Abstract
Background:
Carpal tunnel syndrome (CTS) is a common entrapment neuropathy. Diagnosis of CTS is usually based on a combination of clinical symptoms and electrodiagnostic study (EDS). Ultrasonography (US) also has been shown to be a useful diagnostic tool in CTS and is based on an increase in the median nerve cross-sectional area (CSA) at the level of the pisiform bone. In this study we assessed findings in US in correlation with severity of CTS.
Materials and Method:
This was a cross-sectional case-control study, which was carried out on November 2012 to July 2013. Subjects were chosen from patients who referred to the Alzahra Hospital (Isfahan, Iran). Patients were classified as having mild, moderate, and severe CTS according to EDS and high-resolution US was performed for CSA measurement at the tunnel inlet.
Results:
A total of 87 individuals screened and 52 subjects (81 hands) met all inclusion and no exclusion criteria. The mean ± SD of the CSA was 0.12 ± 0.03 cm2 (range, 0.08–0.18) in mild, 0.15 ± 0.03 cm2 (range, 0.08–0.19) in moderate, and 0.19 ± 0.06 cm2 (range, 0.11–0.32) in severe CTS. We detected a significant correlation between MN CSA and the severity of CTS (P < 0.001).
Conclusion:
In conclusion it is expected that sonography may serve as an additional or complementary method which is useful and reliable in assessing the severity of CTS.
Keywords: Carpal tunnel syndrome, cross-sectional area, median nerve, severity, ultrasonography
INTRODUCTION
Carpal tunnel syndrome (CTS) is a common entrapment neuropathy due to the compression of the median nerve (MN) at the wrist.[1] The prevalence ranges from 1% to 5% among the general population and up to 14.5% among specific occupational groups.[2,3] Early diagnosis is essential in preventing permanent nerve damage and functional sequela.[4] Also, severity of disease is an important clinical factor that may affect the treatment course and prognostic evaluation and should be routinely recorded.[5,6] Diagnosis of CTS is usually based on a combination of clinical symptoms (burning pain, numbness, and nocturnal paresthesia in the distribution of the MN), and signs, such as Tinel sign (tapping over the MN producing dysesthesias) and Phalen sign (wrist flexion producing dysesthesias), and electrodiagnostic study (EDS) [electromyography-nerve conduction studies (EMG-NCS)] which have a sensitivity in the range of 56–85% and a specificity of 94% or higher.[4,7,8,9] However, EDS are time-consuming and expensive, may not be diagnostic in 10–25% of patients with clinical evidence of CTS depending on the severity of disease and the type of nerve conduction techniques used, and false negatives and false positives may occur, even when the most sensitive methods are used.[9,10,11]
Ultrasonography (US) has been shown to be a useful diagnostic tool in CTS and has been used increasingly to confirm a clinical diagnosis of CTS with sensitivity between 44% and 95% and specificity between 57% and 100%.[12,13] It is feasible, simple, relatively low-cost, rapid, accurate, and noninvasive.[14] US diagnosis of CTS is based on an increase in the MN cross-sectional area (CSA) at the level of the pisiform bone.[12]
In this study we survey our findings in US based on measurement of CSA and diameter of MN in mild to severe CTS.
MATERIALS AND METHODS
Subjects
Subjects were chosen from patients who referred to the Alzahra Hospital (Isfahan, Iran). All subjects met the following inclusion criteria: (1) 18-65 years aged; (2) diagnosed clinically with CTS defined according to the criteria of The American Academy of Neurology practice parameters[15,16] and confirmed by EDS (prolonged MN distal motor latencies >4.4 ms or prolonged MN distal sensory latencies >3.5 ms);[17] (3) written informed consent. Subjects also met none of the following exclusion criteria: (1) History of prior carpal tunnel release procedure; (2) history of trauma to the wrist or hand that included broken bones; (3) known history of other neurologic disorders such as polyneuropathy, proximal median or ulnar neuropathy, plexopathy, mononeuritis multiplex and cervical radiculopathy, or cervical spondylosis; (4) pregnancy or being within 3 months postpartum for women.
