Abstract
Aneurysmal rupture is the commonest cause of non-traumatic subarachnoid haemorrhage (SAH). SAH can rarely be the manifestation of cortical venous thrombosis (CVT). CVT is potentially lethal but treatable disorder with positive outcome if timely treatment is instituted. The site of bleeding is mainly on convexities and sulcus with sparing of basal cisterns in SAH related to CVT. Anticoagulation is the mainstay of treatment, in spite of SAH complicated by CVT. In this submission, the author highlighted a case of SAH presented as initial manifestation of CVT in an elderly woman. Early therapy with anticoagulation led to complete clinical and radiological recovery in a short duration of 2 weeks. Thus, diagnosis of CVT should be kept in mind in unusual presentation of SAH.
Background
Aneurysmal rupture is the most common non-traumatic aetiology of subarachnoid haemorrhage (SAH).1 However, rarely SAH may be an initial presentation of cortical venous thrombosis (CVT). The presence of SAH is a relative contraindication for anticoagulant therapy but anticoagulation is required for treatment of CVT. Hence, diagnosis of CVT becomes of paramount significance as treating CVT would lead to early reduction in venous pressure and thereby preventing its expansion and recurrence. CVT initially presented as SAH has been rarely reported till now.2–4
We report a case of CVT presenting as SAH and some clues towards early diagnosis of CVT.
Case presentation
A 65- year-old woman was admitted to the neurology ward, complaining of sudden onset generalised dull aching headache for last 4 days. Headache was persistent throughout the day and became so severe in intensity so as to disturb her sleep. Headache was associated with vomiting. There was no history of altered sensorium, seizure or focal neurological deficit. She was a known case of diabetes mellitus and on oral drugs since last 8 years with poor medication compliance.
On physical examination, blood pressure was 130/80 mm Hg, pulse rate 68/min and respiratory rate was 18/min. Neurological examination revealed normal higher mental function without any cranial nerve palsy. Fundus examination was remarkable for bilateral papilloedema. Motor system examination showed normal tone and power, deep tendon jerks were present and plantars were bilaterally flexors. The rest of the examination was normal.
Investigations
Lab investigations include complete haemogram, liver function tests and renal function tests were normal. Random blood sugar was 286 mg/dl. The lipid profile did not reveal abnormal status. The thrombophilia was absent. The autoreactivity for antinuclear antibody, anticytoplamic neutrophilic antibody, rheumatoid factor and antiphospholipid antigens were negative. The thyroid study showed normal results. The 2D echo cardiac assessment did not demonstrate valvular abnormality or intracardiac thrombus. Prothrombin time was 13 s and international normalised ratio (INR) was 1.2. Cerebrospinal spinal fluid (CSF) appearance was turbid red. CSF microscopy revealed plenty of red blood cells (RBCs) with total RBC count 1 45 000/mm3 of which were 40% crenated RBCs, favouring a diagnosis of SAH. Non-contrast CT of the head demonstrated bilateral hyperdensity over perisylvian fissures, suggestive of SAH (figure 1). CT angiogram was normal and did not reveal any aneurysm or arterio-venous malformation (figure 2). CT venogram showed filling defects in superior saggital sinus suggestive of thrombosis (figure 3). The gradient recoil echo, T2-weighted MRI demonstrated bleeding at sulcus (figure 4).
Figure 1.

Non-contrast CT of the head showing bilateral bleeding near perisylvian sulcus.
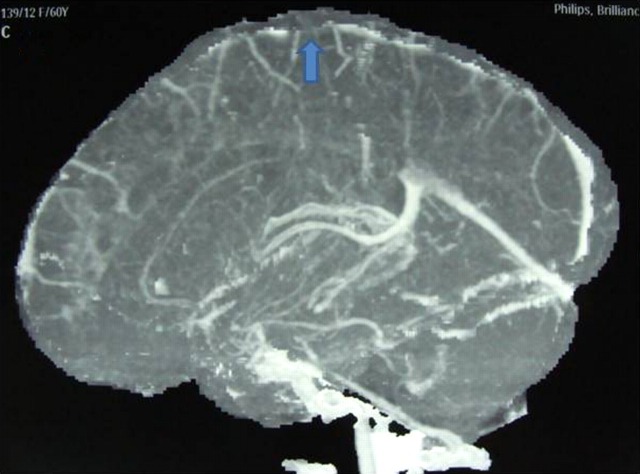
Figure 2.
CT angiogram did not reveal any abnormality.
Figure 3.
CT venogram (sagittal section) showing filling defect in superior saggital sinus s/o thrombosis.
Figure 4.
