Abstract
Fibrodysplasia ossificans progressiva (FOP) is a rare, disabling connective tissue disorder of unknown aetiology. Its occurrence is usually sporadic but may be an inherited autosomal-dominant condition with wide range of expression. FOP is characterised by congenital malformations of the great toes and abnormal progressive heterotopic ossification of striated muscles, tendons, ligaments, fascia and aponeuroses of the trunk and extremities leading to painful swellings. The ossifications typically appear within the first decade of life, resulting in progressive morbidity and severe disability. So far, there has been no effective treatment or prevention. In the early localised phase of disease it may be misdiagnosed, hence the role of correct diagnosis through imaging is essential. Herein, we report a case of a 10-year-old female who was evaluated radiologically and diagnosed as a case of FOP. The findings of plain radiography are described and the role of CT is highlighted.
Background
The following case report shows the multidetector CT images of a rare, inherited connective tissue disorder characterised by fibrosis and ossification of soft tissues in various body parts known as fibrodysplasia ossificans progressiva (FOP) (also known as myositis ossificans progressiva or Munchmeyer's disease). In this condition, painful stony hard swellings are formed that cause significant morbidity and disability; hence the name of ‘Stone man disease’ has also been described.1 Only about 600 cases have been described in medical literature.2 The fact that FOP is so rare finds a number of doctors incorrectly diagnosing patients with the disorder. The process of diagnosing FOP can take months, or even years because of its rarity and unfamiliarity on the part of doctors. Herein we present superior quality images of such a case and think that it may be of interest to the readership of BMJ as diagnostic errors have been documented in up to 87% of FOP cases worldwide, with cancer being the most common incorrect diagnosis. CT with three-dimensional multiplanar postprocessed images gives better and earlier visualisation of ongoing ossification, anatomical details and preosseous lesions that are likely to be missed on conventional radiographs. We would hence like to lay emphasis on this modality as it can confidently diagnose and differentiate this unusual disease.
Case presentation
