Abstract
Cogan's syndrome or non-syphilitic interstitial keratitis with vestibule-auditory dysfunction is a serious and under-recognised complication of rheumatoid arthritis. It is an autoimmune condition characterised by inflammatory infiltrates on the cornea and extensive vestibulocochlear damage. If left untreated, patients progress to develop profound hearing loss. We present a case that was incorrectly diagnosed and treated as conjunctivitis by several emergency departments prior to being correctly recognised as Cogan's syndrome.
Background
Cogan's syndrome is a rare condition that can lead to deafness and blindness. Patients are often misdiagnosed with conjunctivitis and discharged from emergency departments. It is important to increase recognition of this syndrome as the complications are potentially irreversible with devastating consequences. Intervention with steroids helps to reduce these risks.
Case presentation
A 63-year-old Caucasian woman with a 20-year history of rheumatoid arthritis treated with hydroxychloroquine and azathioprine was reviewed in clinic with red eyes, difficulty hearing, associated headaches and rotational vertigo. Her symptoms had started 6 weeks earlier, initially with a pruritic left eye that subsequently became erythematous. Subsequently, both eyes became inflamed and she complained of hearing loss with rotational vertigo. She had sought advice from the emergency department on three occasions, however, was discharged with topical antibiotic and steroid eye drops based on a suspected diagnosis of conjunctivitis. On examination in the clinic, she was unable to walk without support. Bilateral red eyes (figure 1) were noted with normal fundoscopy and neurological examination. Severe sensorineural hearing loss was noted as elicited by Rinne's and Weber's test.
Figure 1.
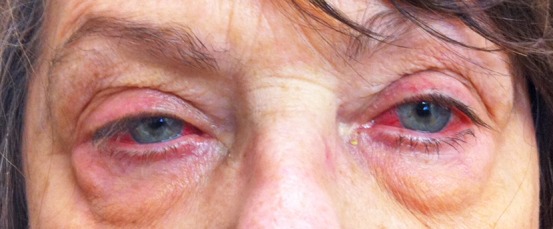
Bilateral interstitial keratitis in patient with Cogan's syndrome.
Investigations
Blood tests showed a C reactive protein of 9 mg/dl, but an erythrocyte sedimentation rate of 40 mm/h. All other bloods were normal, including an anti-neutrophil cytoplasmic antibody (ANCA). Severe sensorineural loss was confirmed using audiometry but MRI was unremarkable.
Differential diagnosis
Painful red eye
Acute glaucoma
Corneal infections
Iritis
Painless red eye
Conjunctivitis
Episcleritis
Subconjunctival haemorrhage
Treatment
High dose oral prednisolone was initiated at a dose of 60 mg once daily.
Outcome and follow-up
Based on these clinical features and a negative syphilis serology, a diagnosis of Cogan's syndrome was made and treated with immediate initiation of steroids. Her ocular symptoms resolved within a week, however, she was left with severe sensorineural hearing loss despite therapy.
Discussion
Cogan's syndrome is a rare multisystem autoimmune condition described in 1945 by ophthalmologist David Glendenning Cogan at the Massachusett's eye and ear infirmary.1 Cogan's syndrome is associated with rheumatoid arthritis but has also been linked to polyarteritis nodosa, Grave's disease and ulcerative colitis. It predominantly affects young to middle-aged Caucasian adults and there have been less than 200 cases described in the literature. There is often a precipitant and patients report a preceding upper respiratory tract infection or pneumonia in 23% of cases. As such, it is hypothesised that an infective stimulus results in the onset of this autoimmune condition in some patients although this is not consistent. There is thought to be an association with Chlamydia pneumoniae due to an increased incidence in sufferers of this particular bacterial pneumonia, however, the overwhelming majority of patients with C pneumoniae do not develop Cogan's syndrome.
The initial symptom may involve the eye (41%), the ear (43%) or other constitutional symptoms such as weight loss, arthralgia, myalgia or fevers. Combined severe vestibule-auditory and ophthalmological dysfunction inevitably occur within a few days to weeks of initial disease manifestation.2 3
These features include interstitial keratitis with associated conjunctivitis, iritis or conjunctival haemorrhage and sensorineural hearing loss, vertigo or tinnitus. Severe complications are common and 15% of patients develop aortic incompetence that requires valve replacement, 25% central neurological signs including hemiplegia and aphasia and 13% develop a vasculitis that can involve iliac or mesenteric vessels.4 5
Blood results are usually non-diagnostic and are not specific. Patients may have leucocytosis, anaemia, thrombocytosis or raised inflammatory markers although none of these are discriminatory. Autoantibodies are usually negative.6 High dose systemic corticosteroid treatment should be initiated early and 82% of patients have a favourable response. Case series have also reported on the efficacy of methotrexate, cyclophosphamide and infliximab.7 Sixty-two per cent of patients have multiple disease relapses, usually affecting the eyes.
In summary, Cogan's syndrome is a rare complication of rheumatoid arthritis that is often overlooked. The syndrome is characterised by ocular and audiovestibular manifestations, though systemic involvement is frequent and severe. In some cases, autoantibodies have been detected which bind to the antigens on sensory epithelia of the inner ear or on the eye.8 A review of the literature notes the importance of early administration of high-dose corticosteroids. In patients treated early with mild auditory impairment, some improvement can be obtained. However, in patients with complete hearing loss, rates of recovery are low and the only hope of restoring function is with a cochlear implant.
Learning points.
Hearing loss and interstitial keratitis in patients with rheumatoid arthritis should prompt the clinician to think of Cogan's syndrome.
Early treatment with high-dose steroids is imperative to prevent long-term complications.
Always discuss with a rheumatologist if uncertainty exists.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Cogan DG, Dickersin GR. Non-syphilitic interstitial keratitis with vestibulo-auditory symptoms—a case with fatal aortitis. Trans Am Ophthalmol Soc 1963;61:113–21. [PMC free article] [PubMed] [Google Scholar]
- 2.Greco A, Gallo A, Fusconi M, et al. Cogan's syndrome: an autoimmune inner ear disease. Autoimmun Rev 2012. (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 3.Murphy G, Sullivan MO, Shanahan F, et al. Cogan's syndrome: present and future directions. Rheumatol Int 2009;29:1117–21. [DOI] [PubMed] [Google Scholar]
- 4.Vinceneux P. Cogan's syndrome. Orphanet (Internet). http://www.orpha.net/data/patho/Pro/en/Cogan-FRenPro3333.pdf (accessed February 2005).
- 5.Gluth MB, Baratz KH, Matteson EL, et al. Cogan syndrome a retrospective review of 60 patients throughout a half century. Mayo Clin Proc 2006;81:483–8. [DOI] [PubMed] [Google Scholar]
- 6.Grasland A, Pouchot J, Hachulla E, et al. Typical and atypical Cogan's syndrome: 32 cases and review of the literature. Rheumatology 2004;43:1007–15. [DOI] [PubMed] [Google Scholar]
- 7.Fricker M, Baumann A, Wermelinger F, et al. A novel therapeutic option in Cogan diseases? TNF-α blockers. Rheumatol Int 2006;27:493–5. [DOI] [PubMed] [Google Scholar]
- 8.Lunardi C, Bason C, Leandri M, et al. Autoantibodies to inner ear and endothelial antigens in Cogan's Syndrome. Lancet 2002;360:915. [DOI] [PubMed] [Google Scholar]


