: 48%, n=24), followed by “never been married” (34%, n=17) and divorced/widowed and not remarried (18%, n=9).
Measures
Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P)
The eating disorder module of the SCID-I/P30, a semi-structured interview that assesses current and lifetime history of Axis I psychopathology, was administered at baseline by trained assessors and supervised by one of the authors (CBP). The interview was used to establish current and lifetime DSM-IV AN (exclusion criteria), BN (exclusion criteria), and full- and sub-threshold BED (descriptive only). Criteria for full-threshold BED followed the guidelines provided in Appendix B of the DSM-IV-TR and included: a) binge eating that occurred at least twice per week for the past 6 months and that was accompanied by distress, b) three or more features associated with binge eating (e.g., eating more rapidly than normal, eating until uncomfortably full, eating large amounts of food when not physically hungry, eating alone because of feeling embarrassed about how much one is eating, and feeling disgusted, depressed, or guilty after eating), c) the absence of regular compensatory behaviors, and d) symptoms that were not better described by AN or BN31. Twelve (24%) were diagnosed at baseline with lifetime (including current) full- or sub-threshold BED, based on the SCID-I. The five participants who were given a sub-threshold BED diagnosis met all but one criterion for BED. Of these five participants, two met all criteria except that the binge eating episodes were not characterized by an objectively large amount of food (i.e., Subjective versus Objective Bulimic Episodes), two did not meet the frequency criteria (i.e., they reported binge eating less than twice per week), and one did not report distress associated with the binge eating episodes.
Beck Depression Inventory-II (BDI-II)
The BDI-II is a self-report measure of current depressive symptoms. The instrument includes 21 items that are rated on a four-point Likert scale ranging from 0 to 3, with higher scores indicating more severe symptoms. Cutoff scores for clinical significance have been suggested (0-13: minimal depression, 14-19: mild depression, 20-28: moderate depression, 29-63: severe depression); however, these are not necessarily meant to serve as diagnostic indicators. In the current study, the BDI-II was administered at baseline and was used descriptively. Scores ranged from 0 to 37, with a mean score of 10.2±8.2.
Positive and Negative Affect States (PANAS)
The PANAS32 is a self-report measure of both higher- (e.g., negative and positive) and lower-order (e.g., fear, joviality) dimensions of affect. Consistent with previous EMA research26, an abbreviated version of the PANAS was used to measure global negative affect. Participants were presented with 11 emotions (see below) and were asked to rate the extent to which they currently felt each of those emotions. The internal consistency of the abbreviated global negative affect subscale (α=.91) was consistent with the internal consistency of the full global negative affect scale when assessed at the momentary level (range of αs=.85-.91)33.
To measure the four facets of negative affect, the global negative affect scale was subdivided into the following four subscales, each comprised of two to four items: Fear (afraid, nervous, jittery), Guilt (ashamed, disgusted, dissatisfied with self, angry with self), Hostility (irritable, angry), and Sadness (lonely, sad)b. In a previous investigation, a confirmatory factor analysis replicated the original factor structure of the lower-order PANAS subscales using the abbreviated instrument with the exception that the Disgust item loaded onto the Guilt subscale rather than the Hostility subscale27. Thus, to maximize consistency between the current study and the Berg et al. (2013) study, the Disgust item was included in the Guilt subscale rather than the Hostility subscale. The internal consistencies of the four abbreviated lower-order negative affect subscales (Fear: α=.83; Guilt: α=.83; Hostility: α=.78; Sadness: α=.73) were consistent with the Berg et al. (2013) study.
Eating Episode Recordings
Participants were asked to record all eating episodes on the palmtop computers immediately after they occurred (i.e., event-contingent recording, see below for more detail). If an eating episode was not recorded immediately after it occurred, participants were given the opportunity to record the episode at the next signaled recording (i.e., signal-contingent recording; see below for more detail). After an eating episode, participants were asked to indicate the extent to which the eating episode was characterized by both overeating and loss of control over eating. To assess overeating, participants were asked to rate the extent to which they felt they had overeaten on a Likert scale from 1 (“not at all”) to 5 (“extremely”). To assess loss of control, participants were asked to rate each of the following four questions on the same scale: (a) “While you were eating, to what extent did you feel a sense of loss of control?”, (b) “While you were eating, to what extent did you feel that you could not resist eating?”, (c) “While you were eating, to what extent did you feel that you could not stop eating once you had started?”, and (d) “While you were eating, to what extent did you feel driven or compelled to eat?”.
An eating episode was categorized as overeating if the episode was rated ≥3 (i.e., at least “moderately”) on the overeating item. Similarly, an eating episode was characterized as loss of control eating if the episode was rated ≥3 (i.e., at least “moderately”) on at least one of the four loss of control items. Overeating-only episodes (OE-only) were then defined as eating episodes that met criteria for overeating but not loss of control eating, loss of control eating-only episodes (LOC-only) were defined as eating episodes that met criteria for loss of control eating but not overeating, and finally, binge eating episodes (binge eating) were defined as episodes that met criteria for both overeating and loss of control eating. A separate study using this dataset found significant, positive correlations between retrospective (EDE-Q) and momentary (EMA) assessments of binge eating, providing preliminary support for the construct validity of these definitions34.
