Abstract
We reported two cases of hepatocellular carcinoma (HCC) with lung metastases who were treated with a combination of thalidomide and cyproheptadine. The use of cyproheptadine in these two cases was originally for skin itching. Follow-up CT images revealed a complete remission of HCC in both of them after treatment for 6 months and 6 weeks, respectively. A following experimental cell line study demonstrated that cyproheptadine effectively reduced the viability of two HCC cell lines.
Background
Hepatocellular carcinoma (HCC) is a leading cause of cancer deaths in Taiwan for the past two decades.1 However, current treatment for advanced HCC is still not satisfactory,2 even with the treatment of target therapy3 or thalidomide.4 HCC is a hypervascular tumour with overexpression of angiogenic factors such as vascular endothelial growth factor.5 Thalidomide is an antineoplastic agent with antiangiogenic properties.5 In a study involving 45 patients, treating with thalidomide alone, complete response was not observed in any patient and partial response was observed in only 5% patients.4
Case presentation
Case 1
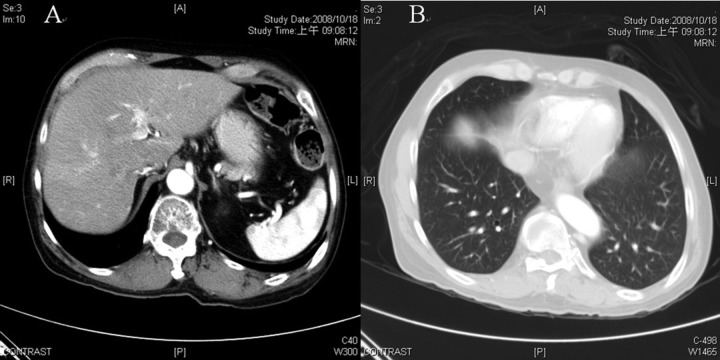
A 57-year-old man with no history of alcohol consumption was diagnosed with chronic hepatitis C. On 26 November 2007, abdominal CT revealed a contrast-enhanced tumour measuring 3 cm in diameter near the dome of the right lobe of liver, and angiography revealed characteristic neovascularity and tumour stain. Serum α-fetoprotein level was 5.4 ng/ml (normal range 0–20 ng/ml). Consequently, a diagnosis of HCC was made on the basis of the criteria in the American Association for the Study of Liver Diseases guidelines.2 He underwent transarterial chemoembolisation for HCC on 3 December 2007. Four months later, abdominal CT performed on 16 April 2008 (figure 1A,B) revealed that the tumour size increased to 10 cm in diameter, with the presence of lung metastasis. The portal vein and its branches were patent and CT images did not reveal cirrhosis or ascites. Physical examination did not reveal any remarkable finding. Because the patient had advanced HCC at Barcelona Clinic Liver Cancer stage C, we treated him with thalidomide (50 mg once daily) for 14 days, followed by thalidomide (50 mg twice daily) for 67 days. At the same time, we prescribed cyproheptadine (4 mg thrice daily) for his skin itching. Eighty-one days later, thalidomide was discontinued because the patient could not afford it, but cyproheptadine was continued. Abdominal CT on 18 October 2008 revealed complete remission of the liver tumour and lung metastasis (figure 2A,B).
Figure 1.
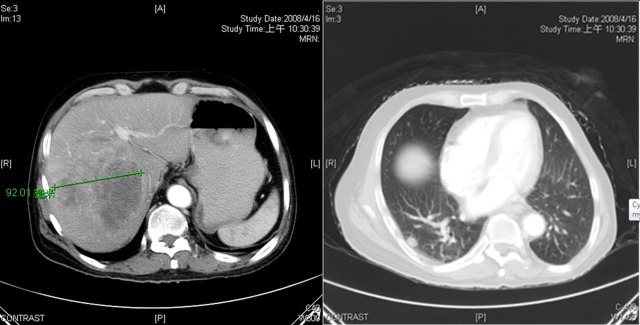
CT of case 1 on 16 April 2008. (A) Hepatocellular carcinoma approximately 10 cm in diameter with daughter nodules. (B) Metastasis in the right lung. (In fact, bilateral lung metastases were observed).
Figure 2.
CT of case 1 on 18 October 2008. (A) Complete remission of large hepatocellular carcinoma. (B) Disappearance of lung metastasis.