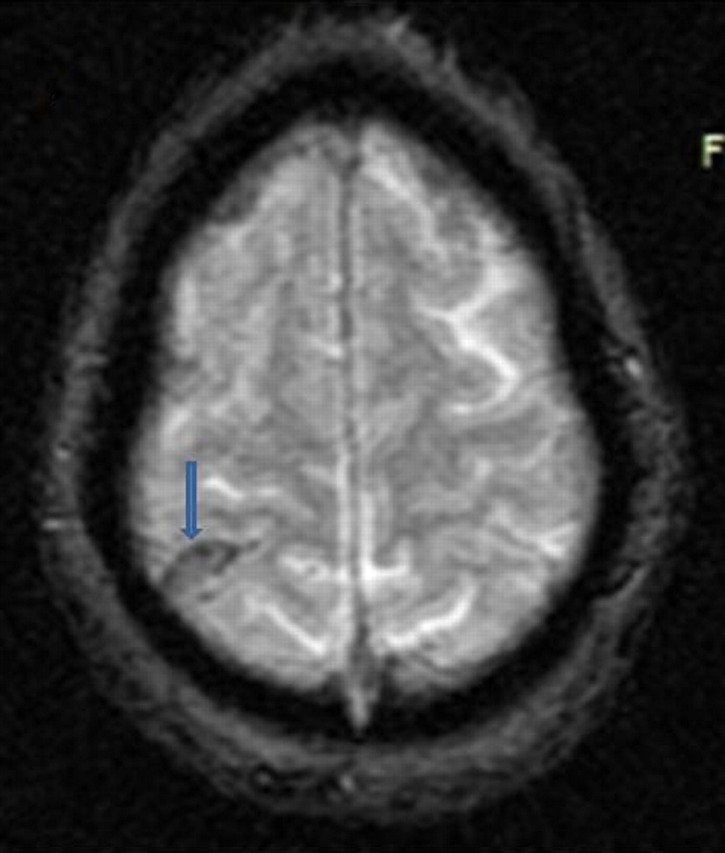
MRI Brain: Gradient recall echo (GRE) sequence showing blooming due to inter-sulcal bleed.
Differential diagnosis
Treatment
Patient was started on low-molecular-weight heparin (enoxaparin) at 1 mg/kg body weight twice daily and overlapped with oral anticoagulant once INR was in therapeutic range (2–3). The patient rapidly showed improvement with the therapy.
Outcome and follow-up
She became asymptomatic within 2 weeks. MR venogram done after 2 weeks depicted recanalization of occluded sinus and disappearance of collaterals (figure 5).
Figure 5.
MR venography demonstrated complete recanalisation of superior saggital sinus after 2 weeks of anticoagulant therapy.
Discussion
SAH is an unusual manifestation of CVT. Due to a wide variety of clinical manifestations ranging from trivial headache to status epilepticus, the diagnosis of CVT remains a great challenge.5 6
Common non-traumatic aetiology of SAH comprises aneurysmal bleeding (85%), dissection of artery, dural A–V fistula, blood dyscrasias, pituitary apoplexy and cocaine abuse.1 As per exhaustive search of literature, CVT is a rare cause of SAH.2–6 Shukla et al7 reported a case of SAH due to multiple major venous sinus thrombosis. Another study presented three cases of isolated thrombosis of cortical vein causing SAH without parenchymal involvement. Pathophysiology of SAH in CVT remains largely undefined; however, many theories have been postulated. De Bruijn et al8 reported SAH in venous haemorrhagic infarction with secondary rupture into subarachnoid space. However, in our case no intraparenchymal bleeding was demonstrated on CT imaging. Hyperdensity suggestive of haemorrhage was seen at perisylvian sulcus without involvement of basal cistern indicative of SAH. More acceptable theory in our case is due to rupture of thin fragile dilated cortical veins over cerebral surface because of secondary venous hypertension leading to SAH. This explains the involvement of brain convexities and interhemisphere fissure without involvement of basal cistern due to SAH.
The distribution of SAH and location of occluded venous sinus in previous case reports is shown in table 1.9–11 The observations have been found that SAH usually occurs within the territory of thrombosed cortical venous sinus. But it can also occur outside the territory. However, it is difficult to draw any conclusion on the basis of these few case reports and it would be prudent to wait till larger case series are published addressing this issue.
Table 1.