Procedures
This study was approved by the Institutional Review Board of the University of Minnesota and all participants provided written, informed consent. Participants were recruited through community advertisements and flyers. Interested participants were initially screened over the phone for inclusion and exclusion criteria by a research coordinator. Participants who were eligible based on the phone screen were then invited to the research lab where they received information about the study, provided written informed consent, completed the eating disorder module of the SCID-I/P to determine eligibility, and received instructions for using the palmtop computers. After being trained on the EMA protocol, participants were given palmtop computers and practiced for 2 days. A secondary goal of this practice period was to minimize the potential for reactivity to the EMA protocol; although there is little evidence for this in the extant literature35. After the practice period, participants completed the EMA assessments over the next two weeks. During the two-week assessment period, one in-person visit was scheduled with each participant during which data from the palmtop computers were uploaded and participants were provided feedback regarding their compliance by a trained research coordinator. Participants received $150 for completing the two-week EMA protocol and could earn a $50 bonus for completing at least 90% of the signal-contingent recordings (see below) within 45 minutes of the signal.
Consistent with previous investigations25,26, the current EMA assessment protocol implemented three types of daily self-report methods: 1) signal-contingent recording, 2) interval-contingent recording, and 3) event-contingent recording36. Signal-contingent recording requires participants to complete EMA assessment ratings when prompted by the palmtop computers. In the current study, participants were prompted to complete six signal-contingent recordings each day. These recordings occurred at semi-random times throughout the day but were all within +/− 20 minutes of each of the six “anchor” times distributed evenly throughout the day: 8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m. Interval-contingent recording requires participants to complete ratings at specified intervals. In the current study, participants were instructed to complete EMA assessment ratings at the end of each day. Finally, event-contingent recording requires participants to complete ratings before or after a specified event occurs. In the current study, participants were instructed to provide EMA assessment ratings immediately after all eating episodes. During all EMA recordings, participants completed the PANAS and indicated whether they had eaten since their last recording. If participants had eaten since their last recording, they were also asked to indicate the extent to which the eating episode was characterized by overeating and/or loss of control eating. Handspring Visors were used for the EMA hardware. The EMA software was Satellite Forms Version 3.1.
Statistical Methods
To examine the temporal relationship between the negative affect subscales (i.e., global negative affect, Fear, Guilt, Hostility, and Sadness) and the three types of eating episodes (i.e., OE-only, LOC-only, and binge eating), the pre- and post-event trajectories of each negative affect subscale were modeled separately using piecewise linear, quadratic, and cubic functions centered on the time at which each of the eating episodes occurred. Thus, momentary observations (Level 1) were nested within subjects (Level 2). The linear functions (i.e., hours prior to event, hours following event) reflected the rate of change in affect prior to and following the eating episodes, the quadratic functions (i.e., [hours prior to event]2, [hours following event]2) reflected the acceleration or deceleration in rate of affect change prior to and following the eating episodes, and the cubic functions (i.e., [hours prior to event]3, [hours following event]3) reflected either further acceleration or dampening of the acceleration/deceleration in rate of affect change. Including the quadratic and cubic functions, in addition to the linear function, allows for an accurate depiction of the relationship between binge eating and negative affect in the event that this relationship is non-linear and has multiple deflection points. In instances when more than one of the eating episodes of interest was reported in a single day, only the first eating episode was used to avoid confounding the relationship between antecedent and consequent affect ratings. Furthermore, if subsequent eating episode(s) of interest occurred within the four-hour time frame following the first eating episode, only affect ratings made after the first eating episode and prior to the subsequent eating episode(s) were included in the post-event analyses. A first-order autoregressive covariance structure (AR1) was used to account for serial correlations. Analyses were conducted in SPSS 19 and were based on all available data. Missing data were not imputed.
RESULTS
EMA Measurements
On average, participants made recordings on 13.9±2.5 days (range=5 to 16 days). The mean number of recordings per day ranged from 4.6 to 15.0, with an overall average of 10.7±2.1 recordings. The total number of recordings per subject ranged from 46 to 225 with an average of 150.5 (SD=42.6). Participants’ compliance was determined by adding the percentage of signal-contingent ratings that were completed within 45 minutes of the prompt and the percentage of interval-contingent ratings that were completed. Overall, compliance during the two-week EMA protocol was good (mean=82.2%; median=87.55%).
Each of the three types of eating episodes was endorsed by the majority of the sample at some point during the two-week EMA procedure. Specifically, OE-only episodes were endorsed by 80% (n=40), LOC-only episodes were endorsed by 84% (n=42), and binge eating episodes were endorsed by 96% (n=48) of the sample. The frequency of these eating episodes varied substantially among the participants. The average frequencies of OE-only, LOC-only, and binge eating episodes per person during the two-week EMA procedure were 9.0 (SD=8.9), 8.0 (SD=10.3), 7.1 (SD=8.3), respectively. Analyses were based on observations of 505 OE-only, 431 LOC-only, and 395 binge eating episodes. Additional information regarding the frequency of OE-only, LOC-only, and binge eating episodes in the current sample has been described previously22. There were no differences in behavior or affect ratings made in Week 1 versus Week 2 of the protocol.
