Abstract
A 78-year-old woman presented 28 days after a low-impact fall, where she sustained a right pubic ramus fracture, with increasing left hip pain and fever. Her blood results showed a high white cell count and deranged urea and electrolytes. An MRI revealed multiple osteoporotic fractures and bilateral gluteal abscesses with left iliopsoas abscess, which had likely formed in a haematoma of a sacral fracture. She received a long course of intravenous antibiotics and CT-guided drainage of the abscesses. She developed symptoms of cauda equina, but no evidence of epidural extension of the abscess was found at operation. She required neurorehabilitation. This case highlights the complications of pelvic osteoporotic fractures, and high associated morbidity and mortality in the elderly population.
Background
Pelvic osteoporotic fractures (POFs) can occur when minimal trauma is applied to abnormal bone with deficient elastic resistance or mineral content.1 Incidence is increasing.2 They mostly affect the elderly population and have a high associated morbidity and mortality. We present a patient with an unusual complication of this condition.
Case presentation
A 78-year-old woman was admitted to the emergency department (ED) after slipping on ice onto concrete, hurting her right arm and hip. She otherwise felt well. She had a medical history of hypertension and adenocarcinoma of the lung, for which she had had a right upper lobectomy 7 years prior. Examination was normal including normal range of movement of her right hip with no bony tenderness. Her blood results were all within normal range and she was apyrexial. A radiograph was suspicious of right pubic ramus fracture. She was admitted for analgesia and physiotherapy, and discharged 2 days later with community physiotherapy and zimmer frame (figure 1).
Figure 1.
The plain radiograph at first presentation, showing no fractures.
Twenty-six days after discharge she was readmitted to ED with increasing left groin and thigh pain. She was now unable to weight-bear. She had a temperature of 38.2°C, heart rate of 100 bpm and blood pressure of 125/69 mm Hg. Examination of her cardiorespiratory system was normal. Abdominal examination revealed mild left iliac fossa pain. Her left leg was neurovascularly intact with no obvious deformity, but she had decreased range of hip motion with all movements due to pain.
Investigations
Her white cell count (WCC) was 22.2×109/litre, with a raised urea (14.2 mmol/l) and creatinine (130 μmol/l), but low sodium (129 mmol/l). Other blood tests were normal. Blood cultures were sent and later grew penicillin-resistant Staphylococcus aureus. An MRI was organised from ED, but performed the next day when she was admitted to the ward (figure 2).
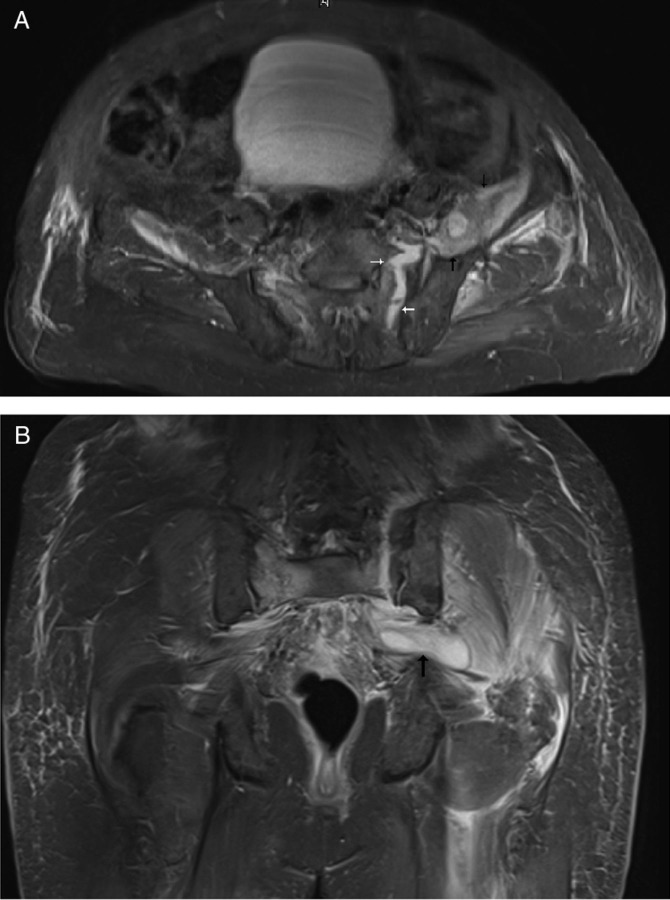
Figure 2.
(A) Axial view and (B) coronal view T1 MRI slice demonstrating a left sacral fracture containing fluid (white arrows), with abscess extending along the left iliopsoas muscle (black arrows) and oedema within the left glutei.