Case 2
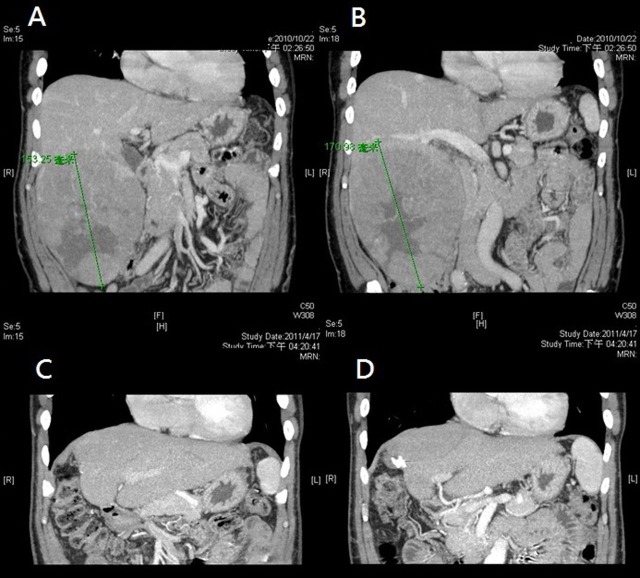
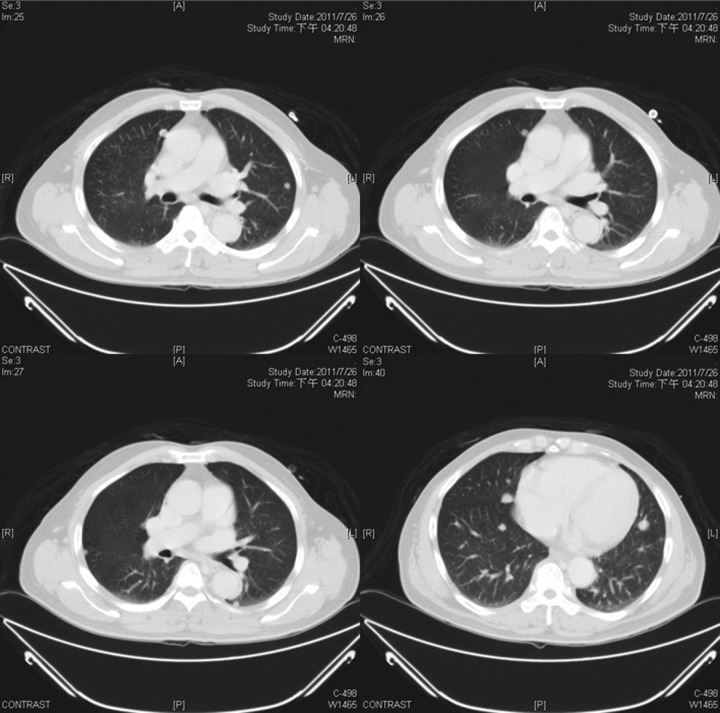
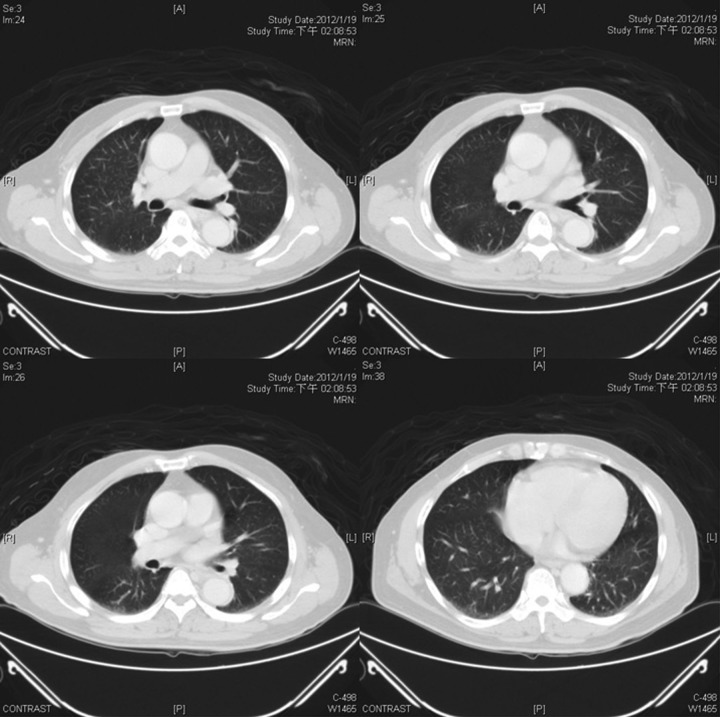
A 63-year-old man with no history of alcohol consumption was diagnosed with chronic hepatitis B and hepatitis C for years. The whole abdomen CT performed on 22 October 2010 (figure 3A,B) showed a large liver tumour about 17 cm in diameter, which was resected on 3 November 2010. Pathological analyses confirmed HCC without cirrhosis, stage T3N0Mx. The serum α-fetoprotein (AFP) level before surgery was 48 203 ng/ml, and decreased to 25.6 ng/ml on 27 December 2010. The whole abdomen CT performed on 17 April 2011 revealed no obvious liver tumour recurrence (figure 3C,D). However, the chest CT performed on 17 April 2011 revealed bilateral lung metastases, and the serum AFP level was up to 30.2 ng/ml. Subsequent chest CT performed on 26 July 2011 revealed progression of lung metastases (figure 4). The patient underwent six chemotherapy cycles with epirubicin at the oncology department; however, the response was poor and his serum AFP level increased to 122 ng/ml on 21 November 2011. Later, we gave him the thalidomide (50 mg once daily) from 2 December 2011. Cyproheptadine (2 mg thrice daily) was also prescribed for skin itching. The serum AFP level on 13 January 2012 was decreased to 5.5 ng/ml and the follow-up chest CT performed on 19 January 2012 revealed that bilateral lung metastases totally disappeared (figure 5).
Figure 3.
