Abstract
A 45-year-old Caucasian female with diagnosis of central serous chorioretinopathy (CSCR) did not improve on conventional observational approach. She was not willing to proceed with photocoagulation or photodynamic therapy. An unconventional approach of topical anti-inflammatory (ketorolac, dexamethasone and hydrocortisone) preparation was prescribed. The course of her CSCR responded well on this unconventional treatment, but relapsed on cessation or tapering of treatment. After 18 weeks of treatment with a gradual taper, her condition resolved. The present case highlights an alternative but unconventional treatment of CSCR with prolonged use of anti-inflammatories.
Background
This case highlights a different therapeutic approach to a common ophthalmic presentation, successfully treated with unconventional therapy.
Case presentation
A 45-year-old Caucasian female was referred by her primary care practitioner to the Dubbo Eye Centre with decreased right visual acuity (VR) and relative central scotoma for a duration of 4 days prior to her presentation.
She denied any ocular history of significance. Her medical history was unremarkable. She is not on any medications and denied using any steroidbased therapy (oral, inhaled or topical). She denied having experienced any recent life stressors. She is a life-long non-smoker and systems review was non-contributory.
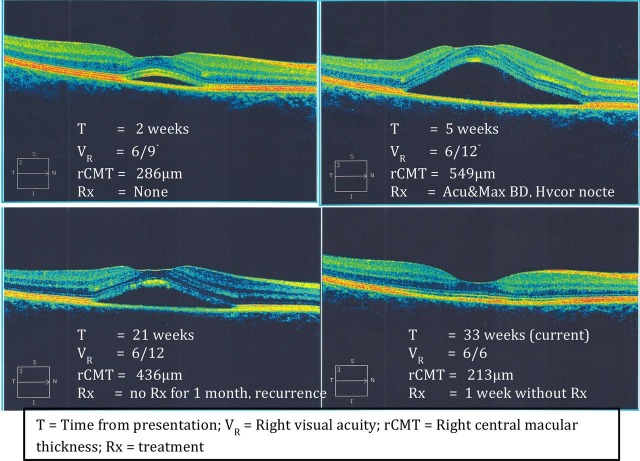
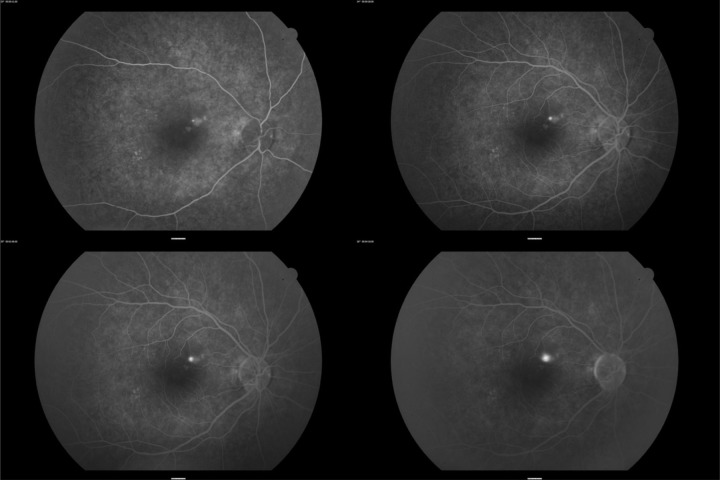
On examination, visual acuity on initial presentation was 6/9− in her right and 6/6 in her left eye. The intraocular pressures were 12 mm Hg in each eye measured at midday. Anterior segment examination was normal. Dilated fundal examination of her right eye showed a hypopigmented area superior to her fovea associated with serous detachment. The left fundus was normal. High-resolution optical coherence tomography (OCT) was performed to evaluate the area of serous detachment (figure 1). Intravenous fundus fluorescein angiography was performed to elucidate the site responsible for her serous detachment (figure 2).
Figure 1.
Recovery pattern of central serous chorioretinopathy on OCT.
Figure 2.
Intravenous fundal fluorescein angiography of the case reported.
She was treated conservatively but returned 2 weeks later with worsening right visual acuity (VR) to 6/12 and increased right central macular thickness (rCMT) from 231 to 286 μm. She has refused treatment with photocoagulation and photodynamic therapy (PDT) is not available due to her geographic location and unwillingness to travel.