Distribution of SAH and location of occluded venous sinus in previous case reports
| Study | Site of SAH | Location of occluded venous sinus |
|---|---|---|
| Lai et al9 | Right frontoparietal sulcus | Superior sagittal sinus |
| Oppenheim et al10 | Case 1: right frontal convexity | Both transverse and sagittal sinus |
| Case 2: left insular sulcus | Superior sagittal and left transverse sinus | |
| Case 3: anterior interhemispheric sulcus | Sagittal and right transverse sinus | |
| Bindu et al11 | Case 1: left sylvian fissure, anterior interhemispheric sulcus and bilateral frontoparietal convexities | Superior sagittal and right transverse sinus |
| Case 2: right sylvian fissure and posterior interhemispheric sulcus | Superior sagittal and left transverse sinus and straight sinus | |
| Case 3: right frontal convexity, right cingulate sulcus, anterior interhemispheric sulcus | Superior sagittal and bilateral transverse sinus and straight sinus | |
| Case 4: interhemispheric fissure, bilateral frontoparietal convexities and left sylvian fissure | Superior sagittal sinus | |
| In our case | Bilateral perisylvian sulci | Superior saggital sinus |
SAH, subarachnoid haemorrhage.
The risk factors associated with CVT include pregnancy, dehydration, coagulopathies, systemic illness, infection, drugs and idiopathic causes.12 Diabetes mellitus was found to be one of the risk factors in our case. Clinically it is very difficult to differentiate between SAH due to aneurysmal bleed and CVT. So it is necessary to enquire about potential risk factors for CVT in a case of SAH-like postpartum state, ear, nose and sinus infection, prothrombotic state and connective tissue disorder. CVT is a serious but fully curable condition and early diagnosis and proper treatment leads to favourable outcome.
In our case, the patient presented with headache and vomiting without focal neurological deficit. CT of the head and CSF was suggestive of subarachnoid bleeding without any parenchymal involvement. CT venogram revealed superior saggital sinus thrombosis. The patient was started on anticoagulant therapy with maintaining the INR in therapeutic range (2–3). Over the period of 2 weeks patient improved symptomatically and repeat MR venogram showed complete recanalisation of superior sagittal sinus.
Learning points.
Initial presentation of subarachnoid haemorrhage (SAH) with sudden-onset headache should be evaluated for rare aetiology like cortical venous thrombosis (CVT).
The high index of suspicion is required of SAH complicated by CVT, if bleed is present on convexities and fissures with absence of blood in basal cisterns.
Presence of risk factors associated with CVT presenting as SAH may be the diagnostic clue.
MR arteriography and venography excludes other common non-traumatic causes of SAH.
Anticoagulant therapy in a case of CVT will prevent further expansion and recurrence of SAH.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Van Gijn J, Rinkel GJ. Subarachnoid haemorrhage: diagnosis, causes and management. Brain 2001;124:249–78. [DOI] [PubMed] [Google Scholar]
- 2.Szancer S. Acute cerebral venous occlusion manifested by spontaneous haemorrhage. Neurology 1955;5:675–7. [DOI] [PubMed] [Google Scholar]
- 3.Ra CS, Lui CC, Liang CL, et al. Superior sagittal sinus thrombosis induced by thyrotoxicosis: case report. J Neurosurg 2001;94:130–2. [DOI] [PubMed] [Google Scholar]
- 4.Sztazel R, Coeytaux A, Dehdashti AR, et al. Subarachnoid haemorrhage: a rare presentation of cerebral venous sinus thrombosis. Headache 2001;41:889–92. [PubMed] [Google Scholar]
- 5.Ferro JM. Cerebral venous thrombosis. J Neuroradiol 2002;29:231–9. [PubMed] [Google Scholar]
- 6.Bousser MG. Cerebral venous thrombosis: report of 76 cases. J Mal Vasc 1991;16:249–54. [PubMed] [Google Scholar]
- 7.Shukla R, Vinod P, Prakash S, et al. Subarachnoid haemorrhage as a presentation of cerebral venous sinus thrombosis. J Assoc Physicians India 2006;54:42–4. [PubMed] [Google Scholar]
- 8.de Bruijn SF, Stam J, Kappelle LJ. Thunderclap headache as first symptom of cerebral venous sinus thrombosis: CVST study group. Lancet 1996;348:1623–5. [DOI] [PubMed] [Google Scholar]
- 9.Lai NK, Hui JW, Wong GK, et al. Cerebral venous thrombosis presenting as subarachnoid haemorrhage. Hong Kong Med J 2008;14:499–500. [PubMed] [Google Scholar]
- 10.Oppenheim C, Domigo V, Gauvrit JY, et al. Subarachnoid hemorrhage as the initial presentation of dural sinus thrombosis. AJNR Am J Neuroradiol 2005;26:614–17. [PMC free article] [PubMed] [Google Scholar]
- 11.Bindu T, Panda S, Chandrashekar HS, et al. Subarachnoid hemorrhage: an unusual presentation of cerebral venous sinus thrombosis. Ann Indian Acad Neurol 2006;9:32–5. [Google Scholar]
- 12.Bousser MG, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol 2007;6:162–70. [DOI] [PubMed] [Google Scholar]