Abstract
Deep Candida infections commonly occur in immunosuppressed patients. A rare case of a multiple deep organ infection with Candida albicansand spinal tuberculosis was reported in a healthy young man. The 19-year-old man complained of month-long fever and lower back pain. He also had a history of scalded mouth syndrome. Coinfection with Mycobacterium tuberculosis and Candida albicans was diagnosed using the culture of aspirates from different regions. Symptoms improved considerably after antifungal and antituberculous therapy. This case illustrates that infection with tuberculosis might impair the host's immune system and increase the risk of invasive candidiasis in an immunocompetent patient.
Keywords: Invasive candidiasis, Spine tuberculosis, Coinfection, Immunocompetent patient
Abstract
As infecções profundas por Candida ocorrem geralmente em pacientes imunossuprimidos. Relatamos caso raro de infecções profundas em múltiplos órgãos por Candida albicans e neuro tuberculose em homem jovem saudável. Um jovem de 19 anos de idade queixou-se de febre e lombalgia há um mês. Relatava ainda histórico de síndrome da boca escaldada. Foi diagnosticada co-infecção por Mycobacterium tuberculosis e Candida albicans em cultura do aspirado de diferentes regiões do organismo. Os sintomas melhoraram significativamente após a terapia antifúngica e antituberculosa. Este caso é apresentado para mostrar que a tuberculose pode prejudicar o sistema imune do hospedeiro e aumentar o risco de candidíase invasiva em paciente imunocompetente.
INTRODUCTION
Invasive candidiasis is a clinical condition that generally occurs in immunosuppressive patients and those with general defects in the immune system. Candida albicans is the most common fungal pathogen capable of causing infections, ranging from slight mucocutaneous disorders to invasive diseases which affect multiple organs3. Deep Candidainfections rarely occur in healthy hosts, but the incidence is greatly increased in immunosuppressive patients. Tuberculosis remains a major global health problem and has become significantly more prevalent in the past decade. Moreover, spinal tuberculosis may not display typical symptoms and, sometimes, show predominant extrapulmonary manifestations that result in delayed or missed diagnosis. Furthermore, multiple deep organ infections caused by Candida albicans and spinal tuberculosis occurring simultaneously in the same patient are very rare. In view of this, the following report presents the rare case of multiple deep abscesses caused by Candida albicans with simultaneously occurring spinal tuberculosis in an immunocompetent patient.
CASE REPORT
A 19-year-old man complained of recurrent fever and lower back pain for a month. He had a history of scalded mouth syndrome with no regular antibiotic or antifungal drug treatment six months prior to hospitalization. He had neither history of taking immunosuppressors, nor of any disease indicative of immunodeficiency. He had, however, received the Bacillus Calmette-Guérin (BCG) vaccine during childhood. On admission, his vital signs included an oral temperature of 39 ºC, heart rate of 92 beats per minute, respiratory rate of 20 breaths per minute and blood pressure of 130/80 mmHg. Physical examination revealed a 9×8cm mass in the right of the patient's neck, but no lesions were found on the oral mucosa. The remainder of the systemic examination was unremarkable.
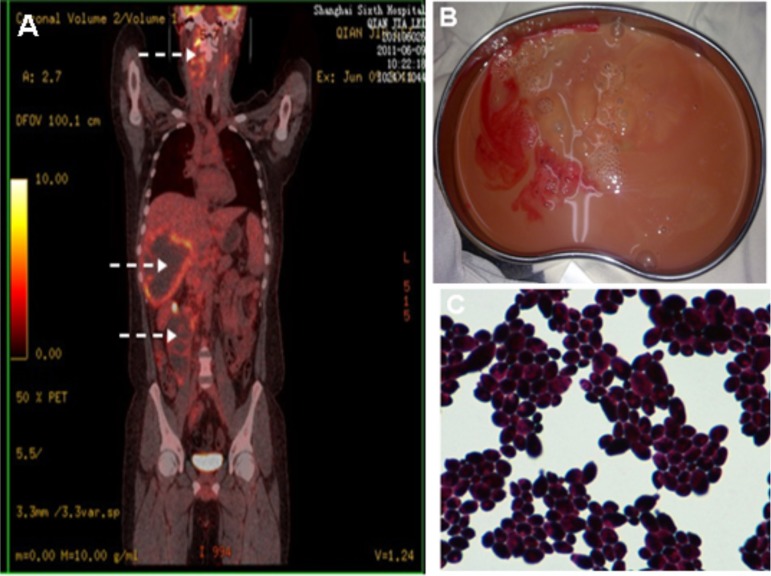