Design and procedures
This was a cross-sectional case-control study, which carried out from November 2012 to July 2013. The study followed the Declaration of Helsinki on Biomedical Research Involving Human Subjects and was approved by the Ethics Committee from the Isfahan University of Medical Sciences. All participants provided written informed consent. Demographic data included age, height, and sex. Patients were classified as having mild, moderate, and severe CTS according to these criteria[18]:
Mild: Prolonged DSL and/or median mixed nerve latency (MNL); normal DML; amplitudes of all responses within normal range; no conduction block (CB) or mild CB; and no thenar EMG abnormalities (if tested)
Moderate: Prolonged DSL, MNL, and DML (if all tested); Amplitudes of all tested responses may be diminished, typically a relative decrease (but not required); CB may be present; and minor thenar EMG abnormalities may be present (if tested)
Severe: Unobtainable median sensory nerve action potentials (or low amplitude and prolonged DSL); low-amplitude or unobtainable median mixed nerve response and, if present, prolonged MNL; low-amplitude or unobtainable median compound muscle action potential and, if present, prolonged DML; CB may be present and pronounced (i.e. >70%); and thenar EMG abnormalities often present (if tested).
Assessments
High-resolution US were performed using a scanner with a 13-MHz linear array transducer for the carpal tunnel study and measuring of CSA (Sonosite machine). During the examination, the patient sat in a comfortable position facing the examiner, with the measured forearm resting on the table, the palm supine, and fingers semi-extended in the neutral position.[19] Since previous reports demonstrated that the CSA of the MN at the carpal tunnel inlet is the best discriminatory criterion with which to identify patients with CTS, so in the present study, the CSA measurement was obtained at the tunnel inlet (just before the proximal margin of the flexor retinaculum)[20] [Figure 1]. The MN was imaged in a longitudinal scan first, placing the US probe at the midline between the radius and ulna with the center of the probe at the distal wrist crease, to obtain an initial general overview of the MN which was then used to assist the examiner in order to obtain optimal axial (cross-sectional) images. Then a transverse scan, keeping the probe directly perpendicular to the long axis of the MN in order to ensure that the area measured indeed reflected a CSA, was performed to record the CSA (calculated by continual tracing of the nerve circumference, excluding the hyperechoic epineurial rim) and elliptical (the transverse and the anteroposterior) diameters (DMN).[21]
Figure 1.
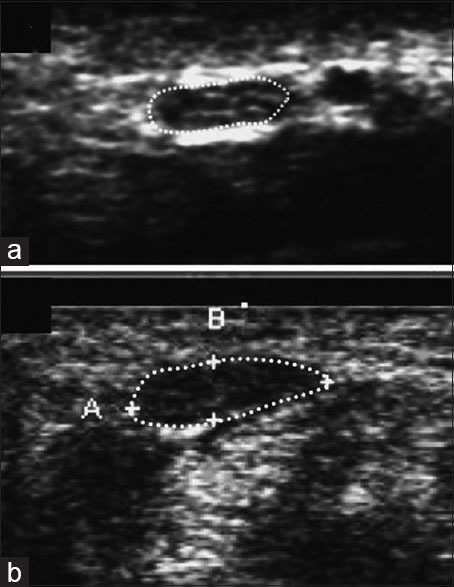
(a) Transverse view of sonogram of the median nerve at the carpal tunnel inlet in a healthy subject. The outer margin of the median nerve is surrounded by a dotted line. (b) Transverse view of sonogram of the median nerve at the carpal tunnel inlet in a subject with carpal tunnel syndrome. The nerve is relatively hypoechogenic
Statistical methods
Data were analyzed by SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). A P < 0.05 was considered significant. Continuous variables were expressed as mean ± SD. ANOVA and Pierson correlation were used for analysis.
RESULTS
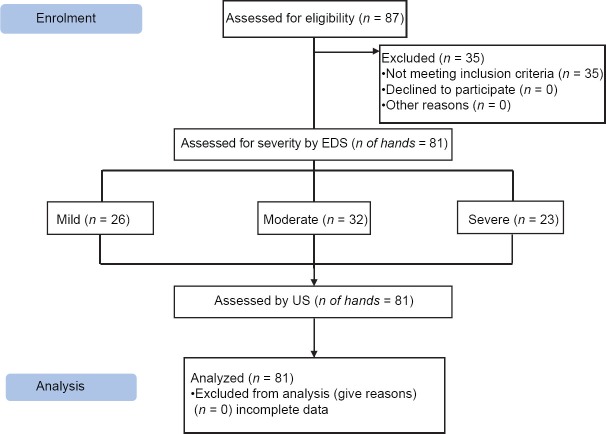
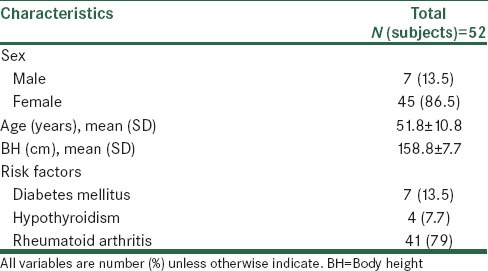
A total of 87 individuals were screened and 52 subjects (81 hands) met all inclusion and no exclusion criteria and were divided into three subgroups according to severity of CTS [Figure 2]. Twenty-six hands (32.1%) were affected with mild CTS, 32 (39.5%) with moderate CTS, and 23 (38.4%) with severe disease. The demographic data of the 52 participants (81 hands) are shown in Table 1.
