Abstract
Torsion of the vermiform appendix is a rare disorder that causes symptoms similar to those of acute appendicitis. Primary and secondary causes of appendiceal torsion have been reported in the literature. Laparoscopy appears to be the most appropriate modality for diagnosis and treatment where the condition is suspected. To our knowledge this is the first case of appendiceal torsion in an adult causing right upper quadrant pain related to caecal malposition.
Background
Torsion of the vermiform appendix is a rare disorder that causes symptoms similar to those of acute appendicitis. Primary and secondary causes of appendiceal torsion have been reported in the literature. In 1918, Payne1 reported the first case of appendiceal torsion. Since then about 34 have been described in the adult population and another 16 in the paediatric population.2 Diagnosis of the torsion is invariably made intraoperatively. To our knowledge this is the first case of appendiceal torsion in an adult causing right upper quadrant pain related to caecal malposition.
Case presentation
A 52-year-old active athletic woman was referred by her general practitioner because of a 3-day history of upper abdominal pain; during the last day was localised more on the right upper quadrant pain and radiated to the back. She suffered a similar episode 2 weeks before that resolved spontaneously. She had had a left laparoscopic oophorectomy 11 years previously for a large cyst. On clinical examination she was an overweight lady with no temperature or tachycardia. On abdominal examination she was tender over the epigastrium and the right side of the abdomen. Murphy's sign was also positive. No hernias or masses were palpable. On per rectal examination there was hard stool on the rectum but no blood and no evidence of masses.
Investigations
White cell count was raised at 16×109/litre (4–10×109), C reactive protein was 16.8 mg/l (0–4) and urinalysis was normal. Abdominal x-ray was unremarkable and abdominal ultrasound showed a normal gallbladder but was unable to visualise the appendix. The patient was admitted for observation and was started on intravenous analgesia. During the following 12 h the pain increased in intensity and the patient was transferred to theatres for diagnostic laparoscopy.
Differential diagnosis
Acute appendicitis, biliary colic and acute cholecystitis.
Treatment
Three ports were inserted (umbilicus, right upper quadrant and suprapubically). On exploration the appendix was found to be gangrenous and lie subhepatically. It was 9 cm long with a 540° of anticlockwise rotation of a narrow, necrotic mesentery (figures 1 and 2). A small amount of serosanguinous fluid but no pus was found. The appendix was mobilised and resected between polydioxanone (PDS) endoloops.
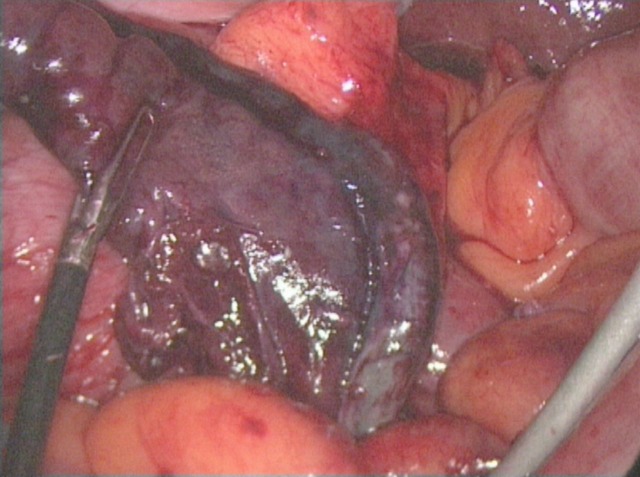
Figure 1.
View from the umbilical port. Gangrenous, rotated appendix. Liver edge can be seen at the top right of the picture suggesting the high position of the appendix.
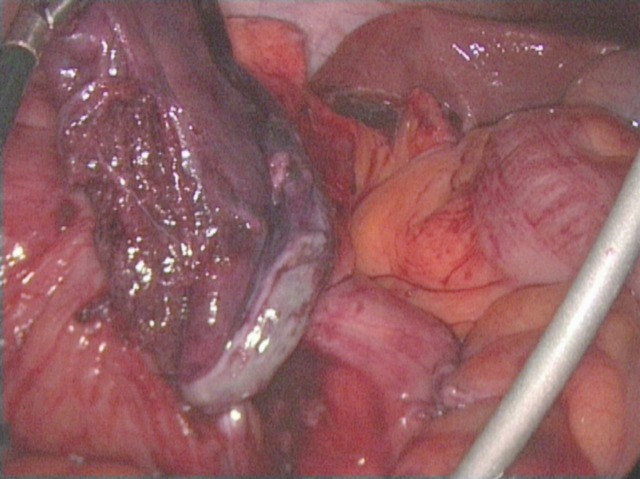
Figure 2.