Laboratory results included a leukocyte count of 14800×103/mm3, serum glucose level of 143 mg/dL, blood urea nitrogen of 40 mg/dL and creatinine level of 1.7 mg/dL. Inflammatory markers were elevated with an erythrocyte sedimentation rate (ESR) of 120 mm/h and C-reactive protein (CRP) level of 11.1 mg/L. Both a tuberculin skin test and human immunodeficiency virus (HIV) antibody exam were negative. Comprehensive immunological studies, including serum immunoglobulins and complement levels, tests for cell-mediated immunity (NK, CD3, CD4, CD8, CD4/CD8 and CD19) and autoantibody tests, were normal. 1, 3-β-D-glucan assay levels and the galactomannan test were normal. Blood cultures were also negative. Whole-body positron emission tomography/computed tomography (PET/CT) revealed multiple abscesses in the right of the patient's neck, liver and right psoas major area respectively (Fig.1A); and there was a raised uptake of [18F] FDG in vertebral bodies of T11, T12 and L1. Consequently, percutaneous abscess drainage was conducted on the upper body using B-mode ultrasonography and drained brown fluids (30 mL, 280 mL and 130 mL, respectively, Fig.1B) were sent to the microbiology lab. Also, drainage tubes were inserted into abscesses in the liver and psoas major, but were removed after no drainage took place. Results of the Chromagar Candida Medium (Chromagar, France) cultures were positive for Candida albicans (Fig. 1C), but no acid-fast bacilli were detected. The germ tube test was positive and the documented diagnosis using API 20C Aux systems (BioMeriux, France) was Candida albicans, which was sensitive to amphotericin B, fluconazole, itraconazole, voriconazole, caspofungin and 5-fluorocytosine. Based on antifungal guidelines and susceptibility tests, he was treated with intravenous 35 mg amphotericin B daily (0.5 mg/kg per day). The patient responded to antifungal therapy and his fever abated after ten days of treatment. Abscess detection using B-mode ultrasonography revealed that the extent of infection in the upper body had greatly decreased at the end of three-week antifungal therapy.
Fig. 1. A. Whole-Body positron emission tomography/computed tomography (PET/CT) showing increased uptake of [18F]FDG appear in right neck, liver, right psoas major area respectively (arrows). B. The brown fluids were drained from the liver under B-mode ultrasonography inducted. C. Microphotography of Candida albicans Gram staining 1000×.
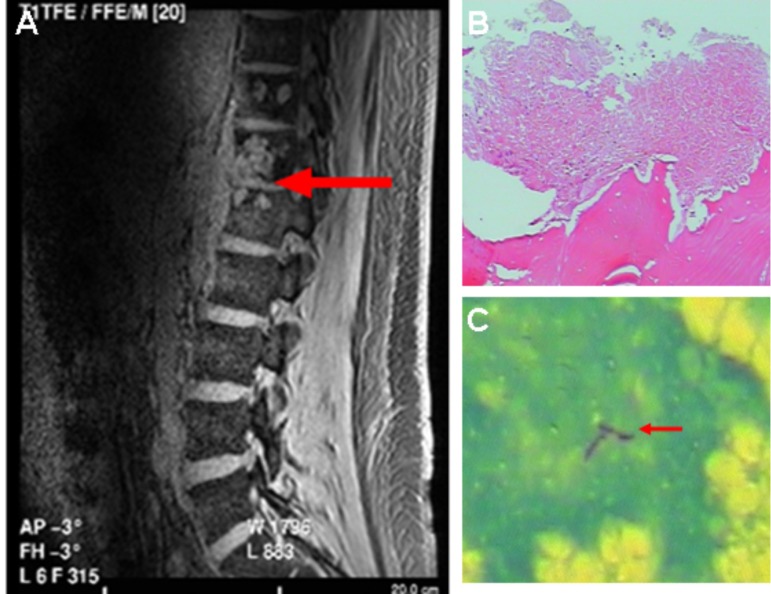
However, there was no improvement in the patient's lower back pain. Spinal magnetic resonance imaging (MRI) showed altered signal intensity in T11, T12, L1 and unique osteolytic lesions in upper vertebral bodies (Fig. 2A). Subsequently, computed tomography (CT) guided percutaneous vertebral biopsy specimens from the T12 vertebrae revealed caseous material and the acid fast bacilli were identified (Fig.2B, C). Also, the aspirate culture showed growth of the M. tuberculosis. Chest CT, urine and sputum examinations were normal. Taking histological and microbiological findings into consideration, the patient was treated with antitubercular therapy (rifampicin, isoniazid, pyrazinamide, ethambutol) for 12 months. In addition, he was treated with a total dose of 1500 mg of amphotericin B, while oral fluconazole and 5-flucytosine were subsequently prescribed for six months. By his 2-year follow up, there were complete resolutions of the lesions in the upper vertebral bodies and no evidence of new abscesses.
