Abstract
A 72-year-old woman underwent left wide local excision and an axillary node sampling in 2005 for a T2, N0, M0 invasive ductal carcinoma followed by adjuvant chemotherapy, radiotherapy and hormonal therapy. In 2011, she developed spontaneous blue breast discolouration. Initial examination revealed global breast firmness, skin thickening and eechymosis. Despite no evidence of recurrent disease, the patient was scheduled for fortnightly review. This review demonstrated marked worsening discolouration and new nipple areolar complex blood-filled blisters. Despite concurrent antiplatelet therapy as a possible cause, the breast clinician's clinical concern of angiosarcoma led to a skin punch biopsy, revealing only non-specific lymphocytic infiltrate. Interval mammographic assessment demonstrated non-specific architectural distortion. Regardless of these benign findings, a breast MRI was performed demonstrating possible breast angiosarcoma. Ultrasound-guided biopsy demonstrated low-grade breast angiosarcoma. The patient underwent completion mastectomy, for a 150 mm high-grade postradiotherapy angiosarcoma. Annual clinical review and contralateral mammography is planned.
Background
With breast screening and greater public awareness, the role of breast-conserving surgery for early-stage breast cancer is becoming more apparent. With the increasing indications for whole breast radiotherapy after breast-conserving therapy, the incidence of radiotherapy-induced breast angiosarcoma is changing.1
The subtle presentation of this condition, the often unremarkable breast imaging, difficulty in diagnosis and paucity of adjuvant therapy guidelines led to the highlighting of this case report to reinforce the consideration of angiosarcoma as a diagnosis in post breast-conserving surgery radiotherapy patients, presenting with delayed bruising and swelling.
Case presentation
In 2005, a 66-year-old woman presented with a left-sided breast lump. Ultrasound-guided core biopsy demonstrated a grade II invasive ductal carcinoma and she underwent a left wide local excision with axillary node sampling. Final histology demonstrated a T2, N0, M0, oestrogen receptor, progesterone receptor, human epidermal growth factor receptor 2 positive (triple positive luminal B subtype) grade II invasive ductal carcinoma.
She underwent adjuvant chemotherapy (4 cycles of adriamycin, cyclophosphamide and 17 cycles of herceptin) followed by whole-breast radiotherapy (25 fractions of 50 Gy) and 5 years of hormonal therapy. She had an annual clinical examination and mammographic surveillance.
She was started on antiplatelet, aspirin therapy following coronary artery by-pass grafting in 2009.
In 2011, at her 5th annual visit, she presented with oedema and discolouration of left lower breast of short duration. Despite her unremarkable annual mammogram, she was scheduled for clinical review in 3 months time. The oedema was still evident, the discolouration had worsened and examination now revealed global breast firmness with extensive skin thickening and eechymosis throughout the left breast. In addition, there was associated blood-filled eruptions at the nipple areolar complex (figures 1 and 2).
Figure 1.
Blood-blistering skin changes suspicious of breast angiosarcoma.
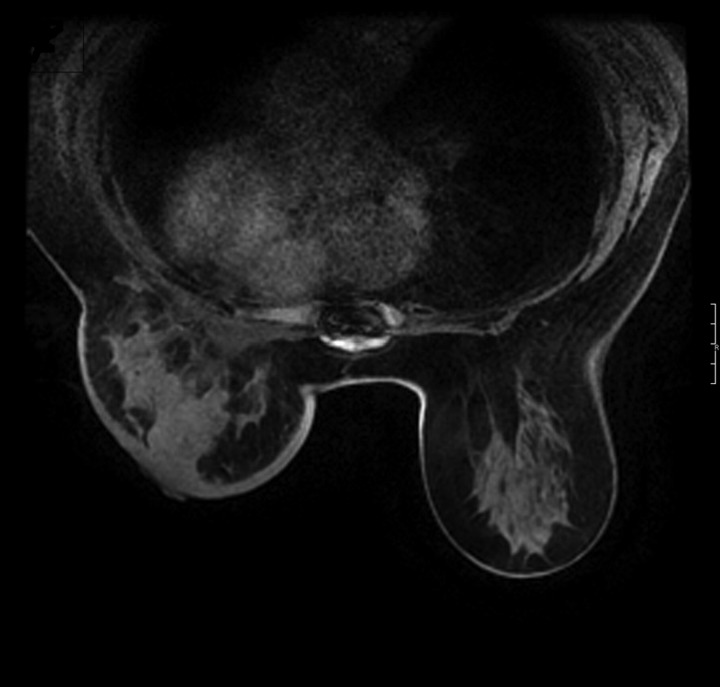
Figure 2.