Figure 2.
Study design flowchart
Table 1.
Demographic data of the 52 participants (81 hands)
The mean ± SD of the CSA was 0.12 ± 0.03 cm2 (range, 0.08–0.18) in mild, 0.15 ± 0.03 cm2 (range, 0.08–0.19) in moderate, and 0.19 ± 0.06 cm2 (range, 0.11–0.32) in severe CTS. We detected a significant correlation between MN CSA and the severity of CTS (P < 0.001) [Table 2].
Table 2.
Between group ANOVA analysis of CSA and DMD in different severity subgroups
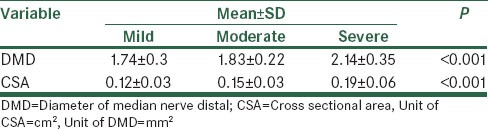
The mean ± SD of the diameter of MN (DMN) was 1.74 ± 0.3 (range, 1.19–2.51) in mild CTS, 1.83 ± 0.22 (range, 1.51–2.44) in moderate, and 2.14 ± 0.35 (range, 1.54–2.90) in severe CTS. We detected a significant correlation between DMN and the severity of CTS (P < 0.001).
Also Pierson correlation showed that there is a strait correlation between CAS and DMN (r = 0.73, P < 0.001).
DISCUSSION
Some authors consider that the role of US in diagnosis of CTS is yet to be proven[22] and other stated that US appears to be of little use in the diagnosis of CTS.[14] By contrast, Wong et al.[23] proposed an algorithm involving initial US examination of patients suspected of having CTS and secondary EDS performed only when US results were negative. Furthermore, one study stated that US could be used to grade the severity of CTS.[17] One meta-analysis was performed to determine the sensitivity and specificity of ultrasound in the diagnosis of CTS and the authors concluded that although ultrasound may not replace electrodiagnostic testing, it may be a feasible alternative to electrodiagnostic testing as a first-line confirmatory test.[5] Another recent meta-analysis confirmed that US, using cross-sectional area of the MN, could give complementary results for diagnosis of CTS.[24] Some authors showed that as neurophysiologic severity of CTS increases, there is increasing US abnormality and US can also be helpful in advanced CTS with severe abductor pollicis brevis muscle atrophy where NCS shows no more response.[25,26]
This study assessed the correlation between MN CSA and the severity of CTS. The results provide preliminary evidence that MN CSA was correlated with the severity of CTS based on the nerve conduction velocity studies and with increasing the sevierity of CTS, CSA would be enlarged. This finding is consistent with Miwa et al. and Ajeena et al. studies which confirmed that the MN CSA is enlarged in patients with CTS and it correlated with the severity of CTS.[14,20] Karadag et al. stated that the US was useful in grading the severity of CTS. They concluded that US measurement of CSA could give information about severity of MN involvement and they set US cut-off points that discriminate between different grades of CTS severity as follows: 10.0–13.0 mm2 for mild, 13.0–15.0 mm2 for moderate, and >15.0 mm2 for severe symptoms.[27] In our study these ranges were nearly similar: 12 ± 3 mm2 for mild, 15 ± 3 mm2 for moderate and 19 ± 6 mm2 for sever CTS. In the other hand, Moran et al., reported that the CSA of the MN at the tunnel inlet were 10.8 ± 1.9 mm2, 11.4 ± 1.8 mm2, and 12 ± 1.5 mm2 in patients with mild, moderate, and severe CTS, respectively. They reported that their clinical groups differed significantly from their control group (5.8 ± 0.9 mm2), but they found no differences between the patient groups.[28] This is in against with our findings. And Mohammadi et al. also asserted that US cannot be used to grade the severity of CTS.[29] But, El Miedany et al. and Lee et al. found that one can be confident of determining the level of severity of CTS based on US measurement of CSA of the MNs. In their work, they reported that US measurements of greater than 15 mm2 correlate with NCS findings of moderate to severe disease and noted that these figures differ significantly from those patients with mild to moderate disease.[30,31]
In our study there was also a strait correlation between MN DMN and the severity of CTS. All these findings suggest that CTS can be objectively stratified in terms of disease severity and such stratification may lead clinical decisions in terms of treatment and prognosis and also be consistent with previous reports that demonstrated the utility of US measurement of MN CSA at the tunnel inlet as a good alternative to NCS for the initial diagnosis of CTS.[17,18]
It is interesting that many studies showed the lack of interreader reliability of the CSA measurements obtained at the tunnel outlet, because MN may be difficult to be seen at outlet in persons with thick palmar skin and it has a wide variation as it usually splits into digital branches here.[17,23] That is why the current study used measurements of the CSA of the MN at the tunnel inlet despite the findings of Mohammadi et al., in 2009, about the usefulness of measuring CSA of the MN at the tunnel outlet.[29]
In conclusion it is expected that sonography may serve as an additional or complementary method for investigation of CTS. But EDX findings are more accurate in comparison to ultrasound, which is more dependent on examiner experience. The MN is easily visualized and measuring its CSA at the level of pisiform bone is a useful noninvasive method that is reliable in assessing the severity of CTS and might reveal some of its possible causes as space-occupying lesion or anatomical variation of the MN.