Fig. 2. A. MRI showing altered signal intensity in T11, T12, L1 and unique osteolytic lesions in the above vertebral bodies (arrow). B, C. Histopathologic examination of aspirates showing caseous material and acid fast bacilli (arrow), respectively.
DISCUSSION
Candida is an opportunistic fungal pathogen which generally forms part of the normal flora of the oropharynx, gastrointestinal tract, and urinary tract in the healthy human . Candida albicans is the most common pathogenic cause of fungal infections in humans, which can involve multiple organs, including the brain, mediastinum, kidney, heart, lung, pancreas, liver and peritoneum. Invasive candidiasis (IC) involves the infection and spread of Candida via the bloodstream and normally affects the immunocompromised or immunodeficient, such as those with diabetes, neutropenia or burns; people undergoing hemodialysis, abdominal surgery or total parenteral nutrition; and those undergoing long term therapy with broad-spectrum antibiotics or corticosteroids11. The incidence of IC in the US between 1996 and 2003 was 19-24 infections per 10,000 annual hospital discharges12.
As one knows, microscopic examination and the cultivation of clinical samples for the diagnosis of fungal infection are gold-standard methods. Diagnosis of invasive candidiasis remains difficult and is generally confirmed by the direct microscopic examination of the fluid drained during percutaneous or surgical abscess drainage. Candida infection in patients is clinically very difficult to recognize and its diagnosis is frequently missed because of non-specific clinical features, poor diagnostic yield of traditional microbiological techniques and the non-specificity of radiological imaging9. The results of blood cultures are frequently negative, as was the case for this patient. In addition, 1, 3-β-D-glucan assay levels and galactomannan tests were normal in this case. Recently, some studies testified the importance of [18F] FDG-PET/CT in detecting non-central nervous system invasive fungal infection at an early stage and assessing the efficiency of antifungal therapy5. With the help of whole-body PET/CT scans, the patient's multiple deep abscesses were found in time. Although the whole-body PET/CT provides a new, more sensitive way of observing deep organ infections, its high costs mean that it cannot be widely used in clinical examinations. According to the clinical practice guidelines for the management of candidiasis by the Infectious Diseases Society of America and antifungal susceptibility testing, amphotericin B is the current antifungal treatment of choice10. The patient responded to antifungal therapy and the number of abscesses was greatly decreased. In spite of the high death rates of invasive candidiasis, the patient survived due to the combination of early diagnosis, percutaneous drainage and antifungal therapy.
Tuberculosis (TB), a disease more common in immunocompromised persons, is a major global problem still prevalent in developing countries, despite the availability of highly effective treatment for decades. China has the second highest level of tuberculosis in the world, registering 12% of global cases (0.9 million - 1.1 million) in 201214. Tuberculosis' insidious nature often leads to delayed or missed diagnosis, sometimes with devastating consequences for the patient. In this patient, Candida spondylitis was initially thought of as the cause of his back pain, yet it showed no improvement following antifungal treatment. However, the patient's history of BCG vaccination, negative skin tests and normal chest scans were not disregarded when considering the diagnosis of tuberculosis. Percutaneous vertebral biopsy was very useful in confirming diagnosis and could help avoid open surgical biopsy in future patients. The mainstay in the treatment of spinal tuberculosis is the conservative management of antituberculous drugs. Surgery is needed only if there is neurological deficit or spinal instability. In the management of osteoarticular tuberculosis, chemotherapy including isoniazid, rifampin, ethambutol, and pyrazinamide is recommended for approximately 12 - 18 months8. The patient was administered antituberculous treatment with the above four drugs for a 12-month period. At the final 2-year follow-up, the patient was free of symptoms, though there was little change in the radiological picture except for increased sclerosis at the margin of the lesion.
Deep Candida infections generally occur in immunosuppressive patients, especially those who have been treated with immunosuppressors. Recent studies showed that M. tuberculosis promoted down-modulatory immune mediators to counteract Th1-type cells and patients' innate immunity, and might have suppressive effects on the host's immune system1 , 2. Also, levels of FoxP3 gene expression and IL-10 secretion were raised in both pulmonary TB and extra-pulmonary TB7. The secretion of IL-10 by regulatory T cells can account for the inhibition of T cell responses and increase the risk of tuberculosis reactivation6. A case of coinfection with M. tuberculosis and Cryptococcus gattii in a healthy young woman indicated that infection with TB predisposed to infection with Cryptococcus by down-regulate immune system and altered host defenses13. In the case featured in this report, the patient was immunocompetent and had no history of using immunosuppressive drugs or having any recent major surgery. It is likely that Candida albicans invaded his bloodstream through impaired oral mucosa membranes and stuck to the endothelial cells of his blood vessels, in turn transmigrating into the tissue4. This indicated that TB infection may impair the host's immune system and that the spread of Candida albicansmaybe ultimately lead to the occurrence of multiple deep organ infections in the healthy young man.
