Description
Acute pulmonary embolism (PE) is common, however, being a fatal disease prompting early diagnosis and treatment to prevent mortality. However, the varying clinical picture makes diagnosis difficult. The author reports a 56-year-old paraplegic man who presented with acute dyspnoea and discomfort in the chest. The patient had recently discontinued his anticoagulant use for prevention of venous thromboembolic disease. The ECG showed the finding of sinus tachycardia along with S wave in lead I, Q wave and inverted T wave in lead III which has been associated with acute massive PE causing cor pulmonale (figure 1).1 Though not sensitive, this raised the suspicion PE and considering the clinical picture a CT pulmonary angiography was ordered that showed extensive thromboembolic disease in the bilateral main pulmonary arteries extending to the lobar and segmental pulmonary arteries. An echocardiogram demonstrated significant right ventricular and atrial enlargement with right ventricular dysfunction and strain pattern. Considering the clinical picture the patient was a candidate for fibrinolytic therapy and had a favourable outcome.
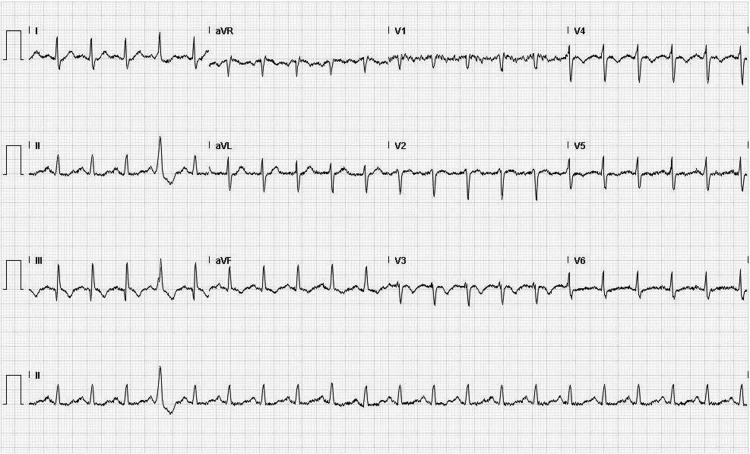
Figure 1.
ECG showing an S wave in lead I, Q wave and an inverted T wave in lead III.
Petruzzeli studied ECG abnormalities in patients with suspected PE and found PR displacement; late R in avR, slurred S in V1 or V2, the S1Q3T3 pattern and T wave inversion in V1 or V2 were significantly more common in patients with confirmed PE.2 Further, Nazeyrollas et al3 found only an S wave in I and Q wave in III significantly more common among those with confirmed PE. Recognising these ECG findings could prompt clinicians to consider PE and lead to earlier diagnosis of the same.
Learning points.
Acute pulmonary embolism (PE) is a fatal disease, and early diagnosis and treatment are indicated to prevent mortality.
ECG abnormalities in such as PR displacement; late R in avR, slurred S in V1 or V2, the S1Q3T3 pattern and T wave inversion in V1 or V2 are significantly more common in patients with confirmed PE.
Recognising the ECG findings could prompt clinicians to consider PE and lead to earlier diagnosis of the same.
Footnotes
Patient consent: Obtained.
References
- 1.McGinn S, White PD. Acute cor pulmonarly resulting from pulmonary embolism. JAMA 1935;104:1473–80. [Google Scholar]
- 2.Petruzzelli S, Palla A, Pieraccini F, et al. Routine electrocardiography in screening for pulmonary embolism. Respiration 1986;50:233–43. [DOI] [PubMed] [Google Scholar]
- 3.Nazeyrollas P, Metz D, Jolly D, et al. Use of transthoracic Doppler echocardiography combined with clinical and electrocardiographic data to predict acute pulmonary embolism. Eur Heart J 1996;17:779–86. [DOI] [PubMed] [Google Scholar]