A 10-year-old female patient presented with congenital deformities of bilateral great toes together with multiple focal, rubbery to hard, tender, progressively increasing soft tissue swellings over the body and progressive bilateral hearing loss for 4 years. Some of these swellings had been precipitated by various diagnostic procedures like biopsies or by minor trauma. Movement restriction was present at multiple joints, with associated skeletal deformities. There was no other significant prenatal, perinatal or postnatal history or any other contributory family history. Physical examination supported the patient's various complaints and demonstrated hallux valgus and dorso-lumbar scoliosis. Her biochemical indices were within normal limits except for anaemia.
Investigations
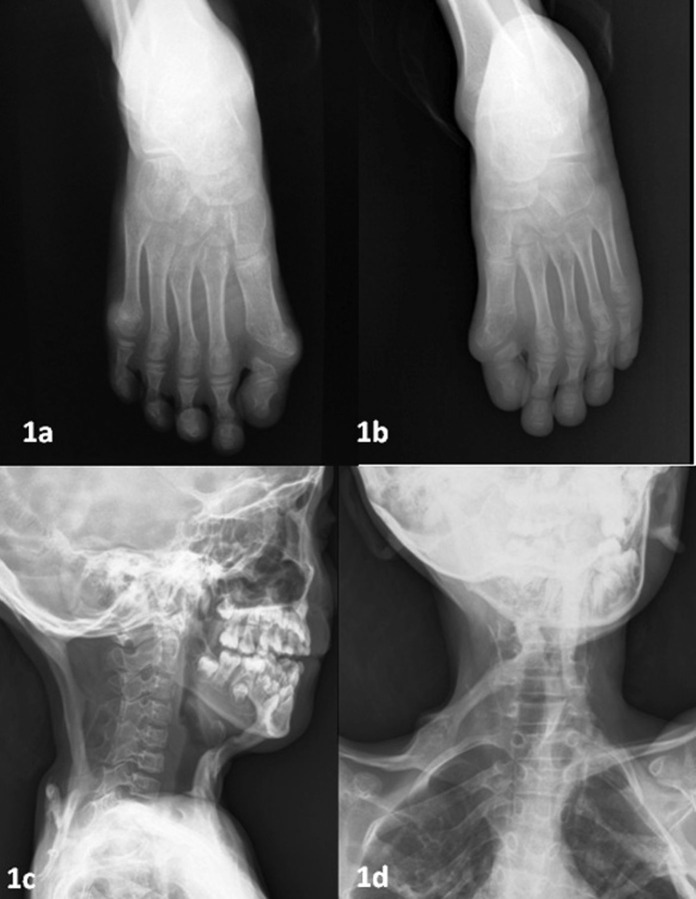
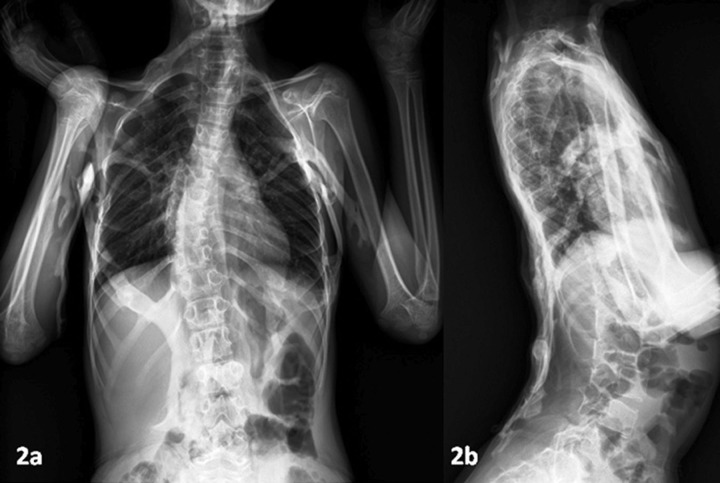
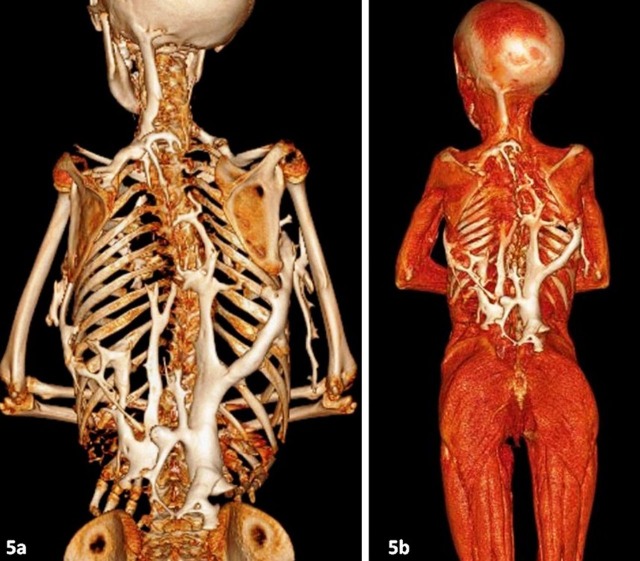
The patient was referred to the Department of Radiodiagnosis for detailed skeletal survey that revealed bilateral hallux valgus and small proximal phalanx (figure 1A,B).There was cord-like ossification of muscles of right anterior and bilateral posterior aspect of neck (figure 1C, D), chest, abdominal, left lateral thigh and back muscles, giving an appearance of a branching tree (figure 2A, B). There was dorso-lumbar scoliosis with primary curvature towards the right. CT of the patient was requested by the pediatrician to evaluate for the preosseous lesions or ongoing ossifications and to rule out other abnormalities. Non-contrast multidetector CT (MDCT) scan with three-dimensional reformations was done on a 64-slice scanner (Philips 64 Slice Brilliance CT Scan Unit, the Netherland), using paediatric protocol to minimise the radiation dose. Images were post-processed on a commercial workstation using multiplanar reformatted (MPR), volume rendered (VR), maximum intensity projection (MIP) images (figures 3–5). Tomography findings supplemented the radiographic with exquisite visualisation of extensive ossifications of soft tissues. Multiple preosseous sites with early ossifications in abdominal and back muscles were also demonstrated (figure 4), which were not detected on plain radiographs. There were no other visceral abnormalities. On the basis of clinico-radiological findings with normal biochemical profile, a final diagnosis of FOP was made.
Figure 1.
(A, B) Plain radiographs bilateral feet showing congenital deformities of great toes because of small proximal phalanx and bilateral hallux valgus. (C, D) Plain radiographs neck anteroposterior (AP) and lateral view showing well-defined cord-like ossifications of anterior and posterior neck muscles with straightening of the cervical spine.
Figure 2.