Liver CT (coronal sections) of case 2. (A and B) CT performed on 22 October 2010 before surgery, revealed a large tumour mass about 17 cm in diameter in the right lobe of the liver. (C and D) CT performed on 17 April 2011 after surgery, showed no obvious liver tumour.
Figure 4.
Chest CT of case 2 on 26 July 2011. Bilateral lung metastases were observed before treatment with thalidomide and cyproheptadine.
Figure 5.
Chest CT of case 2 on 19 January 2012. Complete remission of lung metastasis after treatment with thalidomide and cyproheptadine
Two patients did not take any Chinese herbs and had no other major systemic disease such as hypertension or diabetes mellitus.
Investigations
In order to test the cytotoxicity of cyproheptadine on HCC, in vitro cell viability assay was performed. Two HCC cell lines, HepG2 and Huh-7, were treated with various concentrations of cyproheptadine, and cell viability was measured by the Cell Counting Kit-8 (CCK-8) after 24 and 48 h of incubation. Because we used dimethyl sulfoxide (DMSO)-dissolved cyproheptadine, cells cultured in the media supplemented with an equivalent volume of DMSO (0.3%) were used as controls to ensure DMSO not to cause unwanted effects. A previous study showed that this concentration of DMSO had no significant effect on the growth and survival of HepG2 and Huh-7 cells.6 The results demonstrated that cyproheptadine reduced cell viability in a time-dependent and dose-dependent manner on both cell lines (figure 6). Consistent with previous study, treatment with only DMSO as a control did not alter HepG2 and Huh-7 cell proliferation (p>0.05).
Figure 6.
