Abstract
Here, we present a case of a severe acute disseminated encephalomyelitis (ADEM) of a 42-year-old male patient. The diagnosis was established after brain biopsy and due to acutely evolving encephalopathy occurring in the context of atypical Mycoplasma pneumoniae (MP). We analysed the prominent MRI white matter lesions using a three-dimensional algorithm as cutting-edge technique to study morphological abnormalities and correlated them to the clinical condition of the patient. We found a discrepancy between the lesion size and the clinical deficits of the patient, actually the clinical improvement antedated the regression of the white matter lesions.
Background
This remarkable case may remind readers to keep in mind diagnosis of an acute disseminated encephalomyelitis (ADEM) in young patients developing central neurological symptoms after an infectious illness or after vaccination. In this particular severe case, we present reconstructions of extensive white matter lesions as well as correlation of lesion development with the clinical score of the patient.
Case presentation
A 42-year-old man was referred to our hospital with severe bronchitis and pneumonia which had persisted for 3 weeks despite oral antibiotic treatment with doxycycline followed by ciprofloxacine.
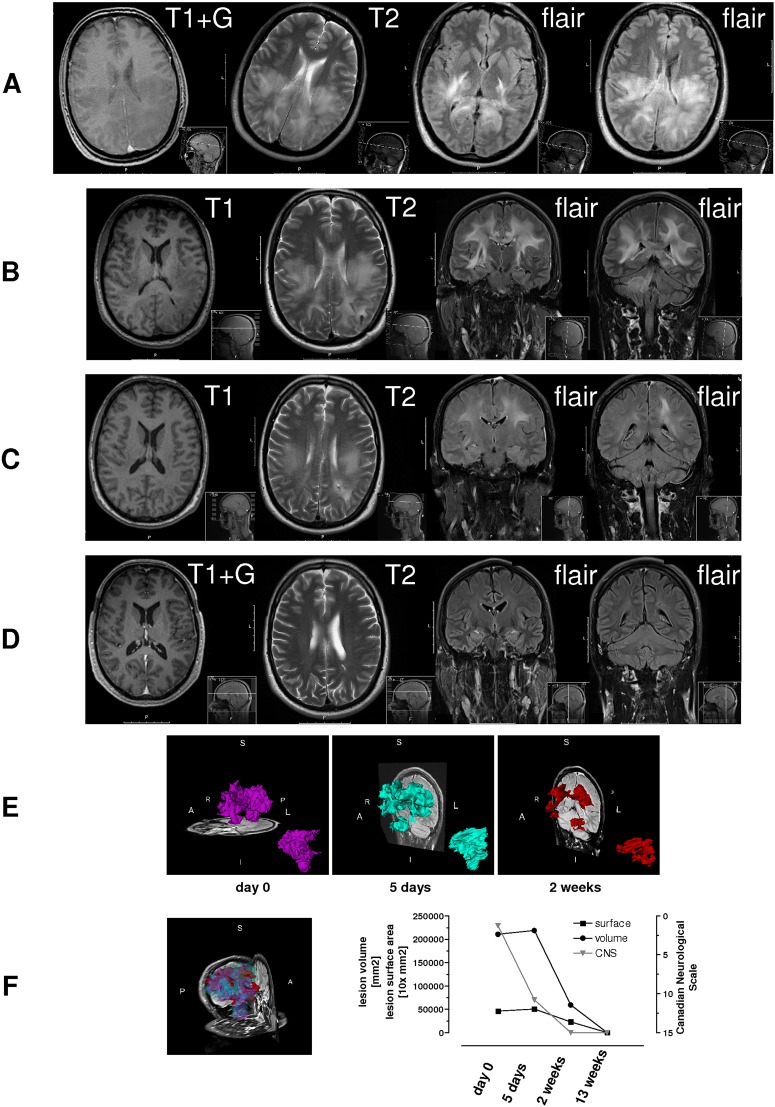
He developed progressive neurological symptoms encompassing dizziness, postural instability, psychomotor slowing and latent weakness of the upper limbs. According to the Canadian Neurological Score1 (CNS) the patient was clinically seriously affected with an initial score of 1.5 points (figure 1F). An MR scan of the brain revealed impressive widespread supratentorial and infratentorial subcortical T2 hyperintense white matter lesions along the tracts with a space-occupying effect and a slight gadolinium enhancement (figure 1A).
Figure 1.