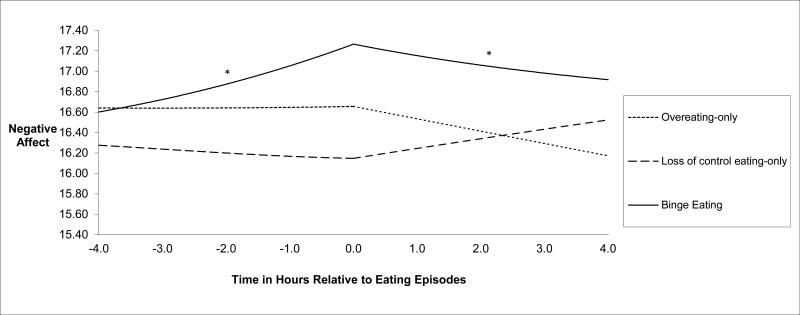
Within-Day Analyses for Global Negative Affect
The results of the within-day analyses for global negative affect are provided in Table 1 and illustrated in Figure 1. Both pre- and post-event linear components in the binge eating model were significant indicating a change in the trajectory of global negative affect before and after binge eating episodes (ps<.05; see Table 1). The directionality of the linear components indicates that global negative affect increased significantly in the four hours prior to binge eating episodes and decreased significantly in the four hours following binge eating episodes. There were no significant findings for the quadratic or cubic components of the binge eating model or for any of the components of the OE-only or LOC-only models.
Table 1.
Within-Day Multilevel Models of the Four Facets of Negative Affect Relative to Eating Episodes
| Fear |
Guilt |
Hostility |
Sadness |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t | Est. | SE | 95% CI | t |
| Overeating-Only | ||||||||||||||||
| Intercept | 1.32 | .05 | 1.21, 1.41 | 26.11*** | 1.50 | .06 | 1.38, 1.61 | 26.06*** | 1.42 | .05 | 1.33, 1.51 | 31.59*** | 1.55 | .06 | 1.43, 1.67 | 26.13*** |
| Hours prior to event | −0.01 | .01 | −.03, .01 | −02.12 | 0.02 | .01 | .00, .04 | 01.82 | 0.00 | .01 | −.02, .02 | 00.12 | 0.02 | .01 | .00, .04 | 01.61 |
| (Hours prior to event)2 | −0.00 | .00 | .00, .00 | −01.25 | 0.00 | .00 | .00, .00 | 00.53 | −0.00 | .00 | .00, .00 | −00.21 | 0.00 | .00 | .00, .00 | 00.61 |
| (Hours prior to event)3 | −0.00 | .00 | .00, .00 | −00.90 | 0.00 | .00 | .00, .00 | 00.30 | −0.00 | .00 | .00, .00 | −00.12 | 0.00 | .00 | .00, .00 | 00.43 |
| Hours following event | 0.01 | .01 | −.01, .03 | 00.85 | −0.02 | .01 | −.04, .00 | −02.06* | 0.00 | .01 | −.02, .03 | 00.31 | −0.01 | .01 | −.04, .01 | −01.03 |
| (Hours following event)2 | 0.00 | .00 | .00, .00 | 01.27 | −0.00 | .00 | .00, .00 | −00.47 | 0.00 | .00 | .00, .00 | 00.18 | −0.00 | .00 | .00, .00 | −00.69 |
| (Hours following event)3 | 0.00 | .00 | .00, .00 | 00.90 | −0.00 | .00 | .00, .00 | −00.31 | 0.00 | .00 | .00, .00 | 00.12 | −0.00 | .00 | .00, .00 | −00.42 |
| Loss of Control Eating-Only | ||||||||||||||||
| Intercept | 1.28 | .04 | 1.19, 1.37 | 28.79*** | 1.45 | .06 | 1.33, 1.56 | 24.81*** | 1.35 | .04 | 1.26, 1.44 | 30.70*** | 1.51 | .06 | 1.39, 1.63 | 25.09*** |
| Hours prior to event | −0.02 | .02 | −.05, .01 | −01.30 | 0.00 | .02 | −.03, .04 | 00.23 | −0.02 | .02 | −.06, .02 | −01.02 | 0.02 | .02 | −.03, .06 | 00.78 |
| (Hours prior to event)2 | −0.00 | .00 | −.01, .00 | −00.94 | 0.00 | .00 | −.01, .01 | 00.39 | 0.00 | .00 | −.01, .01 | 00.03 | 0.00 | .00 | −.01, .01 | 00.68 |
| (Hours prior to event)3 | −0.00 | .00 | .00, .00 | −00.70 | 0.00 | .00 | .00, .00 | 00.75 | 0.00 | .00 | .00, .00 | 00.76 | 0.00 | .00 | .00, .00 | 00.79 |
| Hours following event | 0.03 | .02 | .00, .06 | 01.68 | 0.00 | .02 | −.03, .04 | 00.22 | 0.03 | .02 | −.01, .08 | 01.49 | −0.00 | .02 | −.05, .04 | −00.18 |
| (Hours following event)2 | 0.00 | .00 | .00, .01 | 00.91 | −0.00 | .00 | −.01, .01 | −00.42 | −0.00 | .00 | −.01, .01 | −00.06 | −0.00 | .00 | −.01, .01 | −00.72 |
| (Hours following event)3 | 0.00 | .00 | .00, .00 | 00.71 | −0.00 | .00 | .00, .00 | −00.75 | −0.00 | .00 | .00, .00 | −00.76 | −0.00 | .00 | .00, .00 | −00.76 |
| Binge Eating | ||||||||||||||||
| Intercept | 1.36 | .06 | 1.25, 1.47 | 23.84*** | 1.55 | .06 | 1.41, 1.68 | 23.37*** | 1.47 | .05 | 1.36, 1.57 | 28.72*** | 1.60 | .07 | 1.47, 1.74 | 23.89*** |
| Hours prior to event | −0.00 | .01 | −.02, .02 | −00.35 | 0.03 | .01 | .01, .06 | 02.63** | 0.01 | .01 | −.02, .04 | 00.70 | 0.02 | .01 | −.01, .05 | 01.29 |
| (Hours prior to event)2 | −0.00 | .00 | .00, .02 | −00.50 | 0.00 | .00 | .00, .01 | 01.47 | 0.00 | .00 | .00, .00 | 00.39 | 0.00 | .00 | .00, .01 | 00.46 |
| (Hours prior to event)3 | −0.00 | .00 | .00, .00 | −00.27 | 0.00 | .00 | .00, .00 | 01.10 | 0.00 | .00 | .00, .00 | 00.30 | 0.00 | .00 | .00, .00 | 00.32 |
| Hours following event | −0.00 | .01 | −.03, .00 | −00.14 | −0.05 | .02 | −.08, −.02 | −03.10** | −0.02 | .02 | −.06, .01 | −01.37 | −0.02 | .02 | −.06, .02 | −01.11 |
| (Hours following event)2 | −0.00 | .00 | .00, .00 | 00.75 | −0.00 | .00 | .00, .00 | −00.64 | 0.00 | .00 | .00, .00 | 00.59 | −0.00 | .00 | .00, .00 | −00.08 |
| (Hours following event)3 | −0.00 | .00 | .00, .00 | 00.25 | −0.00 | .00 | .00, .00 | −01.16 | −0.00 | .00 | .00, .00 | −00.38 | −0.00 | .00 | .00, .00 | −00.35 |