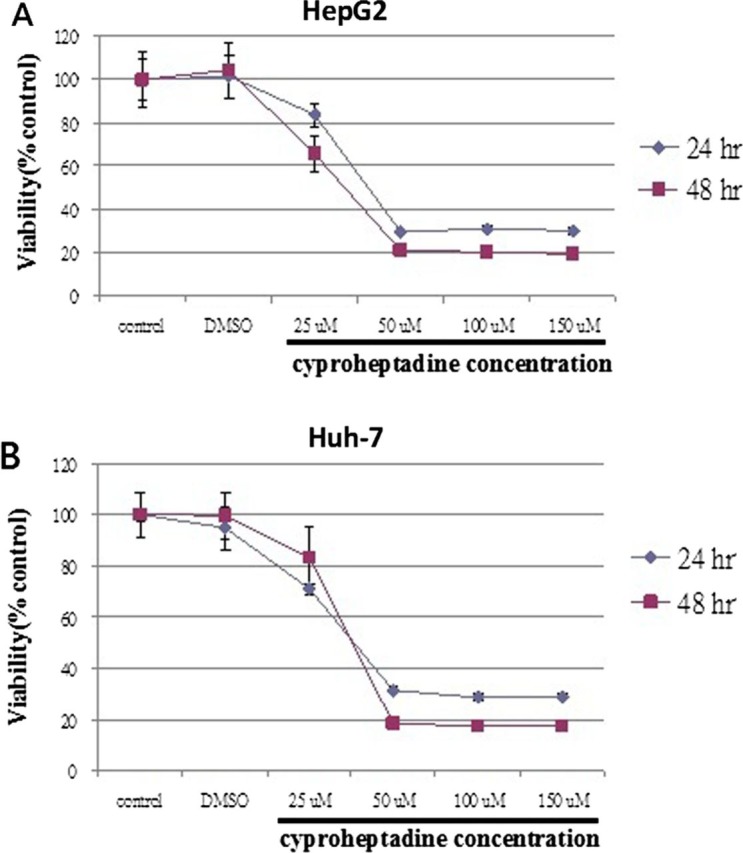
Cytotoxicity of cyproheptadine against hepatocellular carcinoma (HCC) cell lines, (A) HepG2 and (B) Huh-7. Cells were initially seeded at 1×104 cells per well in 96-well plates and cultured in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum for 24 h. Subsequently, cells were starved in medium supplemented with 2% FBS for 24 h, and then treated with various concentrations of cyproheptadine for 24 and 48 h. Cell viability was detected by Cell Counting Kit-8 assay. Data points are presented as mean±SD (n=6) in comparison with the mean of untreated controls. Cells cultured in medium supplemented with 10% FBS and 0.3% dimethyl sulfoxide were used as negative control. Treatment with cyproheptadine at each concentration tested significantly decreased survival in both HCC cell lines compared with corresponding untreated controls using a two-tailed Student's t test (p<0.05). A graphic representation of cell viability data showing dose–response and time–response curves after treatment with various concentrations of cyproheptadine.
Outcome and follow-up
The first case was initially followed up at our hospital regularly, and no recurrence was observed until 28 July 2009 when the last follow-up abdominal CT was performed. But he lost follow-up because he thought he was cured. Unfortunately, he expired on 13 December 2011 at other hospital due to HCC recurrence according to the statement of his families.
The second case continues taking both drugs and keeps asymptomatic until his last follow-up on 21 May 2012. The CT of whole abdomen and chest on 12 May 2012 showed no evidence of HCC recurrence and lung metastasis.
Discussion
Thalidomide is a treatment option for patients with advanced HCC, but its outcome is not satisfactory.4 Cyproheptadine is sometime used in our institute for HCC patients with skin itching. On the basis of these two cases, we accidentally found the outcomes of HCC patients treated with combination therapy (thalidomide and cyproheptadine) were more favourable than patients treated with thalidomide alone.
Cyproheptadine is a first-generation antihistaminic drug often used to treat allergies with few adverse effects. Cyproheptadine can also be used as an appetite stimulant in cancer patients in order to improve their appetite.7 In light of tumour inhibiting effects, three histamine H1-receptor antagonists, diphenhydramine,8 loratadine9 and chlorpheniramine,10 were reported for their inhibitory effects on acute lymphoblastic leukaemia cells,8 human colon carcinoma cell line (HT29)9 and human breast cancer cell line (MCF-7),10 respectively. However, no study has been done on the effectiveness of cyproheptadine for HCC. Our pilot cell line study showed that cyproheptadine has cytotoxic effect on HCC cell lines. Some studies using animal models and cancer cell lines have shown the inhibitory effect of cyproheptadine in myeloma, leukaemia11 and mantle cell lymphoma.12 The previous study by Mao et al11 showed that cyproheptadine inhibited the expression of cyclins D1, D2 and D3 and induced cell cycle arrest in G0/G1 phase followed by apoptosis in myeloma and leukaemia cell lines and primary patient samples preferentially over normal haematopoietic cells.