In conclusion, multiple deep organ infections with Candida albicans and spinal tuberculosis are rare in healthy young men. Moreover, as it is always difficult to identify M. tuberculosis, early diagnosis should be considered in patients with clinical and radiological findings suggesting tuberculosis to avoid missing diagnosis, particularly in developing countries where tuberculosis is endemic. Furthermore, the present case report suggests that tuberculosis infection might increase the risk of invasive candidiasis in patients without significant immunodeficiency. This hypothesis needs to be confirmed by prospective cohorts with sufficiently large sample sizes.
REFERENCES
- 1.Almeida AS, Lago PM, Boechat N, Huard RC, Lazzarini LC, Santos AR, et al. Tuberculosis is associated with a down-modulatory lung immune response that impairs Th1-type immunity. J Immunol. 2009;183:718–731. doi: 10.4049/jimmunol.0801212. [DOI] [PubMed] [Google Scholar]
- 2.Bonecini-Almeida MG, Ho JL, Boéchat N, Huard RC, Chitale S, Doo H, et al. Down-modulation of lung immune responses by interleukin-10 and transforming growth factor beta (TGF-beta) and analysis of TGF-beta receptors I and II in active tuberculosis. Infect Immun. 2004;72:2628–2634. doi: 10.1128/IAI.72.5.2628-2634.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fridkin SK. The changing face of fungal infections in health care settings. Clin Infect Dis. 2005;41:1455–1460. doi: 10.1086/497138. [DOI] [PubMed] [Google Scholar]
- 4.Grubb SE, Murdoch C, Sudbery PE, Saville SP, Lopez-Ribot JL, Thornhill MH. Candida albicans -endothelial cell interactions: a key step in the pathogenesis of systemic candidiasis. Infect Immun. 2008;76:4370–4377. doi: 10.1128/IAI.00332-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hot A, Maunoury C, Poiree S, Lanternier F, Viard JP, Loulergue P, et al. Diagnostic contribution of positron emission tomography with [18F] fluorodeoxyglucose for invasive fungal infections. Clin Microbiol Infect. 2011;17:409–417. doi: 10.1111/j.1469-0691.2010.03301.x. [DOI] [PubMed] [Google Scholar]
- 6.Kursar M, Koch M, Mittrücker HW, Nouailles G, Bonhagen K, Kamradt T, et al. Cutting Edge: regulatory T cells prevent efficient clearance of Mycobacterium tuberculosis. . J Immunol. 2007;178:2661–2665. doi: 10.4049/jimmunol.178.5.2661. [DOI] [PubMed] [Google Scholar]
- 7.Masood KI, Rottenberg ME, Salahuddin N, Irfan M, Rao N, Carow B, et al. Expression of M.tuberculosis -induced suppressor of cytokine signaling (SOCS) 1, SOCS3, FoxP3 and secretion of IL-6 associates with differing clinical severity of tuberculosis. BMC Infect Dis. 2013;13:13–13. doi: 10.1186/1471-2334-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbosacral spine. Clin Orthop Relat Res. 2002;398:40–49. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Oz Y, Kiraz N. Diagnostic methods for fungal infections in pediatric patients: microbiological, serological and molecular methods. Expert Rev Anti Infect Ther. 2011;9:289–298. doi: 10.1586/eri.10.168. [DOI] [PubMed] [Google Scholar]
- 10.Pappas PG, Kauffman CA, Andes D, Benjamin DK, Jr, Calandra TF, Edwards JE, Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–535. doi: 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pfaller MA. Nosocomial candidiasis: emerging species, reservoirs, and modes of transmission. Clin Infect Dis. 1996;22(Suppl 2):S89–S94. doi: 10.1093/clinids/22.supplement_2.s89. [DOI] [PubMed] [Google Scholar]
- 12.Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent problem. Clin Microbiol Rev. 2007;20:133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Tongeren L, Shaipanich T, Fleetham JA. Coinfection with Cryptococcus gattii and Mycobacterium tuberculosis in an otherwise healthy 18-year-old woman. Can Respir J. 2011;18:e62–e63. doi: 10.1155/2011/812345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization . Global tuberculosis report. Geneva: WHO; 2013. [Google Scholar]