Abstract
Castleman's disease represents an atypical lymphoproliferative disorder which is non-clonal but can turn malignant in the form of lymphoma, Kaposi's sarcoma or plasma cell dyscrasia. It has been reported in association with diseases like polyneuropathy organomegaly endocrinopathy monoclonal gammopathy skin changes syndrome and myeloma and very rarely it can be associated with cutaneous vasculitis as in our case. It relatively runs an aggressive course and has a shorter survival. No standard of care therapy is yet established for multicentric Castleman's disease accompanying myeloma. We successfully treated one such patient with bortezomib-based therapy.
Background
Multicentric Castleman's disease (MCD) is a systemic disorder characterised by angiofollicular lymph node hyperplasia and multiorgan involvement. Its association with myeloma is uncommon and treatment of this condition has not been standardised as yet. Bortezomib is a novel proteasome inhibitor that affects myeloma cell growth by nuclear factor-κB (NF-κB) blockade. Clinical trials have clearly demonstrated that bortezomib is active in patients with relapsed and refractory myeloma as well as in fresh myeloma patients but there is no much literature on how to treat Castleman's disease/myeloma overlap. Exploring the efficacy of bortezomib in MCD with myeloma, we successfully treated a 51-year-old man who had overlapping features of MCD and myeloma, associated with cutaneous vasculitis with bortezomib, where very good partial remission was observed.
Case presentation
A 51-year-old man presented with right cervical lymph node of 1 cm in size in 2001 without any constitutional symptoms. Fine needle aspiration cytology as well as surgical biopsy showed reactive lymphadenitis. He was kept on follow-up. Six years later, he developed recurrence at the same site along with left axillary lymph node of 2×2 cm in size. This time he also had generalised weakness and weight loss of 5 kg in 3 months. There was no history of fever or excessive sweating. Clinical examination revealed mild pallor, right cervical and left axillary lymph nodes but no organomegaly. The patient was found to have diabetes mellitus, hypothyroidism and hypertension during the same evaluation for which he received appropriate treatment. Then, in 2009, he developed renal insufficiency with creatinine of 3.8 and multiple painful skin lesions predominantly over the trunk (figure 2A).
Investigations
Among the investigations complete blood counts revealed mild anaemia (haemoglobin of 11.5 g/dl) with normal total leucocyte count, differential count and platelet count. Erythrocyte sedimentation rate was 63 mm for the first hour. Kidney function tests were normal. Liver function tests revealed total protein of 8.5 gm/dl and albumin of 2.7 gm/dl with globulins on the higher side. Non-contrast CT of neck revealed discrete homogenous right deep cervical, posterior triangular, submandibular and supraclavicular lymphadenopathy. Contrast enhanced CT chest/abdomen revealed discrete enhancing nodes in left axilla with small right paratracheal and left paraaortic nodes. Left axillary lymph node biopsy showed hyperplastic lymph node revealing infiltration with mixed population of mature lymphocytes, neutrophils, plasma cells and few histiocytes in a haemorrhagic background. Lymphocytes were positive for leucocyte common antigen and CD20. No granuloma was seen. The overall features were consistent with Castleman's disease of plasma cell variant (figure 1). Serum protein electrophoresis revealed a monoclonal band in the gamma region (M protein=1.08 gm/dl). Urine protein electrophoresis was negative. Bone marrow aspiration did not reveal an increase in plasma cells. Skeletal survey was negative. Among the investigations carried out in 2009, ultrasound revealed bilateral medicorenal disease, skin biopsy showed leucocytoclastic vasculitis and bone marrow showed 10% plasma cells. Serum protein electrophoresis again revealed M band (M protein=2.1 gm/dl).
Figure 1.
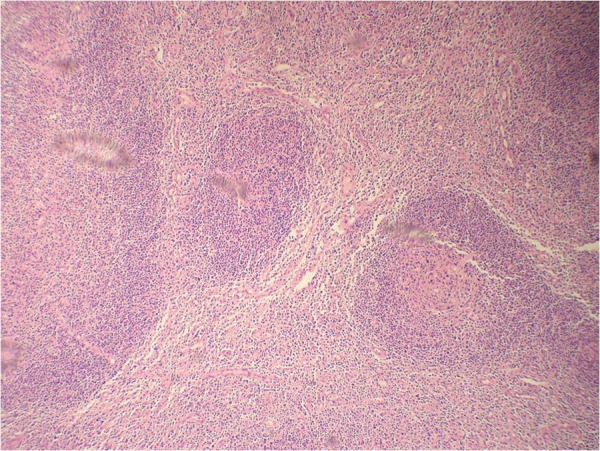
Lymph node section showing follicles with prominent germinal centre and sheets of mature plasma cells in interfollicular region, suggestive of multicentric Castleman's disease (H&E, ×100).
