Abstract
Migraine is a common clinical disorder, quite disabling and affecting the quality of life in majority of patients. The visual aura is the commonest among all types of aura. Various types of migraine aura described in the literature are photopsia, fortification spectra, scotoma, visual distortion, haemianopia and metamorphsia. The epileptic visual aura differs from aura associated with migraine in certain features: short lasting for 2-3 minutes, occurring in clusters, multicoloured and circular in shape. The ictal manifestations of occipital lobe lesions can mimic episodes of migraine with visual aura according to some reports. In this case report, we intended to highlight aggravation and increased frequency of headache attacks and changed pattern of aura induced by occipital lobe cysticercus granuloma in a patient diagnosed of migraine with aura. The importance of neuroimaging of brain in state of unexpected increased frequency of headache episodes has been emphasised.
Background
Migraine is a common, neurovascular primary headache disorder, causing substantial morbidity.1 Migraine mainly manifest with aura or without aura. The visual aura is the commonest presentation, followed by sensory, motor and aphasic auras.2 Migraine has complex pathophysiological mechanisms and episodes are characterised by four phases: prodrome, aura, headache and postdromal phase. The visual manifestations preceding the migraine headache are commonly found in occipital lobe seizures. The visual features of epileptic seizures are characterised by brief spells lasting for 2–3 min, multicoloured, circular in shape with ipsilateral onset.3 This case report highlighted the intensification and increased frequency of headache along with changed visual aura due to occipital lobe granuloma. The institution of antiepileptic drug with albendazole therapy led to remarkably decreased frequency of headache episodes at follow-up after 6 months.
Case presentation
A 21-year-old woman presented to outpatient department with complaints of headache and bright flashes of light prior and during the episode of headache since 2 years. Headache was insidous in onset, usually bifrontal to begin but would become holocranial within 15–30 min, moderate in intensity, lasting for 4–12 h, occured once or twice a month and interfering in patient's routine activity. It was accompanied with nausea and vomiting and associated with phono-photophobia. She also complained of bright and zigzag scintillating scotoma occuring in the centre of visual field and increases to occupy the whole visual field lasting for 15–20 min (figure 1). Her symptoms were relieved after taking analgesics. Since the last 2 months she noticed increase in the frequency of headache and change in the character of visual aura. She noticed yellow–red coloured circular forms appearing in left hemifield, lasting for 2–3 min occuring almost daily (figure 2). There was no history of focal neurological deficit, ataxia, convulsions or loss of consciousness. The family history was non-contributory. The clinical examination did not reveal any abnormality.
Figure 1.
Sketch diagram drawn by the patient during episodes of migraine with visual aura, revealed zig-zag pattern.
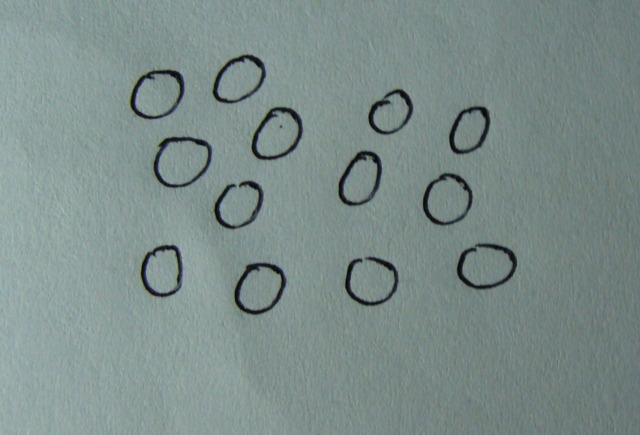
Figure 2.
Patient self-description, demonstrated multiple circles, suggestive of visual seizures.
Investigations
The EEG of the patient showed normal study. The patient underwent MRI with contrast study which demonstrated right-sided occipital lobe cystic granuloma with perilesional oedema (figure 3). Enzyme-linked immunosorbent assay for neurocysticercosis revealed positive results.
Figure 3.

MRI, T2 fluid attenuated inversion recovery axial image depicted ring shape lesion with perifocal oedema, suggestive of cysticercus granuloma.
Treatment
The patient was started divalproex 500 mg once a day in sustained release preparation and albendazole 15 mg/kg body weight per day and prednisolone 1 mg/kg body weight per day for a month. After 3 days of starting medication, she developed rash and hence she discontinued the medication on her own. There was increase in the frequency of positive scotomata. This was also accompanied by episodes of oro-facial numbness and she developed a single episode of generalised tonic clonic seizure followed by loss of consciousness. She was switched over to oral levetiracetam 500 mg twice daily, flunarizine 10 mg per day and albendazole and prednisolone was continued.