(A) Plain radiographs chest posteroanterior (PA) view including abdomen and arms showing extensive focal and cord-like ossification of muscles and soft tissue of back, chest, abdomen and visualised both arms giving pattern of branching tree with dorso-lumbar scoliosis. (B) Plain radiographs thorax and abdomen showing ossification of soft tissue of back.
Figure 3.
(A–D)Coronal maximum intensity projection CT images of thorax, abdomen, arms, neck and thighs showing ossification of back, chest, abdomen, arms, neck and left thigh muscles with dorso-lumbar scoliosis.
Figure 4.
Coronal maximum intensity projection CT images of abdomen and lower thorax showing early ossifying lesions of muscles and soft tissues and preosseous lesions as mild increased attenuation of back and pelvic muscles which were missed on plain radiographs.
Figure 5.
(A, B) Coronal volume rendered CT images of the upper half of the body showing excellent demonstration of soft tissue and muscle ossifications in ‘tree branching pattern’.
Differential diagnosis
The differential diagnoses in early stage of disease with focal progressive mineralised masses include dermatomyositis, tumoral calcinosis, some bone malignancies (juxtacortical osteosarcoma), soft tissue sarcomas and fibromatoses.3 In advanced disease with extensive heterotopic ossification diagnosis is usually a clinico-radiological one, with emphasis on detection of preosseous lesions.
Treatment
Supportive medical management was done. The patient was advised to rest along with avoidance of exercise and traumatic events. He was given non-steroidal anti-inflammatory medications and glucocorticoids for symptomatic relief and was specifically advised against undergoing any invasive procedure.
Outcome and follow-up
Although the patient showed symptomatic improvement and is stable, a significant morbidity and disability is still present in the short-term follow-up of 6 months.
Discussion
FOP, first described in 1648 by Guy Patin, is a rare disorder with no ethnic, racial, geographical or sex predisposition; the incidence being one case per two million live births.3 4 Genetic transmission is autosomal dominant with variable expression but the inheritance because of spontaneous mutations is most common.3
FOP is characterised by the cardinal features of heterotopic progressive osteogenesis and digital anomalies. The heterotopic ossification (HO) starts at the mean age of 3–5 years and is found in almost all patients of less than 15 years of age.5 6 The main target is the axial musculature, but eventually ectopic bone formation involves the ligaments, the fascia, the aponeuroses, the tendons and the joint capsules, usually showing a proximal-to-distal pattern. Congenital abnormalities of the great toes usually present in 79–100% of patients; microdactyly of both halluces with single phalanx in valgus position being most common.6 Hand deformities may be present as short first metacarpal and brachymesophalangy of the fifth finger with clinodactyly.7 Deafness and baldness are reported in up to one-fourth of the cases. Mental retardation is rare.5 Biochemical tests including serum alkaline phosphatases, parathyroid hormone level, renal function test, hematological indices, serum and urinary calcium and phosphates are usually within the normal range.
Painful soft tissue nodules/masses around head and neck with torticollis are the earliest symptoms. They are followed by hard soft tissue swelling and ossifications of other parts of body. These may lead to restricted movement and deformities depending on the extent of involvement. Involvement of intercostals, prevertebral and paravertebral muscle with ankylosis of costo-vertebal/costo-sternal joints and increasing spinal deformities (kyphoscoliosis) decreases the thoracic volume and elastic recoil, thus leading to respiratory compromises with thoracic insufficiency syndrome.8 This is the usual cause of death in these patients.
Diagnostic errors have been documented in up to 87% of FOP cases worldwide, with cancer being the most common incorrect diagnosis.9 This usually alters the natural history and causes iatrogenic harm. FOP is a clinico-radiological diagnosis. Conventional radiography is usually enough to arouse suspicion and to provide knowledge about bony deformities of great toes and hands and the ectopic ossifications. Abnormalities of the cervical spine, temporo-mandibular joint, femoral neck and medial tibial osteochondromas may also be found. These patients are not prone to fractures; on the contrary, healing occurs rapidly because of HO.10
CT with three-dimensional processed images (MPR, MIP and VR) gives better and earlier visualisation of ongoing ossification than by standard radiography. It usually provides better anatomical details and also identifies the preosseous lesions, which are likely to be missed on conventional radiographs. These lesions appear as low-attenuation soft tissue mass or an enlarged muscle belly, occasionally with indistinct, adjacent soft tissue planes.11 MRI, though not routinely used for the evaluation, shows a low-signal-intensity rim and a heterogeneous, high-signal-intensity rim and tumor-like enlargement of affected tissues with early intense heterogeneous gadolinium enhancement.11 Bone scintigraphy with 99mTc- methyl-diphosphonate is another option for thorough assessment and shows abnormal uptake in preosseous soft tissue and demonstrates early HO.12 Histological examination shows a pronounced proliferation of fibroblasts within the muscles in several areas, leading to the destruction of muscle fibers, plus areas of newly formed bone tissue. The well-developed osseous lesions show a typical picture of mature bone with Haversian systems.11
Exacerbation of ossifications can occur spontaneously or may be precipitated by incidental or iatrogenic trauma .Thus, biopsy and surgical procedures are avoided as diagnostic or therapeutic options. Medical management is currently supportive.4 Non-steroidal anti-inflammatory medications, glucocorticoids cyclo-oxygenase-2, leukotriene inhibitors and mast cell stabilisers are useful anecdotally in managing chronic discomfort and ongoing flare-ups, but till date no efficacy has been reported with any therapy in altering the natural history of the disease.4 Surgical interventions for contractures and deformities and osteotomy/surgical removal of ectopic bones are generally unsuccessful and pose an extra risk for post-traumatic HO.
