Abstract
Autologous bone grafts are widely used in oral and maxillofacial surgery, orthopedics, and traumatology. Autologous bone grafts not only replace missing bone, they also support the complex process of bone regeneration. This favorable behavior of autografts is attributed to the three characteristics: osteoconductivity, osteogenicity, and osteoinductivity. However, there is another aspect: Bone grafts release a myriad of molecules, including growth factors, which can target mesenchymal cells involved in bone regeneration. The paracrine properties of bone grafts can be studied in vitro by the use of bone-conditioned medium (BCM). Here we present a protocol on how to prepare bone-conditioned medium from native pig cortical bone, and bone that underwent thermal processing or demineralization. Cells can be directly exposed to BCM or seeded onto biomaterials, such as collagen membranes, previously soaked with BCM. We give examples for in vitro bioassays with mesenchymal cells on the expression of TGF-β regulated genes. The presented protocols should encourage to further reveal the paracrine effects of bone grafts during bone regeneration and open a path for translational research in the broad field of reconstructive surgery.
Keywords: Molecular Biology, Issue 101, Bone Conditioned Medium, BCM, bone autograft, guided bone regeneration, GBR, dental implant, membrane, supernatant, growth factors, contour augmentation, autologous bone
Introduction
Autologous bone is widely used to bridge defects that occurred as a consequence of malformation, resective surgery, reconstructive trauma surgery, and prior to implant placement 1,2. Understanding the biological principles of how bone grafts support the process of graft consolidation is not only key to understand why autografts are considered to be the gold standard in reconstructive surgery, it is also bionic to the improved design of bone substitutes 3. Still, graft consolidation is faster with autologous bone compared to bone substitutes 4,5. Thus, it is imperative to reveal the molecular and cellular mechanisms that make autologous bone so effective to support bone regeneration.
There are three textbook characteristics of autografts that are considered to support the consolidation process 6,7. First, autologous bone is osteoconductive, providing guidance for the newly formed bone to grow into the defect. Secondly, autologous bone is osteogenic, meaning that it contains mesenchymal cells that can differentiate into osteoblasts 8. Third, autologous bone is osteoinductive as growth factors like bone morphogenetic proteins entombed in the matrix can initiate the process of endochondral or even intramembranous bone formation 9. There is another aspect: freshly prepared bone chips hold a paracrine function based on the in vitro observations with “bone-conditioned medium” 10-15. Also the impact of myelopoiesis should be mentioned 16. A similar term “demineralized bone matrix-conditioned medium” was already coined in 1996 and supports the overall concept of a paracrine function of bone, even when processed by demineralization 17. For our purposes, BCM can be prepared from fresh pig mandibles 10,11. Proteomic analyses of BCM revealed the complex composition, including growth factors and constituents of the extracellular matrix 10, also extending existing knowledge on the proteasome of whole bone 18,19. Thus, BCM should reflect the released activity of various modifications of bone grafts in vitro.
What happens when mesenchymal cells, for example those isolated from bone chips or from oral soft tissue, are exposed to BCM? In vitro, BCM reduces osteogenic and adipogenic differentiation, and provokes a strong increase of IL11 expression 11. Genome wide microarray revealed more genes to be differentially expressed in mesenchymal cells in response to BCM. Among these genes are adrenomedullin (ADM), IL11, IL33, NADPH oxidase 4 (NOX4), proteoglycan 4 (PRG4, or lubricin) and pentraxin 3 (PTX3) 15. BCM obtained from autoclaved bone chips failed to change the expression of the respective genes 14. BCM from bone chips that underwent pasteurization and freezing was able to change gene expression 14. Also conditioned medium of demineralized bone matrix (DBM-CM) changes the expression of TGF-β-regulated genes 20. Interestingly, collagen barrier membranes used to shield the bone chips from the surrounding soft tissue 21,22, adsorbed those parts of BCM that are responsible for the changes in gene expression 23. BCM research can be extended to other cell types involved in bone regeneration such as bone-resorbing osteoclasts and endothelial cells, to name a few. Overall, the accumulating in vitro data provide the scientific basis for the design of a preclinical study.
The present protocol is two-fold: First, it shows how to prepare BCM. Secondly, it shows how to test its biological activity based on mesenchymal cells in vitro.