Note. Est.=estimate; SE=standard error; Hours prior to event=pre-eating episode linear function, which reflects the rate of change in affect prior to the eating episode; (Hours prior to event)2 = pre-eating episode quadratic function, which reflects the acceleration or deceleration in rate of affect change prior to the eating episode; (Hours prior to event]3 = pre-eating episode cubic function, which reflects further acceleration or deceleration in rate of affect change prior to the eating episode; Hours following event=post-eating episode linear function, which reflects the rate of change in affect following the eating episode; (Hours following event)2 = post-eating episode quadratic function, which reflects the acceleration or deceleration in rate of affect change following the eating episode; (Hours following event)3 = post-eating episode cubic function, which reflects further acceleration or deceleration in rate of affect change following the eating episode.
p<.05.
p<.01.
p<.001
Figure 1.
Temporal association between higher-order negative affect subscale and overeating-only, loss of control eating-only, and binge eating episodes. The figure shows the momentary levels and trajectories of global negative affect associated with overeating-only, loss of control eating-only, and binge eating episodes. The pre- and post-event trajectories of global negative affect were modeled separately using piecewise linear, quadratic, and cubic functions centered on the time at which each of the eating episodes occurred. Momentary observations (Level 1) were nested within subjects (Level 2). Both pre- and post-event linear components in the binge eating model were significant indicating a change in the trajectory of global negative affect before and after binge eating episodes. The scaling of the y-axis ranged from 11.0 to 55.0.
*p<.05.
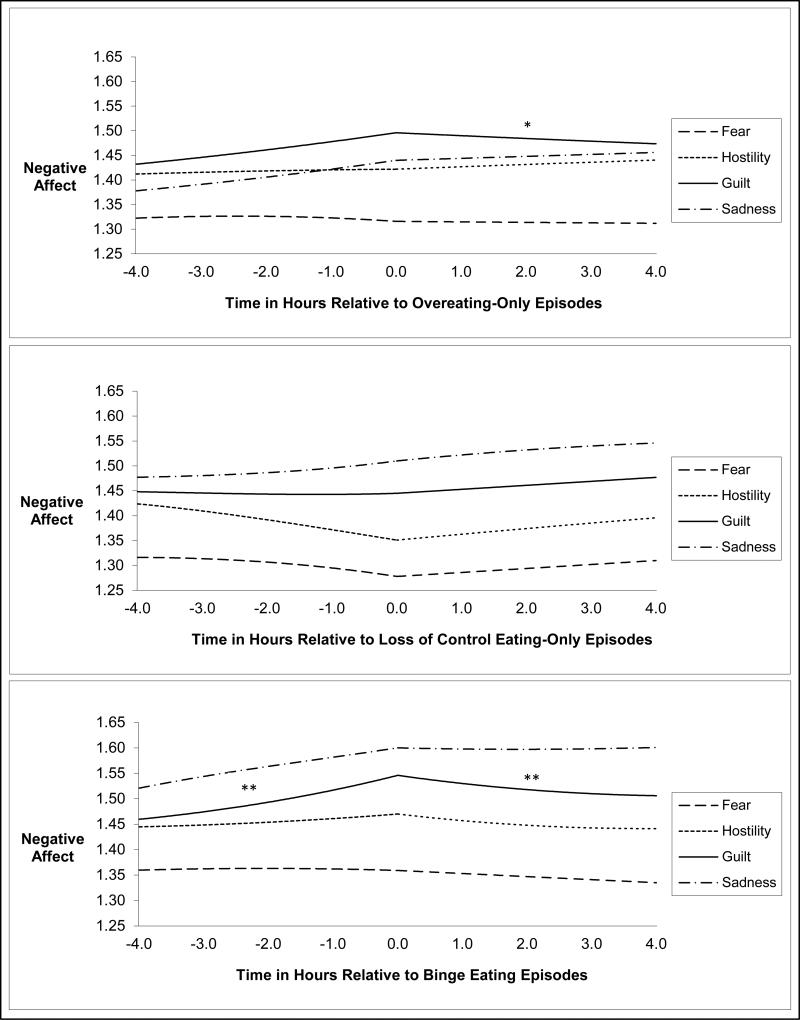
Within-Day Analyses for Facets of Negative Affect
The results of the within-day analyses for the facets of negative affect are provided in Table 1 and illustrated in Figure 2. With regard to Guilt, there were significant findings for both the pre- and post-event linear components of the binge eating model (ps<.01; see Table 1) as well as the post-event linear component of the OE-only model (p<.05; see Table 1). These data suggest that there was a significant change in the trajectory of Guilt prior to binge eating episodes and following both binge eating and OE-only episodes. The directionality of the linear components indicates a significant increase in Guilt in the four hours prior to binge eating episodes and a significant decrease in Guilt in the four hours following both binge eating and OE-only episodes. There were no significant effects for Guilt in the LOC-only model, indicating that the level (i.e., intensity) of Guilt did not vary relative to episodes of LOC eating-only. Additionally, there were no significant findings for any of the other facets of negative affect suggesting that the levels (i.e., intensities) of Fear, Hostility, and Sadness did not vary in relation to OE-only, LOC-only, or binge eating episodes. To further examine the unique effects of Guilt on binge eating and OE-only episodes, the within-day analyses described above were repeated, this time examining Guilt individually using Fear, Hostility, and Sadness as covariates. These post hoc analyses indicated that Guilt still increased prior to and decreased after binge eating episodes and decreased after OE-only episodes even after controlling for Fear, Hostility, and Sadness (all ps<.05).
Figure 2.
Temporal association between lower-order negative affect subscales and overeating-only, loss of control eating-only, and binge eating episodes. The figure shows the momentary levels and trajectories of the facets of negative affect associated with overeating-only, loss of control eating-only, and binge eating episodes. The pre- and post-event trajectories of each negative affect subscale were modeled separately using piecewise linear, quadratic, and cubic functions centered on the time at which each of the eating episodes occurred. Momentary observations (Level 1) were nested within subjects (Level 2). With regard to Guilt, there were significant findings for both the pre- and post-event linear components of the binge eating model as well as the post-event linear component of the OE-only model. The scaling of the y-axis ranged from 1.0 to 5.0.
*p<.05. **p<.01.
DISCUSSION