(A) Initial MR scan with gadolinium showing extensive supratentorial and infratentorial, subcortical T2 hyperintense white matter lesions along the tracts. Lesions exhibit a space-occupying effect and a slight gadolinium enhancement. (B) Follow-up after 5 days: MRI changes are more prominent and T2-signal lesions intensified, corresponding to the flair and signal attenuation in T1, localised infratentorially and supratentorially. (C) Follow-up after 2 weeks: regressive MRI changes. (D) Completely normal after 13 weeks (with gadolinium). (E) Development of white matter lesion at different time points as shown in (A–D). (F) Left: merging of lesion size. Right: Graph represents the clinical development of the patient according to the Canadian Neurological Scale (CNS). Severity of neurological symptoms can be categorised as follows: mild (CNS≥8), moderate (score of 5–7) and severe (score of 1–4). Clinical improvement precedes the morphological regression more than 1 week.
Cerebrospinal fluid analysis showed a lympho-monocytic pleocytosis (129 cells/µl, 92 mg/dl protein). PCR, microbiological and serological study findings were negative, including tests for fungi, viruses and bacteria. No specific aetiology could be identified. Since the patient's condition worsened, a broad therapy with rocephine, acyclovir, clarithoromycine and high-dose steroids was initiated. Developing seizures were treated successfully with valproic acid. Stereotactic brain biopsy revealed slight oedema, reactive astrocytic gliosis and microglial activation as well as single perivascular lymphocytes. There was no evidence for vasculitis, brain abscess, glioma, carcinoma or lymphoma.
Blood tests revealed a positive titre with falling kinetics for Mycoplasma pneumoniae (MP), a positive direct Coombs test and the presence of cold agglutinins. A retrospective evaluation of the initial outpatient chest x-ray revealed atypical pneumonia; therefore, the diagnosis of MP-induced ADEM was made.
Under high-dose steroid treatment, symptoms resolved over 5 days. The patient was without residual neurological deficits after 2 weeks. The follow-up MRI after 5 days still showed a progress in the number and size of the white matter lesions (figure 1B). The volume and surface area of the lesion at different time points was calculated and displayed (figure 1E,F). The MRI 2 weeks after clinical onset showed its diminution (figure 1C,E,F). The MR scan, 13 weeks after onset was completely normal (figure 1D,F).
Discussion
There is consensus that diagnosis of ADEM requires exclusion of other causes and in very atypical cases may necessitate a brain biopsy. In this case, the acutely evolving encephalopathy occurring in the context of an atypical pneumonia caused by MP established the diagnosis.
By definition, ADEM is a monophasic condition. Up to 75% of all cases occur after an infectious illness or vaccination. MP has been identified as one of the infectious triggers of the disease.2–4 Direct invasion of the central nervous system by MP or immune-mediated damage due to a previous MP infection have been invoked as pathogenic mechanisms.5
Three-dimensional lesion measurements, quantification of the patient's deficits and correlation of both parameters provides evidence that the development of the lesion size was still increasing, while the clinical condition of the patient was already improving. It is noteworthy that—as in this case—in ADEM, there can be a remarkable discrepancy between the severe MR changes and the clinical deficits, and the morphological aberration lags behind the clinical improvement.
Learning points.
Acute disseminated encephalomyelitis (ADEM) is a diagnosis of exclusion.
ADEM may occur in the context of atypical Mycoplasma pneumoniae (MP).
MRI abnormalities may be discrepant to the clinical deficits of the patient.
In our case the clinical improvement antedated the regression of the white matter lesions.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Cote R, Battista RN, Wolfson C, et al. The Canadian Neurological Scale: validation and reliability assessment. Neurology 1989;39:638–43. [DOI] [PubMed] [Google Scholar]
- 2.Menge T, Kieseier BC, Nessler S, et al. Acute disseminated encephalomyelitis: an acute hit against the brain. Curr Opin Neurol 2007;20:247–54. [DOI] [PubMed] [Google Scholar]
- 3.Tenembaum S, Chitnis T, Ness J, et al. Acute disseminated encephalomyelitis. Neurology 2007;68:S23–36. [DOI] [PubMed] [Google Scholar]
- 4.Tsiodras S, Kelesidis T, Kelesidis I, et al. Mycoplasma pneumoniae-associated myelitis: a comprehensive review. Eur J Neurol 2006;13:112–24. [DOI] [PubMed] [Google Scholar]
- 5.Pellegrini M, O'Brien TJ, Hoy J, et al. Mycoplasma pneumoniae infection associated with an acute brainstem syndrome. Acta Neurol Scand 1996;93:203–6. [DOI] [PubMed] [Google Scholar]