Breast MRI suspicious of breast angiosarcoma.
Despite the possible aetiology of the patients’ concurrent antiplatelet therapy as a cause of the clinical findings, a high index of suspicion led to a skin punch biopsy which revealed only perivascular lymphocytic infiltrate, a non-specific benign finding. Repeat interval mammogram and ultrasound demonstrated non-specific architectural distortion throughout the left breast. Despite these benign histological and radiological findings a clinical suspicion of angiosarcoma persisted and a breast MRI was performed. This raised the possibility of angiosarcoma of the breast.
Ultrasound-guided core biopsies of the non-specific area of architectural distortion, demonstrated low-grade breast angiosarcoma.
Investigations
| 2006–2010 | Annual normal mammography. |
| 2011 | Nipple areolar complex skin punch biopsy, revealing benign non-specific lymphocytic infiltrate. |
| 2011 | Breast MRI raising possibility of breast angiosarcoma. |
| 2011 | Interval mammogram and breast ultrasound demonstrating indeterminate multifocal architectural distortion. |
| 2011 | Ultrasound biopsy of the architectural distortion, demonstrated low-grade breast angiosarcoma. |
Differential diagnosis
Spontaneous cutaneous eechymosis due to aspirin antiplatelet therapy.
Postradiotherapy benign skin thickening.
Treatment
She underwent a left completion mastectomy in the following week, demonstrating an extensive 150 mm high-grade angiosarcoma (postradiotherapy subtype) of left breast, with clear margins.
Outcome and follow-up
After the left mastectomy the patient made an uneventful recovery. Following multidisciplinary discussion and review of current literature, no role for adjuvant chemotherapy/hormonal/radiotherapy was deemed necessary. Annual clinical review and contralateral surveillance mammography is planned.
Discussion
A similar case was reported, in a 68-year-old woman, 5 years post breast-conserving surgery for a 5 cm node negative invasive ductal cancer. The patient received postoperative radiation therapy and tamoxifen therapy for 5 years. At her fifth annual postoperative visit a cutaneous angiosarcoma was found in the residual breast tissue.2
Secondary angiosarcomas may occur in women who have undergone breast cancer treatment. There are two types, lymphoedema-associated cutaneous angiosarcoma and postirradiation angiosarcoma. Lymphoedema-associated cutaneous angiosarcoma was first described in 1948 by Stewart and Treves3 and the presence of postradiation chronic lymphoedema possibly contributes to its aetiology and may be an early warning sign for potential development. Postirradiation angiosarcoma commonly affects the breast dermis within the radiation field but may develop in the breast parenchyma. Its incidence ranges from 0.09 to 0.16%.4 5
Patients present with areas of skin discolouration, red plaques or nodules which may be mistaken for bruising and may delay the correct diagnosis.2 Skin thickening due to angiosarcoma may be masked or misinterpreted as skin changes that occur after radiation therapy. Establishing a definitive diagnosis may be difficult.