Footnotes
Source of Support: This work was supported by Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Wilbourn AJ. Diabetic entrapment and compression neuropathies. In: Dyck PJ, Thomas PK, editors. Diabetic neuropathy. Philadelphia: Saunders; 1999. pp. 481–508. [Google Scholar]
- 2.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153–8. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Roquelaure Y, Ha C, Pelier-Cady MC, Nicolas G, Descatha A, Leclerc A, et al. Work increases the incidence of carpal tunnel syndrome in the general population. Muscle Nerve. 2008;37:477–82. doi: 10.1002/mus.20952. [DOI] [PubMed] [Google Scholar]
- 4.Klauser AS, Halpern EJ, De Zordo T, Feuchtner GM, Arora R, Gruber J, et al. Carpal tunnel syndrome assessment with US: Value of additional cross-sectional area measurements of the median nerve in patients versus healthy volunteers. Radiology. 2009;250:171–7. doi: 10.1148/radiol.2501080397. [DOI] [PubMed] [Google Scholar]
- 5.Descatha A, Huard L, Duval S. Letter to the editor: The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: A meta-analysis. Clin Orthop Relat Res. 2011;469:901–2. doi: 10.1007/s11999-010-1761-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowler JR, Gaughan JP, Ilyas AM. The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: A Meta analysis. Clin Orthop Relat Res. 2011;469:1089–94. doi: 10.1007/s11999-010-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. Muscle Nerve. 2002;25:918–22. doi: 10.1002/mus.10185. [DOI] [PubMed] [Google Scholar]
- 8.Sarría L, Cabada T, Cozcolluela R, Martínez-Berganza T, García S. Carpal tunnel syndrome: Usefulness of sonography. Eur Radiol. 2000;10:1920–5. doi: 10.1007/s003300000502. [DOI] [PubMed] [Google Scholar]
- 9.Jablecki CK, Andary MT, Floeter MK, Miller RG, Quartly CA, Vennix MJ, et al. Practice parameter: Electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589–92. doi: 10.1212/wnl.58.11.1589. [DOI] [PubMed] [Google Scholar]
- 10.Lew HL, Date ES, Pan SS, Wu P, Ware PF, Kingery WS. Sensitivity, specificity, and variability of nerve conduction velocity measurements in carpal tunnel syndrome. Arch Phys Med Rehabil. 2005;86:12–6. doi: 10.1016/j.apmr.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 11.Atroshi I, Gummesson C, Johnsson R, Ornstein E. Diagnostic properties of nerve conduction tests in population-based carpal tunnel syndrome. BMC Musculoskelet Disord. 2003;4:9. doi: 10.1186/1471-2474-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beekman R, Visser LH. Sonography in the diagnosis of carpal tunnel syndrome: A critical review of the literature. Muscle Nerve. 2003;27:26–33. doi: 10.1002/mus.10227. [DOI] [PubMed] [Google Scholar]
- 13.Seror P. Sonography and electrodiagnosis in carpal tunnel syndrome diagnosis, an analysis of the literature. Eur J Radiol. 2008;67:146–52. doi: 10.1016/j.ejrad.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Ajeena IM, Al-Saad RH, Al-Mudhafar A, Hadi NR, Al-Aridhy SH. Ultrasonic assessment of females with carpal tunnel syndrome proved by nerve conduction study. Neural Plast. 2013;2013:754564. doi: 10.1155/2013/754564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Practice parameter for carpal tunnel syndrome (summary statement): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1993;43:2406–9. [PubMed] [Google Scholar]
- 16.You H, Simmons Z, Freivalds A, Kothari MJ, Naidu SH. Relationships between clinical symptom severity scales and nerve conduction measures in CTS. Muscle Nerve. 1999;22:497–501. doi: 10.1002/(sici)1097-4598(199904)22:4<497::aid-mus11>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 17.Wong SM, Griffith JF, Hui AC, Tang A, Wong KS. Discriminatory sonographic criteria for the diagnosis of carpal tunnel syndrome. Arthritis Rheum. 2002;46:1914–21. doi: 10.1002/art.10385. [DOI] [PubMed] [Google Scholar]
