Abstract
A 70-year-old Greek lady presented with fever, arthralgias of knees, cervical and lumbar pain during the last month. On clinical examination the patient was found to have tenderness of the cervical and the lumbar spine with great motion restriction. The blood tests revealed high erythrocyte sedimentation rate and C-reactive protein, abnormal liver function tests and a positive rheumatoid factor. Serological test for Brucella was positive while cervical MRI revealed epidural abscess and spondylodiscitis. Conservative treatment with streptomycin (it was substituted by rifampicin after the third week) and doxycyclin for 4 months significantly improved her symptoms. The frequency as well as the diagnosis and management of this manifestation are discussed.
Background
Brucellosis, an endemic zoonosis in many countries, is caused by bacteria of the genus Brucella, a Gram-negative coccobacillus. More than 500 000 cases are reported yearly to the World Health Organisation.1 Brucella melitensis is the most common species and is distributed primarily in the Mediterranean region followed by Brucella abortus, Brucella suis and Brucella canis. Brucellae are transmitted to humans by consumption of unpasteurised milk or dairy products or by direct contact with infected animals. More than half of the cases worldwide occur in the meat-processing industry. Brucellosis may present as a subclinical illness, as an acute disease with general manifestations or as a localised disease affecting any organ system. Osteoarticular involvement is one of the most common complications, occurring in up to 40% of cases. It may present as arthritis, synovitis, sacroiliitis, spondylitis or osteomyelitis and all age groups may be affected. Spondylitis as well as epidural abscess most commonly affect the lumbar spine while the cervical spine is infrequently affected.
A case of a patient with spondylodiscitis and cervical epidural abscess due to Brucella is described here.
Case presentation
A 70-year-old, Greek-ruralist lady presented to our department with fever (up to 38°C), started 2 days before. She complained of transient swelling of both knees, a few episodes of nocturnal sweats and cervical and lumbar pain with gradual deterioration during the last month. Her medical history included arterial hypertension, brucellosis 30 years ago (presented with fever, arthralgias and loss of weight) and a chronic lumbar pain that needed frequent use of non-steroidal anti-inflammatory drugs. Her main occupation was that of a farmer and sheep-breeding. Clinical examination revealed an intense tenderness of the cervical and the lumbar spine with great motion restriction. There were no neurological deficits such as sensory or motor disturbances or reduced tendon reflexes. Peripheral lymph nodes, liver and spleen were not palpable. Heart and lung auscultation as well as the rest of the examination were normal.
Investigations
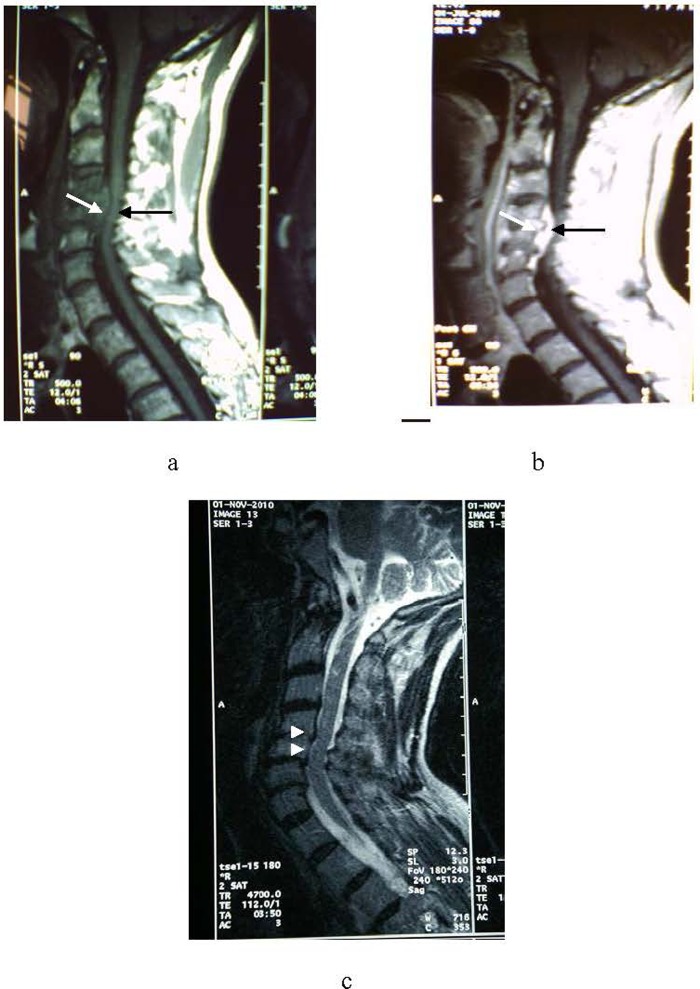
The blood tests revealed white cell count: 6.100/μl with 600 mononuclear cells, Ht: 35.4%, haemoblobin: 11.9 g/dl, aspartate aminotransferase: 71 IU/l, alanine aminotransferase: 38 IU/l, alkaline phosphatase: 167 IU/l (normal range 35–125 IU/l), erythrocyte sedimentation rate (ESR):80 mm/h, C-reactive protein (CRP): 8.2 mg/dl (normally <0.5 mg/dl), negative Coombs’ test, creatine phosphokinase: 672 IU/l, rheumatoid factor:132 IU/ml, a negative Wright test, ferritin: 106 ng/ml, antibodies against Brucella (IgG: positive with ratio 1.8 and IgM: negative with ratio 0.7 (negative <0.9)), toxoplasma (IgG and IgM negative), Epstein Barr (IgG: positive and IgM: negative). Chest x-ray was normal and Mantoux test was negative. Blood cultures were negative for aerobic or anaerobic bacteria. An ultrasound of the abdomen showed mild liver and spleen enlargement whereas a lumbar MRI showed degenerative findings and mild disc herniations. A cervical MRI showed spondylodiscitis at the C4–C5 level with an epidural abscess (of approximately 2.5 cm diameter) compressing the spinal cord, despite the absence of neurological symptoms and normal neurological examination (figure 1A, B).