Differential diagnosis
The patient was given the final diagnosis of Castleman's disease with myeloma with leucocytoclastic vasculitis which fulfilled the WHO 2008 criteria (figure 3).
Figure 3.
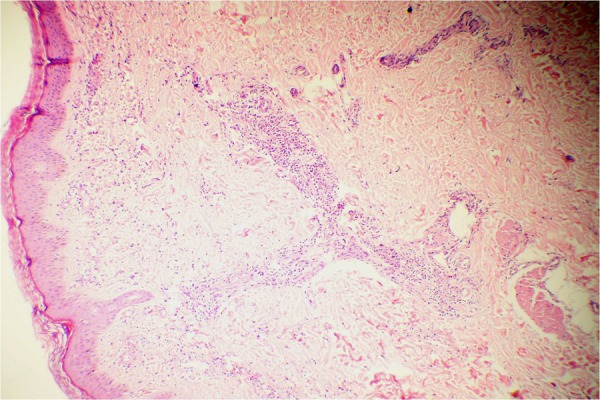
Skin biopsy showing perivascular neutrophilic infiltrate and extravasated red blood cells in the dermis suggestive of leucocytoclastic vasculitis (H&E, ×100).
Treatment
The patient received monthly cycles of bortezomib 2 mg intravenously weekly (4 injections per month) and dexamethasone 40 mg with weekly bortezomib injection for a total of eight cycles, followed by thalidomide oral 50 mg/d as maintenance.
Outcome and follow-up
During treatment the patient was examined at each weekly visit, especially for peripheral neuropathy. Complete blood counts, renal function tests, liver function tests and blood glucose were conducted at each weekly visit. Serum protein electrophoresis was carried out every 2 months. After bortezomib/dexamethasone treatment the patient showed marked improvement in the form of disappearance of lymph nodes, correction of renal failure, resolution of skin lesions (figure 2B), >90% reduction in M spike (M protein=0.18 gm/dl) and bone marrow plasma cells <5%. Presently, he is in very good partial remission at more than 2 years of follow-up.
Figure 2.

(A) Truncal skin lesions (leucocytoclastic vasculitis) before bortezomib therapy. (B) Cleared skin lesions after bortezomib therapy.
Discussion
MCD was first described by Gaba et al1 in 1978. It is more common in elderly men (men/women is 2.5∼13 : 1). It is generally of the plasma cell type or mixed variant. MCD is a systemic disease with significant peripheral lymphadenopathy and hepatosplenomegaly, as well as frequent fever, night sweats, fatigue and weight loss. Cutaneous vasculitis in Castleman's disease is rare. Izutsu et al2 in 1998 described a 62-year-old man with Castleman's disease with concomitant leucocytoclastic vasculitis and polyclonal plasmacytosis. Wolf et al3 in 2011 highlighted a case of multicentric plasma cell variant Castleman's disease who presented with cutaneous vasculitis and pulmonary parenchymal involvement in a background of ankylosing spondylitis. Abnormal laboratory findings include pancytopenia, abnormal function of liver and kidney, raised C reactive protein, interleukin 6 (IL-6) and hypergammaglobulinemia. However, monoclonal gammaglobulinaemia is rare. In addition, it has been reported in association with amyloidosis, nephrotic syndrome, Sjögren syndrome, polyneuropathy organomegaly endocrinopathy monoclonal gammopathy skin changes (POEMS) syndrome and myeloma and can progress to Kaposi's sarcoma or malignant lymphoma.4 HHV-8 infection has been regarded as an important aetiological factor for its causation. Overproduction of cytokine IL-6, either native or virally encoded, has been hypothesised to drive plasma cell proliferation in these subtypes.5 The prognosis varies greatly depending upon the histopathological type. Solitary lesions are best treated with local resection.
The MCD plasma cell subtype runs a more aggressive course with poor prognosis, and optimal therapies have not been well established. A number of therapies have been used for multicentric disease, including steroid-monotherapy and combined chemotherapy. Other therapies include interferon-α, antiviral medications, anti-IL-6 monoclonal antibody and humanised antihuman IL-6 receptor monoclonal antibody,6 All-trans retinoic acid, thalidomide7 and rituximab.8 Most of these reports included only a small number of patients.