Investigations
Treatment
Tapering dose of topical anti-inflammatory ophthalmic preparations over 6 weeks:
Dexamethasone 0.1%; four times a day,
ketorolac trometamol 5 mg/ml; four times a day and
hydrocortisone acetate 1%; nocte.
Outcome and follow-up
Four weeks after her initial presentation, VR improved to 6/5, rCMT was 231 μm, she was using the above eye drop regime twice a day and ointment at night. She was pleased with her results and continued tapering her treatment.
A week later (5 weeks after initial presentation) she noticed worsening of her right visual acuity with a grey shadow (relative central scotoma), VR was 6/12−, and her rCMT was 549 μm. She was on daily topical drops only at that stage. Her topical regime was increased to four times a day again.
She was reviewed again 2 weeks later (7 weeks after initial presentation); visual acuity was 6/6, rCMT decreased to 394 μm. She continued her current drop regime without taper. rCMT on OCT 4 weeks after recommencement of therapy (9 weeks after initial presentation) returned to 238 μm, VR stabilised at 6/6. Her topical treatment regime was slowly tapered over 2 months.
Two weeks after stopping treatment, she re-presented with recurrence relative central scotoma. Right visual acuity was 6/12 and rCMT was 436 μm. Topical anti-inflammatory therapy was recommenced. She was reviewed 2 weeks later and reported improvement of her scotoma, VR was 6/9, rCMT decreased to 405 μm. She continued her therapy for a further 5 weeks, VR improved to 6/6, rCMT returned to 234 μm. Therapy was again tapered on a fortnightly basis.
She is currently 1 week without treatment, VR was 6/6 and rCMT was 213 μm.
Discussion
Our case offers a possible alternative treatment to patients with recalcitrant central serous chorioretinopathy (CSCR) with limited treatment options.
The primary pathophysiology of CSCR is a dysfunction of the retinal pigment epithelium (RPE), which leads to increased permeability of the RPE causing neurosensory retinal detachment.1 There have been numerous postulations to the dysfunction of RPE cells and hyperpermeable state seen in CSCR:
elevated circulating cortisol level;2 increases capillary fragility and has a direct affect on RPE ion transfer, inducing a hyperosmolar state in the sub-RPE space resulting in osmotic diffusion of fluid into the sub-RPE space causing neurosensory detachment;3
damage to the microcirculation of the choriocapillaris and RPE;4
steroid use, suppresses healing process of the RPE.5
We believe damage to RPE might be mediated by an inflammatory process, hence we trialled the use of topical anti-inflammatories in this case. Steroid use (systemic and inhaled) has been implicated as a risk factor or causal factor for development of CSCR for the reason described above. However, topical treatment with steroids and anti-inflammatories might be enough to suppress the inflammatory process but not have such a profound effect to hinder the healing process of the RPE.
Learning points.
Conventional treatment might not be available or appropriate in certain cases.
Exploration of unconventional treatment approaches might work, and have worked in this case.
A trial of anti-inflammatories might be helpful in inflammatory-mediated processes.
Typical appearance of central serous chorioretinopathy demonstrated in OCT and angiogram pictures.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Von Graefe A. Uber centrale recidivierende Retinitis. Graefes Arch Clin Exp Ophthalmol 1866;12:211–15. [Google Scholar]
- 2.Gass JDM. Pathogenesis of disciform detachment of the neuro-epithelium:1. General concepts and classification. Am J Ophthalmol 1967;63:573–85. [PubMed] [Google Scholar]
- 3.Wang M, Munch IC, Hasler PW, et al. Central serous chorioretinopathy. Acta Ophthalmol 2008;86:126–45. [DOI] [PubMed] [Google Scholar]
- 4.Ciardella AP, Huang SJ, Danielle LLC, et al. Central serous chorioretinopathy. In: Frankhauser F, ed. Lasers in ophthalmology: basic, diagnostic and surgical aspects: a review. Netherlands: Kugler Publications, 2003:255–75. [Google Scholar]
- 5.Carvalho-Recchia CA, Yannuzzi LA, Negrao S, et al. Corticosteroids and central serous chorioretinopathy. Ophthalmol 2002;109:1834–7. [DOI] [PubMed] [Google Scholar]