Gangrenous appendix with 540° of anticlockwise rotation along its base.
Outcome and follow-up
Histology revealed a necrotic acutely inflamed appendix with overlying serositis. There was no evidence of neoplasia. The postoperative period was uneventful and the patient was discharged home the day after the operation. Her 6 weeks postoperative outpatient review confirmed full recovery.
Discussion
The appendix is a vestigial organ situated on the postero-medial aspect of the caecum, 2.5 cm below the ileocecal valve. Its mean length is 6.5 cm.3 Acute appendicitis is thought to occur in association with obstruction of the appendiceal wall (most often due to fecalith or lymphoid hyperplasia).4 While appendicitis is the most common intra-abdominal surgical emergency, torsion of the vermiform appendix is rare. Payne in 19181 was the first to describe a case of a torted appendix. In reviewing the English literature a total of 30 cases have been reported in adults, including our case (see table 1). Another 16 cases have been reported in paediatric patients.2 A review of the adult cases reveals that this condition affects both genders in similar proportion (18 women vs 16 men) and the age ranges at presentation from 18 to 78 with a mean of 40.8 years. The condition in its presentation is indistinguishable from acute appendicitis and is invariably diagnosed intraoperatively.5 The site of the torsion varies but most often is found within a centimetre from the base of the appendix.4 5 The location of the appendix also varies but most commonly it is freely lying or pelvis.4 6 An abnormally long appendix was noted in most studies (mean length: 9.6 cm). In the majority of cases the rotation occurs in an anticlockwise manner ranging from 180 to 1260°7–9 with a mean of 532. It is worth noting that even a slight rotation (180°) can compromise significantly vascular supply.
Table 1.
Appendiceal torsion in adults
| Author | Year | Age-sex | Presenting symptoms investigations (CT, USS) | Degree of torsion, mean 532° | Length (cm), mean 9.6 |
|---|---|---|---|---|---|
| Payne JE | 1918 | 37-F | RIF pain, N/V, no USS/CT | 1080 | 7 |
| Bevers EC | 1920 | 35-F | RIF pain, N/V, fever, no USS/CT | 720 | 7.6 |
| McFadden GDF | 1926 | NR-M | RIF pain, N/V, fever, no USS/CT | 180 | 12.7 |
| Flatley G | 1936 | 22-F | RIF pain, N/V, fever, no USS/CT | 900 | 10.8 |
| Hughes M | 1949 | 25-M | Generalised abdominal pain, N/V, no USS/CT | N/R | N/R |
| Dickson DR | 1953 | 60-F | RIF pain, N/V, no USS/CT | 720 | 11.5 |
| Cassie GF | 1953 | 25-M | Pain, nausea, no USS/CT | 720 | 11 |
| Chan KP | 1965 | 18-F | RIF pain, no USS/CT | 1260 | 10 |
| Ghent WR | 1966 | 21-M | RIF pain, N/V, fever, no USS/CT | 450 | N/R |
| De Bruin AJ | 1969 | 28-F | Pain, fever, no USS/CT | 360 | 10.5 |
| Killam AR | 1969 | 47-M | RIF pain, N/V, fever, no USS/CT | N/R | 7 |
| Legg NGM | 1973 | 29-M | Pain, fever, no USS/CT | 360 | 10 |
| Finch DRA | 1974 | 38-F | RIF pain, N/V, fever, no USS/CT | 360 | N/R |
| Won OH | 1977 | 35-M | RIF pain, N/V, fever, no USS/CT | N/R | 12 |
| Petersen KR | 1982 | 59-F | Pain, N/V, no USS/CT | 540 | 10 |
| Abu Zidan FM | 1992 | 32-F | RIF pain, USS: non-diagnostic | N/R | N/R |
| Tzilinis A | 2002 | 44-M | RIF pain, N/V, fever, no USS/CT | 540 | 5.5 |
| Moten AL | 2002 | 44-F | RIF pain, no USS/CT | 360 | N/R |
| Khattak S | 2003 | 35-M | RIF pain, N/V, anorexia, no USS/CT | N/R | N/R |
| Bestman TJR | 2006 | 35-F | RIF pain, nausea, USS: non-diagnostic | N/R | 7.5 |
| Bowling BC | 2006 | NR-F | RIF pain, N/V, CT: non-diagnostic | N/R | 8 |
| Rajendran N | 2006 | 29-F | RIF pain, anorexia, no USS/CT | 360 | 11 |
| Hamada T | 2007 | 79-M | RIF pain, USS: diagnostic | 180 | N/R |
| Kitagawa M | 2007 | 34-M | RIF pain, CT: non-diagnostic | 180 | 10 |