The results indicate that there was a significant increase in global negative affect in the four hours prior to binge eating episodes and a significant decrease in global negative affect in the four hours following binge eating episodes. In contrast, global negative affect did not fluctuate in relation to either OE-only or LOC-only episodes. With regard to the facets of negative affect, Guilt was the only facet to fluctuate in relation to binge eating episodes. In this sample, Guilt increased significantly in the four hours prior to binge eating episodes and decreased significantly in the four hours following binge eating episodes. These results held even after controlling for the other facets of negative affect. In contrast, with the exception of a significant decrease in Guilt in the four hours following OE-only episodes, there were no significant fluctuations in any of the facets of negative affect prior to or following OE-only or LOC-only episodes.
Implications for Maintenance Models of Binge Eating in the Context of Obesity
The main findings from the current study, that global negative affect increased in the four hours prior to binge eating episodes and decreased in the four hours after binge eating, are consistent with both tenets of the affect regulation model of binge eating. These data replicate findings from two previous EMA investigations of negative affect and binge eating in anorexia nervosa25 and bulimia nervosa26. Additionally, the finding that Guilt increased in the four hours prior to and decreased in the four hours after binge eating episodes replicates research on Guilt and binge eating in bulimia nervosa27 and adds specificity to the affect regulation model of binge eating. Overall, these results suggest that the function of binge eating in the context of obesity may be to mitigate negative affect generally, and guilt specifically. These data also suggest that the function of binge eating among obese adults is similar to the function of binge eating in adult women with anorexia nervosa and bulimia nervosa. Although there was a significant decrease in Guilt following OE-only episodes, there was no significant fluctuation in Guilt prior to these eating episodes. These data suggest that whereas OE-only episodes may function to mitigate guilt, fluctuations in guilt may not precipitate or trigger this type of eating behavior. Finally, in this sample, the function of LOC-only episodes appeared unrelated to global negative affect or any of the facets of negative affect. In other words, in this sample, LOC-only episodes did not appear to be precipitated, triggered, or maintained by global negative affect or any of the facets of negative affect.
Although these data are consistent with results from three previous EMA studies in anorexia nervosa25 and bulimia nervosa26,27, these data also contradict findings from the Haedt-Matt & Keel (2011) meta-analysis (described above). The most likely explanation for the observed inconsistencies between these studies is the fact that different analytic approaches were used. Given the statistical constraints associated with meta-analyses, the Haedt-Matt & Keel (2011) study compared two specific ratings of negative affect - the most proximal pre-binge rating and the most proximal post-binge rating (referred to hereafter as the “single comparison approach”). In contrast, the current study, along with three other EMA studies25-27, used multilevel modeling to examine the trajectory of negative affect over time relative to episodes of binge eating (referred to hereafter as the “multilevel modeling approach”). Analyses using the single comparison approach have consistently found that post-binge negative affect is higher than pre-binge negative affect (suggesting that negative affect increases after binge eating) whereas analyses using the multilevel modeling approach have consistently found that negative affect increases prior to and decreases following binge eating episodes (suggesting that negative affect decreases after binge eating). In fact, the Engel et al. (2013) demonstrated that even when these two analytic approaches were conducted with the same dataset, the expected results were still found - the single comparison approach found that post-binge negative affect was higher than pre-binge negative affect whereas the multilevel modeling approach found that negative affect decreased after binge eating. Therefore, it is possible (and perhaps likely) that the results of the current study would be different if these data were analyzed using the single comparison approach. However, it is arguable that the multilevel modeling approach used in the current study is the more statistically rigorous approach because it uses all available data (as opposed to single data points) and because it locates each rating in time (as opposed to assuming that all ratings were made at the same point in time relative to the binge eating episode). However, additional research is still needed to reconcile these two approaches and provide an explanation for their consistently inconsistent results.