Figure 1.
MRI of cervical spine before (A,B) and after (C) treatment. Spondylodiscitis of C4–C5 vertebrae (white arrow) was found and epidural abscess (black arrow) at the same level was compressing the spinal cord before (A) and after (B) gadolinium contrast. After treatment (C), both spondylodiscitis and epidural abscess were greatly improved (white arrows) with decompression of the spinal cord.
Differential diagnosis
Differential diagnosis of an epidural abscess must include all the infections caused by bacteria or fungi, such as Staphylococcus aureus, Mycobacterium tuberculosis, Pseudomonas sp., Escherichia coli, Candida sp., Actinobacillus sp., Salmonella enteritidis, Nocardia sp. or Brucella.
Treatment
Despite the negative tests for Brucella and because of her medical and occupational history (sheep-breeding, previous history of brucellosis, symptoms and high ESR) she was started on an empirical treatment with intramuscular injections of streptomycin (1 g/day) combined with doxycycline (100 mg twice daily orally). After the third week of treatment, streptomycin was substituted by rifampicin (900 mg/day).
Outcome and follow-up
Fever gradually declined after the second day with a parallel improvement of lumbar pain. Blood tests were repeated 10 days later. Antibodies against Brucella were now positive (IgG 70 IU (negative <30) and IgM 46 IU (negative <20), ELISA test), mononuclear cells were 1200/μl, ESR: 16 mm/h, CRP: 0.7 mg/dl and ferritin:30 ng/ml. The cervical pain as well as the movement ability of the cervical spine gradually improved. The patient was referred to the neurosurgery department for further evaluation. She was treated conservatively for 4 months with great improvement of the epidural abscess and decompression of the spinal cord (figure 1C).
Discussion
Brucellosis is a systemic disease with manifestations from many organ systems. Osteoarticular disease is very common and usually is presented as sacroiliitis, arthritis, osteomyelitis or spondylodiscitis. In the case of spinal cord involvement the main symptoms are back pain (100%), weakness (69%), fever (66%), weight loss and anorexia (57%), sweats and arthralgias (54%) and neurological deficits (46%).2 Frequency of spondylodiscitis and/or epidural abscess varies in different studies. In a study with 152 patients with brucellosis, 22 (14.5%) had spondylitis while 3 (2%) of them had abscess formation.3 In another study with 135 patients, 31 (23%) had spondylitis and 19 (14%) had an abscess.4
In general, it is estimated that epidural abscess is responsible for 1 or 2 of every 10 000 admissions. The most common cause is S aureus whereas Brucella spp. is the aetiological factor for only 0.1% of the cases. Risk factors for this uncommon presentation are immunosuppression (diabetes mellitus, alcoholism, chronic renal failure and cancer), spinal procedures or trauma. Diagnosis is based on isolation of Brucella organisms in blood, bone marrow or involved tissue cultures. Nevertheless, culture of Brucella spp. is difficult and bacteraemia is intermittent, especially in chronic cases. Positive serology (titre >1 : 160) or a four-fold rise in antibody titres from the baseline is also considered definite. Turgut et al5 suggested that diagnosis of brucellosis may be established based on the presence of at least two of the following criteria: clinical picture compatible with brucellosis, positive serology, radiological findings suggesting infectious vertebral involvement, isolation of Brucella in blood or tissue samples, histological findings of chronic inflammation and non-caseating granulomatous tissue.
Most epidural abscesses are located posteriorly in the thoracic and the lumbar spine. Anterior epidural abscesses are usually related with spondylodiscitis or osteomyelitis. A few case reports and retrospective studies have been published reporting patients with epidural abscesses, mainly lumbar and thoracic, while cervical abscesses are quite rare.6 7 Pina et al8 reported four cases of cervical epidural abscess whereas Sengul et al,9 Ates et al,10 Basaranoglu et al11 and Güzey et al12 reported one case each. Görgülü et al13 reported nine cases of epidural abscess, but only one was located in the cervical spine and Bodur et al14 reported four cases.