Bortezomib has recently been shown to produce significant responses in about one-third of patients with refractory and relapsed myeloma.9 The mechanism of action of bortezomib is thought in part to be due to selective inhibition of the proteasome.10 This drug has been reported to affect myeloma cell growth by NF-κB blockade, downregulation of cytokines such as IL-6. IL-6 has been implicated in the pathophysiology of MCD, as mentioned above, providing a rationale for treatment of MCD with bortezomib. Previous clinical trials have indicated that the combination of bortezomib and dexamethasone may be additive or possibly synergistic. It is likely that the effect of bortezomib on MCD is due to inhibition of IL-6 secretion.
The effect of bortezomib on MCD associated with myeloma has not been established yet. However, there is a single case report of successful treatment of MCD with myeloma with bortezomib/dexamethasone combination. Yuan et al in 2009 reported the first case report of MCD with myeloma who showed a remarkable response to a bortezomib/dexamethasone combination. They treated a 71-year-old man who had MCD/myeloma overlap with four cycles of bortezomib and dexamethasone and found that he was in very good partial remission at 18 months of follow-up.11 Sobas et al12 in 2010 showed that bortezomib is effective in refractory MCD associated with POEMS syndrome. To the best of our knowledge, our case is probably the second one which has shown high efficacy of bortezomib-based therapy on MCD/myeloma overlap and emphasises that bortezomib-based therapies could be an attractive option for these patients.
Learning points.
High index of suspicion is required to diagnose Castleman's disease.
Leucocytoclastic vasculitis is a rare accompaniment of Castleman's disease.
Bortezomib can be an effective option for patients with Castleman's disease/myeloma overlap for which there is no standardised treatment as yet.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Gaba AR, Stein RS, Sweet DL, et al. Multicentric giant lymph node hyperplasia. Am J Clin Pathol 1978;69:86–90. [DOI] [PubMed] [Google Scholar]
- 2.Izutsu K, Usuki K, Inoue K, et al. Polyclonal plasmacytosis in peripheral blood and leukocytoclastic vasculitis in Castleman's disease. Rinsho Ketsueki 1998;39:210–15. [PubMed] [Google Scholar]
- 3.Wolf M, Van Offel JF, Van de Velde A, et al. Multicentric plasma cell variant Castleman's disease presenting with cutaneous vasculitis and pulmonary parenchymal involvement in a patient with ankylosing spondylitis: case report and review of the literature. Acta Clin Belg 2011;66:305–10. [DOI] [PubMed] [Google Scholar]
- 4.Jongsma TE, Verburg RJ, Geelhoed-Duijvestijn PH. Castleman's disease: a rare lymphoproliferative disorder. Eur J Intern Med 2007;18:87–9. [DOI] [PubMed] [Google Scholar]
- 5.Yoshizaki K, Matsuda T, Nishimoto N, et al. Pathogenic significance of interleukin-6 (IL-6/BSF-2) in Castleman's disease. Blood 1989;74:1360–7. [PubMed] [Google Scholar]
- 6.Nishimoto N, Kanakura Y, Aozasa K, et al. Humanized anti-interleukin-6 receptor antibody treatment of multicentric Castleman's disease. Blood 2005;106:2627–32. [DOI] [PubMed] [Google Scholar]
- 7.Lee FC, Merchant SH. Alleviation of systemic manifestations of multicentric Castleman's disease by thalidomide. Am J Hematol 2003;73:48–53. [DOI] [PubMed] [Google Scholar]
- 8.Ide M, Kawachi Y, Izumi Y, et al. Long-term remission in HIV-negative patients with multicentric Castleman's disease using rituximab. Eur J Haematol 2006;76:119–23. [DOI] [PubMed] [Google Scholar]
- 9.Richardson PG, Barlogie B, Berenson J, et al. A phase II study of bortezomib in relapsed, refractory myeloma. N Engl J Med 2003;348:2609–17. [DOI] [PubMed] [Google Scholar]
- 10.Rajkumar SV, Richardson PG, Hideshima T, et al. Proteasome inhibition as a novel therapeutic target in human cancer. J Clin Oncol 2005;23:630–9. [DOI] [PubMed] [Google Scholar]
- 11.Yuan ZG, Dun XY, Li YH, et al. Treatment of multicentric Castleman's disease accompanying multiple myeloma with bortezomib: a case report. J Hematol Oncol 2009;2:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sobas MA, Alonso VN, Diaz AJ, et al. Efficacy of bortezomib in refractory form of multicentric Castleman disease associated to poems syndrome (MCD-POEMS variant). Ann Hematol 2010;89:217–19. [DOI] [PubMed] [Google Scholar]