Implications for Treatment
These data have important implications for the treatment of obesity, and in particular, the treatment of binge eating in the context of obesity. First, although the majority of the sample did not meet criteria for either full- or subthreshold BED at baseline, all but two of the participants endorsed binge eating during the two-week EMA protocol. The near universality of self-reported binge eating in this sample, combined with the high frequency with which it was endorsed, suggests that binge eating may be more common and more pervasive in obese adults than previously recognized. These data suggest that binge eating may be an important target in obesity treatments regardless of whether patients endorse binge eating during their initial assessment.
Second, these data suggest that treatments for binge eating in the context of obesity should address the functionality of binge eating, with particular attention given to the role of negative affect. For example, treatments that focus on decreasing the intensity and/or lability of negative affect could reduce patients’ drive to binge eat. Alternatively, treatments that aim to increase distress tolerance (i.e., the ability to “sit with” negative emotions without attempting to modulate them) or the use of adaptive coping strategies (i.e., alternative behaviors that can be used to mitigate negative affect) could also result in a decreased drive to binge eat. Such emotion-focused treatments (e.g., Dialectical Behavior Therapy, Acceptance and Commitment Therapy, Integrative Cognitive-Affective Therapy) have been applied to the treatment of binge eating within the context of eating disorders with promising results37-41. However, these treatments have been slower to develop in the field of obesity. Therapeutic approaches that aim to change emotional experiences indirectly through the modification of cognitions and behavior (e.g., Cognitive Behavioral Therapy) may also be effective, especially for addressing feelings of guilt that stem from self-devaluative cognitive processes. Although these data demonstrate a potentially important temporal relationship between negative affect and binge eating, these data do not preclude the possibility that additional factors (e.g., nutritional status, positive affect) could also be temporally and functionally associated with binge eating. Additional, more comprehensive data is needed to delineate the unique contributions of each of these variables to the occurrence of binge eating in the context of obesity.
Finally, these data further implicate the importance of specifically addressing feelings of guilt in the treatment of binge eating. It is important to note that although the subscale is titled “Guilt”, the item content of the Guilt subscale (i.e., “angry with self”, “ashamed”, “disgusted”, “dissatisfied with self”) may be more suggestive of “shame” (i.e., embarrassment, inadequacy) than “guilt” (i.e., culpability). Regardless of whether the specific emotional content is guilt or shame, these data suggest that self-referential feelings of dissatisfaction and disgust are associated with binge eating. Unfortunately, these data do not provide any context for the feelings of guilt/shame (e.g., guilt/shame regarding binge eating versus body size versus interpersonal situations versus work/school-related issues) and future research is needed to delineate the context of guilt/shame as it relates to the functionality of binge eating.
Strengths and Limitations
There are several notable strengths of the current study. First, data were collected using electronic, time-stamped EMA, which decreases the risk of recall biases, allows for repeated assessments in the natural environment, and maximizes the accuracy of temporal associations between assessments. Second, the trajectory of affect before and after eating episodes was modeled using all available data points, which provides a highly nuanced representation of the temporal relationship between affect and behavior. Third, participants were recruited from the community and were not required to endorse binge eating at baseline, which increases the generalizability of the findings. Fourth, both overeating and loss of control were rated independently and dimensionally. Given that lay definitions of binge eating tend to be characterized primarily by the quality of loss of control regardless of the amount of food consumed, there are concerns that self-reported binge eating is more reflective of loss of control eating than binge eating. The collection of independent, dimensional measurements of the two components of binge eating (i.e., overeating, loss of control) may provide a method for measuring binge eating that is less susceptible to bias from participants’ preconceived notions of what constitutes binge eating. Furthermore, independent assessments of overeating and loss of control allowed for separate analyses of OE-only, LOC-only, and binge eating episodes and their relationships to negative affect.
Despite these strengths, limitations of these data should also be noted. First, although overeating and loss of control were rated independently and dimensionally, these variables were still self-rated by participants. As such, ratings of overeating and loss of control may not have been consistent across participants. Furthermore, the extent to which self-ratings of overeating and loss of control are similar to ratings made by trained assessors is unclear at this time. For example, overeating may have been more reflective of perceived overeating than objective overeating (based on kilocalories consumed). Thus, conclusions about the functionality of subjective versus objective bulimic episodes cannot be made using these data. However, given the differential findings for the three types of eating episodes, there does appear to be a unique and important relationship between affect and those eating episodes that are perceived as being high on dimensions of overeating and loss of control. A second limitation is the fact that global negative affect, Fear, Guilt, Hostility, and Sadness were all measured using abbreviated subscales. The decision to use these abbreviated scales was motivated by a desire to decrease the assessment burden on participants given the frequency of EMA ratings. This decision was informed by previous EMA research demonstrating a similar factor structure and internal reliabilities as the full scales (e.g., Berg et al., 2013). A third limitation is that not all of the participants endorsed each of the three types of eating episodes, which means that the results for each of the eating episodes are based on a subset of the full sample. A fourth limitation was that the majority of participants in the current study were Caucasian females, which may limit the generalizability of the findings to men and racial/ethnic minorities. A fifth limitation is that these data are descriptive and do not indicate a causal relationship between negative affect and eating behaviors.