- 18.Sucher BM. Grading severity of carpal tunnel syndrome in electrodiagnostic reports: Why grading is recommended. Muscle Nerve. 2013;48:331–3. doi: 10.1002/mus.23824. [DOI] [PubMed] [Google Scholar]
- 19.Kuo MH, Leong CP, Cheng YF, Chang HW. Static wrist position associated with least median nerve compression: Sonographic evaluation. Am J Phys Med Rehabil. 2001;80:256–60. doi: 10.1097/00002060-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Miwa T, Miwa H. Ultrasonography of Carpal Tunnel Syndrome: Clinical Significance and Limitations in Elderly Patients. Intern Med. 2011;50:2157–61. doi: 10.2169/internalmedicine.50.5771. [DOI] [PubMed] [Google Scholar]
- 21.Chen SF, Huang CR, Tsai NW, Chang CC, Lu CH, Chuang YC, et al. Ultrasonographic assessment of carpal tunnel syndrome of mild and moderate severity in diabetic patients by using an 8-point measurement of median nerve cross-sectional areas. BMC Med Imaging. 2012;12:15. doi: 10.1186/1471-2342-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prime MS, Palmer J, Khan WS, Goddard NJ. Is there light at the end of the tunnel? Controversies in the diagnosis and management of carpal tunnel syndrome. Hand (N Y) 2010;5:354–60. doi: 10.1007/s11552-010-9263-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: Diagnostic usefulness of sonography. Radiology. 2004;232:93–9. doi: 10.1148/radiol.2321030071. [DOI] [PubMed] [Google Scholar]
- 24.Descatha A, Huard L, Aubert F, Barbato B, Gorand O, Chastang JF. Meta-Analysis on the Performance of Sonography for the Diagnosis of Carpal Tunnel Syndrome. Semin Arthritis Rheum. 2012;41:914–22. doi: 10.1016/j.semarthrit.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Pastare D, Therimadasamy AK, Lee E, Wilder-Smith EP. Sonography versus nerve conduction studies in patients referred with a clinical diagnosis of carpal tunnel syndrome. J Clin Ultrasound. 2009;37:389–93. doi: 10.1002/jcu.20601. [DOI] [PubMed] [Google Scholar]
- 26.Nakamichi K, Tachibana S. Ultrasonographic measurement of median nerve cross-sectional area in idiopathic carpal tunnel syndrome: Diagnostic accuracy. Muscle Nerve. 2002;26:798–803. doi: 10.1002/mus.10276. [DOI] [PubMed] [Google Scholar]
- 27.Karadağ YS, Karadağ O, Ciçekli E, Oztürk S, Kiraz S, Ozbakir S. Severity of carpal tunnel syndrome assessed with high frequency ultrasonography. Rheumatol Int. 2010;30:761–5. doi: 10.1007/s00296-009-1061-x. [DOI] [PubMed] [Google Scholar]
- 28.Moran L, Perez M, Esteban A, Bellon J, Arranz B, del Cerro M. Sonographic measurement of cross-sectional area of the median nerve in the diagnosis of carpal tunnel syndrome: Correlation with nerve conduction studies. J Clin Ultrasound. 2009;37:125–31. doi: 10.1002/jcu.20551. [DOI] [PubMed] [Google Scholar]
- 29.Mohammadi A, Afshar AR, Masudi S, Etemadi A. Comparison of high resolution ultrasonography and nerve conduction study in the diagnosis of carpal tunnel syndrome: Diagnostic value of median nerve cross-sectional area. Iran J Radiol. 2009;3:47–152. [Google Scholar]
- 30.El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: Substantive or complementary tests? Rheumatology (Oxford) 2004;43:887–95. doi: 10.1093/rheumatology/keh190. [DOI] [PubMed] [Google Scholar]
- 31.Lee D, van Holsbeeck MT, Janevski PK, Ganos DL, Ditmars DM, Darian VB. Diagnosis of carpal tunnel syndrome: Ultrasound versus electromyography. Radiol Clin North Am. 1999;37:859–72. doi: 10.1016/s0033-8389(05)70132-9. [DOI] [PubMed] [Google Scholar]