| Suggala S | 2008 | 18-M | RIF pain, N/V, anorexia, fever, no USS/CT | 270 | 8 |
| Salim OEF | 2008 | 29-M | RIF pain, anorexia, no USS/CT | N/R | 12 |
| Wani I | 2008 | 76-M | RIF pain, nausea, no USS/CT | 540 | 10 |
| Wani I | 2010 | 38-F | RIF pain, N/V, anorexia, fever, CT: non-diagnostic | 180 | 20 |
| Lee CH | 2011 | 78-F | RIF pain, N/V, fever, CT: non-diagnostic | 900 | 10.5 |
| Present study | 52-F | RUQ pain, no USS/CT | 540 | 9 | |
F, female; M, male; NR, normal; RIF, right iliac fossa; RUQ, right upper quadrant; USS, ultrasound.
Both primary and secondary torsions of the appendix have been reported below.
Primary torsion of the appendix: This occurs without a known cause. Suggested predisposing factors include anatomic variations such as (1) long, fan-shaped meso-appendix with a narrow base; (2) the absence of azygotic folds that normally laterally fix the appendix and (3) caecal malposition. In addition, the use of laxatives and vigorous physical exercise or abnormal peristaltic bowel movements have been suggested to predispose to appendiceal torsion.2 10–12 It is interesting to note that in our case there was a caecal malposition, a long appendix and a history of vigorous physical exercise.
Secondary torsion of the appendix: This is much rarer with only 18 reported cases in the English literature to date.8 It occurs in association with a mucocele, intussusception, lipoma, cystadenoma, adhesions and inflammation causing distention, instability and a tendancyto twist.4 13–15 Carcinoid tumour and infestation with parasites such as Schistosoma haematobium may also rarely lead to torsion of the appendix.16 17
In the literature, this condition is rarely identified on preoperative imaging. Apart from one case,18 ultrasound scanning has failed to visualise as a torted appendix in any of the cases where the diagnosis was made at operation. In that unique case, sonography showed a target-like appearance at the base of the appendix (similar to that in cases of ovarian or testicular torsion); this is also known as ‘whirlpool sign’.18 CT can show signs of appendicular pathology but has never been reported to give the diagnosis of appendiceal torsion. It may identify a primary pathology of the appendix such as a mucocele or cystadenoma.3 8 Laparoscopy is therefore best at identifying and treating this condition.
It has been suggested that a chronic intermittent epigastric pain, which is not related to meals and relieved not by antacids but by belching, may represent a reflux dysfunction of the gastrointestinal tract associated with a long-standing mucocele of the appendix. A consequent torsion of the enlarged organ will give symptoms similar to those of acute appendicitis.15 Also, as with torsion of any organ, self-untwisting may happen at any point. This can explain some of the cases where the patient presents with symptoms of acute appendicitis but a normal appendix is encountered and no other pathology is found during the operation.4 5
Caecal malposition is not rare; 6% of the population is reported to have an undescended caecum.2 Subhepatic appendicitis is a recognised clinical entity.19–21
Subhepatic appendiceal torsion has only been described once in a child2 but never in an adult. The clinical diagnosis in these cases is difficult because the presentation is not typical for acute appendiceal pathology. The delay in diagnosis and treatment results in a necrotic perforated appendix. In our case the abdominal ultrasound excluded our initial diagnosis of cholecyctitis or biliary colic. Appendicitis should be among our differential diagnosis when characteristic signs and symptoms are present, even if the location of abdominal pain is not typical.
Learning points
Appendiceal torsion is extremely rare with only a few case reports in the literature and is invariably diagnosed intraoperatively.