A final limitation is that the current sample was heterogeneous with regard to age, BMI, BED diagnostic status, treatment history, and depression symptoms. It is possible, and perhaps probable, that there are individual differences in the extent to which affect fluctuates relative to binge eating episodes as well as the extent to which binge eating functions to regulate affect. Another possibility is that some binge eating episodes may function to regulate affect whereas others do not. Examining potential moderators is a clear next step in this area of research, given the limited power to conduct moderator analyses with the sample size of the current study. Given that the results of the current study were based on within-subject analyses, the use of between-subject covariates (e.g., age, diagnostic status) would not change the results. Thus, additional research with greater power is needed to examine moderators of the observed relationship between negative affect and binge eating.
Conclusions
Consistent with previous investigations in anorexia nervosa and bulimia nervosa, these data demonstrated a temporal relationship between negative affect, guilt, and binge eating in which both negative affect and guilt increased in the four hours prior to and decreased in the four hours after episodes of binge eating among obese adults. These findings are consistent with the affect regulation model which posits that binge eating in the context of obesity functions to mitigate negative affect and is maintained through negative reinforcement. Additionally, these data further specify that the function of binge eating may be to specifically avoid or reduce feelings of guilt rather than feelings of fear, hostility, or sadness. Overall, these results suggest that the relationship between affect and binge eating may not be a phenomenon unique to individuals with clinical eating disorders and implicate the importance of targeting negative affect and the functionality of binge eating in treatments for obesity.
Acknowledgments
This research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (P30DK 50456) and the National Institute of Mental Health (T32 MH082761-01).
Footnotes
Given inconsistent definitions of binge eating in the extant literature 23,24,42 as well as discrepancies between investigator and lay definitions of binge eating 43, the relationships between negative affect and the three types of eating episodes were evaluated separately to determine whether negative affect is differentially associated with overeating, loss of control, or the combination.
The terms fear, guilt, hostility, and sadness will be capitalized when referring to the PANAS subscales.
Contributor Information
Kelly C. Berg, University of Minnesota
Ross D. Crosby, Neuropsychiatric Research Institute University of North Dakota School of Medicine and Health Sciences
Li Cao, Neuropsychiatric Research Institute.
Scott J. Crow, University of Minnesota The Emily Program
Scott G. Engel, Neuropsychiatric Research Institute University of North Dakota School of Medicine and Health Sciences
Stephen A. Wonderlich, Neuropsychiatric Research Institute University of North Dakota School of Medicine and Health Sciences
Carol B. Peterson, University of Minnesota The Emily Program
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Jr., Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;61:358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mannucci E, Tesi F, Ricca V, Pierazzuoli E, Barciulli E, Moretti S, et al. Eating behavior in obese patients with and without type 2 diabetes mellitus. Int J Obes. 2002;26:848–853. doi: 10.1038/sj.ijo.0801976. [DOI] [PubMed] [Google Scholar]
- 4.Goodwin RD, Hoven CW, Spitzer RL. Diabetes and eating disorders in primary care. Int J Eat Disord. 2003;33:85–91. doi: 10.1002/eat.10106. [DOI] [PubMed] [Google Scholar]
- 5.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Decaluwe V, Braet C, Fairburn CG. Binge eating in obese children and adolescents. Int J Eat Disord. 2003;33:78–84. doi: 10.1002/eat.10110. [DOI] [PubMed] [Google Scholar]
- 7.Goldschmidt AB, Le Grange D, Powers P, Crow SJ, Hill LL, Peterson CB, et al. Eating disorder symptomatology in normal-weight vs. obese individuals with binge eating disorder. Obesity. 2011;19:1515–1518. doi: 10.1038/oby.2011.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu LKG, Mulliken B, McDonagh B, Krupa Das S, Rand W, Fairburn CG, et al. Binge eating disorder in extreme obesity. International Journal of Obesity. 2002;26:1398–1403. doi: 10.1038/sj.ijo.0802081. [DOI] [PubMed] [Google Scholar]
- 9.Striegel-Moore RH, Wilson GT, Wilfley DE, Elder KA, Brownell KD. Binge eating in an obese community sample. International Journal of Eating Disorders. 1998;23:37. doi: 10.1002/(sici)1098-108x(199801)23:1<27::aid-eat4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 10.de Zwaan M, Mitchell JE, Seim HC, Specker SM, Pyle RL, Raymond NC, et al. Eating related and general psychopathology in obese females with binge eating disorder. International Journal of Eating Disorders. 1994;15:43–52. doi: 10.1002/1098-108x(199401)15:1<43::aid-eat2260150106>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 11.Wadden TA, Foster GD, Letizia KA, Wilk JE. Metabolic, anthropometric, and psychological characteristics of obese binge eaters. International Journal of Eating Disorders. 1993;14:17–25. doi: 10.1002/1098-108x(199307)14:1<17::aid-eat2260140103>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 12.Yanovski SZ, Leet M, Yanovski JA, Flood M, Gold PW, Kissileff HR, et al. Food selection and intake of obese women with binge-eating disorder. American Journal of Clinical Nutrition. 1992;56:975–980. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]