Management of spinal brucellosis is not standard and drug selection, duration of treatment and the role of surgery remain controversial. Most authors suggest a combination of two antibiotics, rifampicin plus doxycyclin while others recommend the addition of aminoglycosides in severe cases. The duration of treatment varies from 6 weeks to 1 year depending on clinical improvement. Surgical intervention is recommended for cases with spinal cord compression or neurological deficits.15
Our case diagnosis was based on clinical manifestations, positive serology and MRI findings. It is worth mentioning that serology investigation for Brucella was initially negative and became positive 10 days after initiation of the treatment. It is well known that serology tests may be negative during the first day or week and become positive later during the course of the disease. There are also published case reports where serology tests were persistently negative and diagnosis was based on blood cultures and biopsy specimens.16 Thus, negative blood tests must not definitely exclude diagnosis of brucellosis and they should be repeated a couple of weeks later. After initiation of a combined regimen, an obvious clinical and laboratory improvement was noticed. We preferred a combination of two regimens instead of three as there were no neurological deficits and a prompt response was noticed. Nevertheless, the patient was referred to a neurosurgery department as sudden neurological deterioration may occur despite the initial response to conservative treatment. Difficulties in the diagnosis and delay of appropriate treatment may lead to permanent neurological complications. Brucellosis must always be considered as a possible diagnosis in patients with spinal cord pain, especially in endemic areas.
Learning points.
Brucellosis must always be considered as a possible diagnosis in patients with fever and spinal cord pain.
Cervical epidural abscess is a very rare manifestation of brucellosis.
Permanent neurological complications may occur in these patients if treatment is delayed.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Salata RA. Brucellosis. In: Goldman L, Ausiello D, eds. Cecil textbook of medicine. Philadelphia, Pennsylvania, USA: Saunders, 2004:1887–90. [Google Scholar]
- 2.Solera J, Lozano E, Martínez-Alfaro E, et al. Brucellar spondylitis: review of 35 cases and literature survey. CID 1999;29:1440–9. [DOI] [PubMed] [Google Scholar]
- 3.Bozgeyik Z, Ozdemir H, Demirdag K, et al. Clinical and MRI findings of brucellar spondylodiscitis. Eur J Radiol 2008;67:153–8. [DOI] [PubMed] [Google Scholar]
- 4.Kaptan F, Gulduren HM, Sarsilmaz A, et al. Brucellar spondylodiscitis: comparison of patients with and without abscesses. Rheumatol Int. Published Online First: 29 July 2012. doi:10.1007/s00296-012-2491-4. [DOI] [PubMed] [Google Scholar]
- 5.Turgut M, Turgut A, Kosar U. Spinal brucellosis: Turkish experience based on 452 cases published during the last century. Acta Neurochir (Wien) 2006;148:1033–44. [DOI] [PubMed] [Google Scholar]
- 6.Uqarriza LF, Porras LF, Lorenzana LM, et al. Brucellar spinal epidural abscesses. Analysis of eleven cases . Br J Neurosurg 2005;19:235–40. [DOI] [PubMed] [Google Scholar]
- 7.Bozgeyik Z, Ozdemir H, Demirdag K, et al. Clinical and MRI findings of brucellar spondylodiscitis. Eur J Radiol 2008;67:153–8. [DOI] [PubMed] [Google Scholar]
- 8.Pina MA, Modrego PJ, Uroz JJ, et al. Brucellar spinal epidural abscess of cervical location: report of four cases. Eur Neurol 2001;45:249–53. [DOI] [PubMed] [Google Scholar]
- 9.Sengul G, Akar A, Alper F, et al. Nonsurgically treated cervical brucellar epidural abscess causing spinal cord compression. J Clin Neurosci 2008;15:1411–14. [DOI] [PubMed] [Google Scholar]
- 10.Ates O, çayli SR, Koçak A, et al. Spinal epidural abscess caused by brucellosis: two case reports. Neurol Med Chir (Tokyo) 2005;45:66–70. [DOI] [PubMed] [Google Scholar]
- 11.Basaranoglu M, Mert A, Tabak F, et al. A case of cervical Brucella spondylitis with paravertebral abscess and neurological deficits. Scand J Infect Dis 1999;31:214–15. [DOI] [PubMed] [Google Scholar]
- 12.Güzey FK, Emel E, Sel B, et al. Cervical spinal brucellosis causing epidural and prevertebral abscesses and spinal cord compression : a case report. Spine J 2007;7:240–4. [DOI] [PubMed] [Google Scholar]
- 13.Görgülü A, Albavrak BS, Görgülü E, et al. Spinal epidural abscess due to Brucella. Surg Neurol 2006;66:141–6. [DOI] [PubMed] [Google Scholar]
- 14.Bodur H, Erbay A, Colpan A, et al. Brucellar spondylitis. Rheumatol Int 2004;24:221–6. [DOI] [PubMed] [Google Scholar]
- 15.Katonis P, Tzermiadianos M, Gikas A, et al. Surgical treatment of spinal brucellosis. Clin Orthop Relat Res 2006;444:66–72. [DOI] [PubMed] [Google Scholar]
- 16.Celik AD, Yulugkural Z, Kilincer C, et al. Negative serology: could exclude the diagnosis of brucellosis? Rheumatol Int 2012;32:2547–9. [DOI] [PubMed] [Google Scholar]