Learning points.
It is a rare heritable disorder—autosomal-dominant or spontaneous mutation, thus genetic counseling may play a role in the prevention of disease.
Affected individuals are normal at birth except for congenital deformity of the great toe with hallux valgus that may be used as indication for follow-up.
A misdiagnosis or delayed diagnosis can adversely affect these patients leading to inappropriate and unnecessary testing such as biopsies that may cause flare-ups and permanent immobility. This may also cause avoidable inappropriate treatments such as chemotherapy.
Radiography and specially multidetector CT are the most essential imaging modalities for early diagnosis of the disease and avoiding wrong diagnosis.
Patients with FOP should be treated symptomatically with special emphasis on avoiding the invasive procedure (surgery and biopsy) that may exacerbate the disease process.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Schober P, Krage R, Thone D, et al. Ultrasound-guided nkle block in dtone man disease, fibrodysplasia ossificans progressiva. Anesth Analg 2009;109:988–90. [DOI] [PubMed] [Google Scholar]
- 2.Majmudar DK, Hathila NN, Vaishya KB, et al. Fibrodysplasia ossificans progressive. Indian J Radiol Imaging 2005;15:347–8. [Google Scholar]
- 3.Magryta CJ, Kligora CJ, Temple H, et al. Clinical presentation of fibrodysplasia ossificans progressiva: pitfalls in diagnosis. J Pediatric Hematol Oncol 1999;21:539–43. [PubMed] [Google Scholar]
- 4.Kaplan FS, Merrer ML, Glaser DL, et al. Fibrodysplasia ossificans progressiva. Best Pract Res Clin Rheumatol 2008;22:191–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connor JM, Evans DA. Fibrodysplasia ossificans progressiva, the clinical features and natural history of 34 patients. J Bone Joint Surg 1982;64:76–83. [DOI] [PubMed] [Google Scholar]
- 6.Smith R. Fibrodysplasia (myositis) ossificans progressiva: clinical lessons from a rare disease. Clin Orthop Rel Res 1998;346:7–14. [PubMed] [Google Scholar]
- 7.Schroeder HW, Zasloff M., Jr The hand and foot malformations in fibrodysplasia ossificans progressiva. Johns Hopkins Med J 1980;147:73–8. [PubMed] [Google Scholar]
- 8.Kaplan FS, Glaser DL. Thoracic insufficiency syndrome in patients with fibrodysplasia ossificans progressiva. Clin Rev Bone Miner Metab 2005;3:213–16. [Google Scholar]
- 9.Kitterman JA, Kantanie S, Rocke DM, et al. Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 2005;116:654–61. [DOI] [PubMed] [Google Scholar]
- 10.Einhorn TA, Kaplan FS. Traumatic fractures of heterotopic bone in patients who have fibrodysplasia ossificans progressiva. Clin Orthop Rel Res 1994;308:173–7. [PubMed] [Google Scholar]
- 11.Mavrogenis AF, Soucacos PN, Panayiotis J, et al. Heterotopic ossification revisited. Orthopedics 2011;34:177. [DOI] [PubMed] [Google Scholar]
- 12.Trisha V, Kumar R, Khan SA, et al. Characteristic appearance on bone scintigraphy of a ‘Stone Man’. Clin Nucl Med 2005;30:517–18. [DOI] [PubMed] [Google Scholar]