In addition, cyproheptadine is also a potent serotonin antagonist,13 which inhibits the binding of serotonin to its receptors, and is the drug of choice for serotonin syndrome.14 The human HCC cell lines Huh-7 and HepG2 have been used to assess the function of serotonin. Soll et al15 demonstrated that serotonin promotes the growth and survival of starved HCC cells. Serotonin is involved in the growth of HCC cells through downstream activation of mammalian target of rapamycin, and serotonin-related pathways may represent a new treatment strategy.15
Learning points.
The concomitant use of thalidomide and cyproheptadine may be a potential treatment for hepatocellular carcinoma (HCC).
The antihistamine cyproheptadine was found to have cytotoxicity on HCC cell lines in our in vitro experimental study.
More studies are needed to explore the mechanism and treatment effect of antihistamine on HCC and other malignant diseases.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Jan CF, Chen CJ, Chen HH. Causes of increased mortality from hepatocellular carcinoma in high incidence country: Taiwan experience. J Gastroenterol Hepatol 2005;20:521–6. [DOI] [PubMed] [Google Scholar]
- 2.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology 2005;42:1208–36. [DOI] [PubMed] [Google Scholar]
- 3.Llovet JM, Ricci S, Mazzaferro Vet al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–90. [DOI] [PubMed] [Google Scholar]
- 4.Yau T, Chan P, Wong Het al. Efficacy and tolerability of low-dose thalidomide as first-line systemic treatment of patients with advanced hepatocellular carcinoma. Oncology 2007;72:67–71. [DOI] [PubMed] [Google Scholar]
- 5.Yabu T, Tomimoto H, Taguchi Yet al. Thalidomide-induced antiangiogenic action is mediated by ceramide through depletion of VEGF receptors, and is antagonized by sphingosine-1-phosphate. Blood 2005;106:125–34. [DOI] [PubMed] [Google Scholar]
- 6.Baek JY, Hur W, Wang JS, et al. Selective COX-2 inhibitor, NS-398, suppresses cellular proliferation in human hepatocellular carcinoma cell lines via cell cycle arrest. World J Gastroenterol 2007;13:1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kardinal CG, Loprinzi CL, Schaid DJet al. A controlled trial of cyproheptadine in cancer patients with anorexia and/or cachexia. Cancer 1990;65:2657–62. [DOI] [PubMed] [Google Scholar]
- 8.Jangi SM, Asumendi A, Arlucea Jet al. Apoptosis of human T-cell acute lymphoblastic leukemia cells by diphenhydramine, an H1 histamine receptor antagonist. Oncol Res Featur Preclin Clin Cancer Ther, 14, 2004;7:363–72. [DOI] [PubMed] [Google Scholar]
- 9.Soule BP, Simone NL, DeGraff WG, et al. Loratadine dysregulates cell cycle progression and enhances the effect of radiation in human tumor cell lines. Radiat Oncol 2010;5:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medina MA, García de Veas R, Morata P, et al. Chlorpheniramine inhibits the synthesis of ornithine decarboxylase and the proliferation of human breast cancer cell lines. Breast Cancer Res Treat 1995;35:187–94. [DOI] [PubMed] [Google Scholar]
- 11.Mao X, Liang SB, Hurren Ret al. Cyproheptadine displays preclinical activity in myeloma and leukemia. Blood 2008;112:760–9. [DOI] [PubMed] [Google Scholar]
- 12.Paoluzzi L, Scotto L, Marchi E, et al. The anti-histaminic cyproheptadine synergizes the antineoplastic activity of bortezomib in mantle cell lymphoma through its effects as a histone deacetylase inhibitor. Br J Haematol 2009;146:656–9. [DOI] [PubMed] [Google Scholar]
- 13.Kapur S, Zipursky RB, Jones C, et al. Cyproheptadine: a potent in vivo serotonin antagonist. Am J Psychiatry 1997;154:884. [DOI] [PubMed] [Google Scholar]
- 14.Graudins A, Stearman A, Chan B. Treatment of the serotonin syndrome with cyproheptadine. J Emerg Med 1998;16:615–19. [DOI] [PubMed] [Google Scholar]
- 15.Soll C, Jang JH, Riener MOet al. Serotonin promotes tumor growth in human hepatocellular cancer. Hepatology 2010;51:1244–54. [DOI] [PubMed] [Google Scholar]