Appendiceal torsion can be either primary or secondary.
Preoperative imaging is very rarely diagnostic of the condition (only one case report in the literature).
Self-untwisting of the appendix can explain some of the cases where the patient presents with symptoms of acute appendicitis but a normal appendix is encountered during the operation.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Payne J. A case of torsion of the appendix. Br J Surg 1918;6:327. [Google Scholar]
- 2.Montes-Tapia F, Quiroga-Garza A, Abrego-Moya V. Primary torsion of the vermiform appendix and undescended cecum treated by video-assisted transumbilical appendectomy. J Laparoendosc Adv Surg Tech A 2009;19:839–41. [DOI] [PubMed] [Google Scholar]
- 3.Kitagawa M, Kotani T, Yamano T, et al. Secondary torsion of vermiform appendix with mucinous cystadenoma. Case Rep Gastroenterol 2007;1:32–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tzilinis A, Vahedi MH, Wittenborn WS. Appendiceal torsion in an adult: case report and review of the literature. Curr Surg 2002;59:410–11. [DOI] [PubMed] [Google Scholar]
- 5.Merrett ND, Lubowski DZ, King DW. Torsion of the vermiform appendix: a case report and review of literature. Aust N Z J Surg 1992;62:981–3. [DOI] [PubMed] [Google Scholar]
- 6.Gopal K, Kumar S, Grewal H. Torsion of the vermiform appendix. J Pediatr Surg 2005;40:446–7. [DOI] [PubMed] [Google Scholar]
- 7.McFadden GDF. Torsion of the meso-appendix associated with gangrene of the appendix. Br Med J 1926;2:1223. [Google Scholar]
- 8.Lee CH, Lee MR, Kim JC, et al. Torsion of a mucocele of the vermiform appendix: a case report and review of the literature. J Korean Surg Soc 2011;81:s47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Val-Bernal JF, Gonzalez-Vela C, Garijo MF. Primary acute torsion of the vermiform appendix. Pediatr Pathol Lab Med 1996;16:655–61. [PubMed] [Google Scholar]
- 10.Bowling CB, Lipscomb GH. Torsion of the appendix mimicking ovarian torsion. Obstet Gynecol 2006;107(2 Pt 2):466–7. [DOI] [PubMed] [Google Scholar]
- 11.Moten AL, Williams RS. Torsion of the appendix. Med J Aust 2002;177:632. [DOI] [PubMed] [Google Scholar]
- 12.Rajendran N, Ameen S, Rohatgi A. Laparoscopic management of a torted appendix. Ann R Coll Surg Engl 2006;88:W6–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wani I, Maqbool M, Sheikh T. Secondary torsion of vermiform appendix. J Emerg Trauma Shock 2010;3:206–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suggala S, Gopi E, Sreejayan M. Torsion of vermiform appendix: a case report. Internet J Surg 2008;17(2). doi:10.5580/1efb. [Google Scholar]
- 15.Chan KP. Volvulus complicating mucocele of the appendix. Br J Surg 1965;52:713–14. [DOI] [PubMed] [Google Scholar]
- 16.Hughes M. A case of bilharzia of the appendix, with strangulation of ileum. Br J Surg 1949;36:428. [DOI] [PubMed] [Google Scholar]
- 17.Cassie GF. Torsion of mucocele of the appendix caused by a carcinoid tumour. Br J Surg 1953;41:105–6. [DOI] [PubMed] [Google Scholar]
- 18.Hamada T, Kosaka K, Shigeoka N, et al. Torsion of the appendix secondary to appendiceal mucocele: gray scale and contrast-enhanced sonographic findings. J Ultrasound Med 2007;26:111–15. [DOI] [PubMed] [Google Scholar]
- 19.Scott KJ, Sacks AJ, Goldschmidt RP. Subhepatic appendicitis. Am J Gastroenterol 1993;88:1773–4. [PubMed] [Google Scholar]
- 20.Kulvatunyou N, Schein M. Perforated subhepatic appendicitis in the laparoscopic era. Surg Endosc 2001;15:769. [DOI] [PubMed] [Google Scholar]
- 21.Palanivelu C, Rangarajan M, John SJ, et al. Laparoscopic appendectomy for appendicitis in uncommon situations: the advantages of a tailored approach. Singapore Med J 2007;48:737–40. [PubMed] [Google Scholar]