- 13.Goldfein JA, Walsh BT, Devlin MJ, LaChaussee JL, Kissileff HR. Eating behavior in binge eating disorder. Int J Eat Disord. 1993;14:427–431. doi: 10.1002/1098-108x(199312)14:4<427::aid-eat2260140405>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 14.Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, White MA. Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. J Consult Clin Psychol. 2011;79:675–685. doi: 10.1037/a0025049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masheb RM, Grilo CM, Rolls BJ. A randomized controlled trial for obesity and binge eating disorder: Low-energy-density dietary counseling and cognitive-behavioral therapy. Behav Res Ther. 2011;49:821–829. doi: 10.1016/j.brat.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.StriegelMoore RH, Wilson GT, DeBar L, Perrin N, Lynch F, Rosselli F, et al. Cognitive behavioral guided self-help for the treatment of recurrent binge eating. J Consult Clin Psychol. 2010;78:312–321. doi: 10.1037/a0018915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005?2012. Int J Eat Disord. 2013;46:462–469. doi: 10.1002/eat.22103. [DOI] [PubMed] [Google Scholar]
- 18.Strauman TJ, Merrill KA. The basic science/clinical science interface and treatment development. Clinical Psychology: Science and Practice. 2004;11:263–266. [Google Scholar]
- 19.Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. Guilford Press; New York, NY: 1993. pp. 173–205. [Google Scholar]
- 20.Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- 22.Berg KC, Peterson CB, Crosby RD, Cao L, Crow SJ, Engel SG, et al. Relationship between daily affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry Research. 2014;215:185–191. doi: 10.1016/j.psychres.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arnow B, Kenardy J, Agras WS. Binge eating among the obese: A descriptive study. Journal of Behavioral Medicine. 1992;15:155–170. doi: 10.1007/BF00848323. [DOI] [PubMed] [Google Scholar]
- 24.Agras WS, Telch CF. The effects of caloric deprivation and negative affect on binge eating in obese binge-eating disordered women. Behavior Therapy. 1998;29:491–503. [Google Scholar]
- 25.Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow SJ, Peterson CB, et al. The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology. 2013;122:709–719. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- 27.Berg KC, Peterson CB, Crosby RD, Cao L, Engel SG, Mitchell JE, et al. Facets of negative affect prior to and following episodes of binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology. 2013;122:111–118. doi: 10.1037/a0029703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. Journal of Consulting and Clinical Psychology. 2000;68:95–102. [PubMed] [Google Scholar]
- 29.Le Grange D, Gorin A, Catley D, Stone AA. Does momentary assessment detect binge eating in overweight women that is denied at interview? European Eating Disorders Review. 2001;9:309–324. [Google Scholar]
- 30.First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for the DSM-IV axis I disorders - patient edition (SCID-I/P, version 2) New York State Psychiatric Institute; Biometrics Research Department; New York: 1995. [Google Scholar]
- 31.American Psychiatric Association . Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR) APA; Washington, D.C.: 2000. [Google Scholar]
- 32.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 33.Watson D, Clark LA. The panas-X: Manual for the positive and negative affect schedule - expanded form. 1994 [Google Scholar]
- 34.Wonderlich JA, Lavender JM, Wonderlich SA, Peterson CB, Crow SJ, Engel SG, et al. Examining convergence of retrospective and ecological momentary assessment measures of negative affect and eating disorder behaviors. Int J Eat Disord. 2014 doi: 10.1002/eat.22352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farchus Stein K, Corte CM. Ecologic momentary assessment of eating-disordered behaviors. Int J Eat Disord. 2003;34:349–360. doi: 10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]
- 36.Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. Journal of Personality. 1991;59:339–354. [Google Scholar]
- 37.Safer DL, Robinson AH, Jo B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behavior Therapy. 2010;41:106–120. doi: 10.1016/j.beth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- 39.Wonderlich SA, Peterson CB, Crosby RD, Smith TL, Klein MH, Mitchell JE, et al. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychological Medicine. 2013:1–11. doi: 10.1017/S0033291713001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Juarascio A, Shaw J, Forman E, Timko CA, Herbert J, Butryn M, et al. Acceptance and commitment therapy as a novel treatment for eating disorders: An initial test of efficacy and mediation. Behavior Modification. 2013;37:459–489. doi: 10.1177/0145445513478633. [DOI] [PubMed] [Google Scholar]
- 41.Juarascio AS, Forman EM, Herbert JD. Acceptance and commitment therapy versus cognitive therapy for the treatment of comorbid eating pathology. Behavior Modification. 2010;34:175–190. doi: 10.1177/0145445510363472. [DOI] [PubMed] [Google Scholar]
- 42.Goldschmidt AB, Engel SG, Wonderlich SA, Crosby RD, Peterson CB, Le Grange D, et al. Momentary affect surrounding loss of control and overeating in obese adults with and without binge eating disorder. Obesity. 2012;20:1206–1211. doi: 10.1038/oby.2011.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Telch CF, Pratt EM, Niego SH. Obese women with binge eating disorder define the term binge. International Journal of Eating Disorders. 1993;24:313–317. doi: 10.1002/(sici)1098-108x(199811)24:3<313::aid-eat9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]