Mammography may reveal a non-specific skin thickening and/or an ill-defined non-calcified superficial mass or focal asymmetry in 33% of cases. Contributing to the difficulty of radiological diagnosis in younger women is the increased density of their breast parenchyma which may obscure visualisation of any mass.6
Breast ultrasound may confirm the presence of a palpable mass with colour Doppler showing hyper-vascularity in some cases.7
Breast MRI has a promising role in diagnosis of angiosarcoma lesions show low-signal intensity with T1 weighting but high-signal intensity in T2 weighting.6 7
Specifically areas of haemorrhage may be correlated to irregular areas of high signal in T1-weighted images. The higher the tumour grade the greater the enhancement, with high-grade angiosarcomas demonstrating rapid enhancement and washout.8 MRI also has a role in detecting residual or recurrent disease after excision. However, the ultimate diagnostic tool remains a core biopsy of the suspicious lesion.9
Clinical course is highly dependent on tumour grade. A low-grade angiosarcoma exhibits an indolent, smouldering clinical course similar to that of benign atypical vascular lesions.10 Conversely, high-grade lesions are characterised by explosive growth and relentless local recurrences within months of radical resection. A poorly differentiated histology is a negative prognostic indicator for patients with angiosarcoma.11 Once a diagnosis is established, the mainstay of treatment is completion mastectomy alone. The role for postoperative radiotherapy remains controversial, with some institutions showing promising early initial results with accelerated hyper-fractionated postoperative radiotherapy.12
In summary, the authors feel the consideration of angiosarcoma as a diagnosis in post breast-conserving surgery radiotherapy patients, presenting with delayed bruising and swelling must be included in the differential clinical diagnosis of astute breast surgeons.
Learning points.
A high index of suspicion will be required to diagnose angiosarcoma.
Imaging studies such as mammograms may have non-specific findings, MRI should be considered.
Concurrent antiplatelet therapy may cause spontaneous bleeding but the appearance of blood blistering is highly suspicious of angiosarcoma in postradiotherapy breast tissue.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Katrina NG, Maureen JM, Reynolds C. Angiosarcoma of the breast. AJR 2008;190:533–8. [DOI] [PubMed] [Google Scholar]
- 2.Majeski J, Austin RM, Fitzgerald RH. Cutaneous angiosarcoma in an irradiated breast after breast conservation therapy for cancer: association with chronic breast lymphoedema. J Surg Oncol 2001;76:239–41. [DOI] [PubMed] [Google Scholar]
- 3.Stewart FW, Treves N. Lymphangiosarcoma in post mastectomy lymphoedema. A report of six cases in elephantiasis chirurgica. Cancer 1948;1:64–81. [DOI] [PubMed] [Google Scholar]
- 4.Marchal C, Weber B, de Lafontan B, et al. Nine breast angiosarcomas after conservative treatment for breast carcinoma: a survey from French comprehensive cancer centres. Int J Radiat Oncol Biol Phys 1999;44:113–19. [DOI] [PubMed] [Google Scholar]
- 5.Strobbe LJ, Peterse HL, van Tinteren H, et al. Angiosarcoma of the breast after conservation therapy for invasive cancer, the incidence and outcome: an unforeseen sequelae. Breast Cancer Res Treat 1998;47:101–9. [DOI] [PubMed] [Google Scholar]
- 6.Liberman L, Dershaw DD, Kaufman RJ, et al. Angiosarcoma of the breast. Radiology 1992;183:649–54. [DOI] [PubMed] [Google Scholar]
- 7.Yang WT, Hennessy BT, Dryden MJ, et al. Mammary angiosarcomas: imaging findings in 24 patients. Radiology 2007;242:725–34. [DOI] [PubMed] [Google Scholar]
- 8.Glazebrook KN, Morton MJ, Reynolds C. Vascular tumors of the breast: mammographic, sonographic, and MRI appearances. AJR 2005;184:331–8. [DOI] [PubMed] [Google Scholar]
- 9.Marchant LK, Orel SG, Perez-Jaffe LA, et al. Bilateral angiosarcoma of the breast on MR imaging. AJR 1997;169:1009–10. [DOI] [PubMed] [Google Scholar]
- 10.Fineberg S, Rosen PP. Cutaneous angiosarcoma and atypical vascular lesions of the skin and breast after radiation therapy for breast carcinoma. Am J Clin Pathol 1994;102:757–63. [DOI] [PubMed] [Google Scholar]
- 11.Rainwater LM, Martin JK, Jr, Gaffney TA, et al. Angiosarcoma of the breast. Arch Surg 1986;121:669–72. [DOI] [PubMed] [Google Scholar]
- 12.Feigenberg SJ, Mendenhall NP, Reith JD, et al. Angiosarcoma after breast-conserving therapy: experience with hyper fractionated radiotherapy. Int J Radiat Oncol Biol Phys 2002;52:620–6. [DOI] [PubMed] [Google Scholar]