Outcome and follow-up
The patient showed complete clinical improvment. She never had seizure till 6 months of follow-up. Her headache episodes had greatly decreased in frequency with mild intensity.
Discussion
The visual manifestations preceding a migraine like headache are commonly found in occipital lobe seizures. The visual aura due to epileptic seizures is characterised by brief episodes, lasting for 2–3 min, multicoloured, circular in shape with ipsilateral onset. There is an absence of photophobia and postictal headache does not have throbbing and pulsatile character. The migraine visual manifestations are usually black and white in colour, zigzag patterns, lasting for more than 3 min, followed by headache which comprises photophobia, phonophobia and vomiting.4 In our patient, there was change in visual aura, induced by occipital lobe granuloma.
Neurocysticercosis, caused by tinea solium, is a common cause of symptomatic epilepsy in the developing world.5 It has diverse clinical presentation depending upon their site, number, stage and perilesional oedema. MRI is an essential tool in diagnosis of symptomatic occipital epilepsy due to space occupying lesion. Failure to differentiate visual aura from visual ictal symptoms leads to erroneous diagnosis and incorrect treatment for migraine instead of antiepileptic drugs.6 In our patient, cystic granuloma with perilesional oedema located in the right occipital lobe led to ictal visual symptoms, which was followed by postictal headache and vomiting mimicking an episode of migraine with visual aura.
The aura defined by International Headache Society (2004) as episodic disorder characterised by attacks of reversible focal neurological manifestations that develop slowly in a span of 5–20 min lasting less than an hour. The visual aura represents spreading depression, depolarising wave traversing anteriorly from the occipital lobe.2
The different types of visual aura described are photopsia (unformed flashes of light), fortification spectra (bright zigzag margins), scotoma (crescent-shaped blind spot), visual distortion, hemi-anopia and metamorphopsia (altered shapes of objects).7
The neuronal hyperexcitability due to occipital lobe lesion may reduce the threshold for cortical spreading depression, which may explain the change in pattern of visual aura in our patient. The cortical spreading depression enhances secretion of calcium, sodium and potassium ions which has also been seen in epileptic brain lesions. The visual hallucinations, vision loss and headache are known ictal symptomatology of seizures due to occipital lobe lesions such as tumours, arterio-venous malformations, head injury and benign occipital epilepsy of childhood.8 9
We presume that the changed aura pattern represents occipital lobe seizures. The implication would be that patient was vulnerable for full-blown epileptic seizures, which truly happened in our case. The patient had almost complete subsidence of headache episodes in the following 6 months, after starting appropriate therapy.
Learning points.
Comprehensive evaluation of visual symptoms can help in clinically differentiating between migraine aura and visual seizures.
Visual seizures mimicking as migraine visual aura may be erroneously treated with antimigraine agents instead of antiepileptic drugs.
The case report highlighted the role of structural disorder (occipital lobe cysticercus granuloma) in enhancing cortical hyperexcitability.
The change in visual aura pattern and increased frequency of headache episodes in known patient of migraine with aura should alarm the physician about the possibility of occipital lobe lesion and should be ruled out with the help of neuroimaging.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Stovner LJ, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27:193–210. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24(Suppl 1):9–160. [DOI] [PubMed] [Google Scholar]
- 3.Panayiotopoulos CP. Elementary visual hallucinations in migraine and epilepsy. J Neurol Neurosurg Psychiatr 1994;57:1371–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson PD, Thadani VM, Darcey TM, et al. Occipital lobe epilepsy: clinical characteristics, seizure spread patterns, and results of surgery. Ann Neurol 1992;31:3–13. [DOI] [PubMed] [Google Scholar]
- 5.Román G, Sotelo J, Del Brutto O, et al. A proposal to declare neurocysticercosis an international reportable disease. Bull World Health Organ 2000;78:399–406. [PMC free article] [PubMed] [Google Scholar]
- 6.Menon B. Symptomatic occipital epilepsy misdiagnosed as migraine. Headache J Head Face Pain 2007;47:287–9. [DOI] [PubMed] [Google Scholar]
- 7.Russell MB, Olesen J. A nosographic analysis of the migraine aura in a general population. Brain 1996;119:355–61. [DOI] [PubMed] [Google Scholar]
- 8.Hadjikhani N, Sanchez Del Rio M, Wu O, et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci USA 2001;98:4687–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koch UR, Musshoff U, Pannek HW, et al. Intrinsic excitability, synaptic potentials, and short-term plasticity in human epileptic neocortex. J Neurosci Res 2005;80:715–26. [DOI] [PubMed] [Google Scholar]