Differential diagnosis
Urinary tract infection was considered, based on the deranged urea and electrolytes with raised WCC and left iliac fossa pain. Also considered was septic left hip joint, although there was no swelling or erythema. She was seen by an orthopaedic senior house officer, who considered psoas abscess. MRI confirmed this, showing multiloculated collections in the gluteus muscles and iliopsoas, in communication with a fracture in the left sacrum, therefore likely an infected haematoma. It showed multiple osteoporotic fractures—in the right acetabulum, bilateral ischial rami, right sacrum and left pubic ramus.
Treatment
The collections consisted of too many small loculations to drain percutaneously at that time, so she was treated with intravenous co-amoxiclav until the blood culture results were known the next day, when she was started on 2 g of intravenous flucloxacillin four times a day, 7 days later rifampicin was added. She was started on regular oxycontin and oxynorm when required by the Acute Pain Team.
On day 2 of her admission she went into urinary retention and had constipation, which was attributed to the morphine use. On day 9 she had back pain with faecal incontinence. Digital rectal examination revealed poor anal tone. She underwent MRI and was reviewed by the neurosurgeons who were concerned about an epidural collection posterior to the L3 and L4 vertebral bodies, which could represent epidural extension of the abscesses. She underwent L3 and L4 laminectomy the next day. No infective material was found, but epidural fat was removed. Postoperatively her back pain and power in her legs improved to 4/5, but urinary retention remained.
After 16 days she was converted to oral flucloxacillin, with CT-guided drainage being performed on day 28. The left iliopsoas abscess was aspirated to dryness (12 ml) and the left gluteal abscess had a drain inserted (30 ml aspirated).
Outcome and follow-up
This lady was discharged to a neurorehabilitation unit. She was hospitalised for a total of 98 days. Subsequent bone mineral densitometry showed osteoporosis. At follow-up nearly a year after the original fall she was walking with one stick, was catheterised but continent of faeces.
Discussion
POFs can occur after low-impact trauma in those whose bones are of decreased density. The most common sites of POFs include the pubic rami, sacrum, ilium and acetabulum.3 There is often more than one fracture.4
They are associated with high in-hospital mortality (104–14%5) and complication rates (20% to 50%6), as well as long average admission time (185 to 454 days). Many patients do not return to their premorbid independence.7 It is hypothesised that the type of injury after low-energy trauma is less important than pre-existing comorbidities, and that it is the clinical complexity of those patients that is responsible for poor outcomes.8
Iliopsoas abscess is relatively uncommon with an annual worldwide incidence of 12 cases per year. The incidence is increasing, due to improving diagnostic imaging.9 It may be primary with no focus of infection, or secondary, as a result of direct spread from adjacent structures. The majority are due to infections by S aureus.10 There is a significant mortality, and secondary abscesses carry a mortality of 18.9%.11
To our knowledge, this is the first report of psoas abscess secondary to osteoporotic fracture, and it is important to demonstrate the varied complications of this condition.
Learning points/take home messages.
Osteoporotic fractures have a high morbidity and mortality, and so efforts should be made to prevent their occurrence.
Osteoporotic fractures are not easily seen and diagnosed on plain radiographs, and may need further imaging.
Psoas abscess should be suspected in those patients with pelvic fractures and deterioration with fever.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Kannus P, Palvanen M, Parkkari J, et al. Osteoporotic pelvic fractures in elderly women. Osteoporos Int 2005;16:1304–5. [DOI] [PubMed] [Google Scholar]
- 2.Krappinger D, Struve P, Schmid R, et al. Fractures of the pubic rami: a retrospective review of 534 cases. Arch Orthop Trauma Surg 2009;129:1685–90. [DOI] [PubMed] [Google Scholar]
- 3.Alost T, Waldrop RD. Profile of geriatric pelvic fractures presenting to the emergency department. Am J Emerg Med 1997;15:576–8. [DOI] [PubMed] [Google Scholar]
- 4.Alnaib M, Waters S, Shanshal Y, et al. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthopaed Traumatol 2012;12:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spencer JD, Lalanadham T. The mortality of patients with minor fractures of the pelvis. Injury 1985;16:321–3. [DOI] [PubMed] [Google Scholar]
- 6.Breuil V, Roux CH, Testa J, et al. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Joint Bone Spine 2008;75:585–8. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk WA, Poeze M, van Helden SH, et al. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury 2010;41:411–14. [DOI] [PubMed] [Google Scholar]
- 8.Shortt NL, Robinson CM. Mortality after low-energy fractures in patients aged at least 45 years old. J Orthop Trauma 2005;19:396–400. [DOI] [PubMed] [Google Scholar]
- 9.Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol 1992;147:1624–6. [DOI] [PubMed] [Google Scholar]
- 10.Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: world-wide variation in aetiology. World J Surg 1986;10:834–43. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg BO, Hedges JR, Stewart DW. Psoas abscess. J Emerg Med 1984;1:533–7. [DOI] [PubMed] [Google Scholar]