Protocol
1. BCM Preparation
Obtain pig mandibles from the local butcher as fresh as possible. Place the mandibles onto a firm surface and release a full thickness flap paying special attention not to leave any soft tissue or periosteum attached to the bone. Work in a clean environment without the need to work under the flow hood.
- Once a full thickness flap is released, use a bone scraper to harvest the bone chips from the buccal side. Please note that the bone scraper has to be sharp. Handle firmly the bone scraper and with long movements collect the bone. Discard bone chips smaller that 1mm.
- To maintain native bone chips, place directly the bone chips in plastic dishes of 10cm diameter with Dulbecco's Modified Eagle's medium (DMEM) supplemented with 1% antibiotics and antimycotics not letting them to dry out.
- To evaluate the impact of thermal processing, subject bone chips to pasteurization for 30 min at 80 °C or autoclave for 20 min at 121 °C.
- To evaluate the impact of demineralization, shake bone chips in 1 M HCL for 4-6 hr at 4 °C and wash repeatedly with culture medium until the pH is neutral.
Place a total of 5 g of bone chips per 10 ml fresh DMEM supplemented with 1% antibiotics and antimycotics into a new plastic dish.
Place the plastic dishes in a humidified atmosphere at 37 °C for 24 hr. Then, harvest BCM. Centrifuge the BCM at 200 x g for 10 min to remove debris, filter it sterile (0.2 nm), and keep aliquots frozen at -80 °C.
Thaw the BCM stock immediately before use and avoid repeated cycles of freezing and thawing.
For indicated experiments, soak collagen membranes with BCM or serum-free medium for 1 hr at RT. Wash vigorously the membranes with PBS and place them into 96 well plates. Wet membranes are seeded with cells.
BCM preparation process is summarized in Figure 1.
2. Bioassays Based on Mesenchymal Cells
Seed human mesenchymal cells (for example bone cells, gingival and periodontal ligament fibroblasts) into a 12-well plate with a concentration of 30,000 cells/cm2. To seed the cells use growth medium consisting of DMEM, 10% fetal calf serum and antibiotics. Let the cells attach to the plate O/N.
Discard the culture medium and wash the cells with pre-warmed PBS at 37 °C. Stimulate the cells by adding pre-warmed serum-free culture medium with and without 20% BCM. Place the cells in a humidified atmosphere at 37 °C for 24 hr.
Discard the culture medium, rinse the cells with pre-warmed PBS and extract the RNA according to your preferred protocol.
Adjust the concentration of RNA in order to have the same amount of RNA in each sample. Prepare cDNAs and perform a qRT-PCR to analyse the selected genes using the primers shown in Table 1. NOTE: These are the dilutions of every component: 2x SYBR Green, 20x primer forward, 20x primer reverse, 5x sterile DD water, 5x cDNA. The qRT-PCR is performed in 40 cycles of 95 °C 15 sec and 60 °C 1 min.
Calculate the relative expression levels by normalizing to the housekeeping gene GAPDH using the Δ(ΔCt) method where ΔCT is CT target - CT GAPDH and Δ(ΔCT) is ΔCT stimulated - ΔCT control.
After this quality control, add BCM to culture medium to stimulate all types of cells including mesenchymal cells, hematopoietic cells or endothelial cells.
Representative Results
Bone Conditioned Medium is prepared from fresh porcine bone chips. General overview of the process to prepare BCM and to use biomaterials in combination with BCM is shown in Figure 1 and Figure 2 respectively. During the BCM preparation, it is important to obtain large bone chips with long movements as short movements or very small bone chips can affect the quality of the final BCM. Quality of BCM can be controlled by analyzing the gene expression of BCM target genes: ADM, PTX3, IL11, IL33, NOX4 and PRG4 (Figure 3). ADM and PTX3 are down-regulated down to 0.4-fold and IL11, IL33, NOX4 and PRG4 can be up-regulated to 200-fold. If oral fibroblasts do not express BCM target genes at the level shown, check the health of the cells or prepare new BCM from new mandibles. Figure 4 displays typical results from the expression of BCM target genes in oral fibroblasts seeded onto a collagen barrier membrane. Oral fibroblasts stimulated with 20% of conditioned medium from pasteurized bone chips and conditioned medium from demineralized bone chips, showed similar gene expression to cells stimulated with BCM (Table 2 and Table 3). However, gene expression of oral fibroblasts exposed to conditioned medium from sterilized (121 °C) bone chips, was comparable to un-stimulated controls.
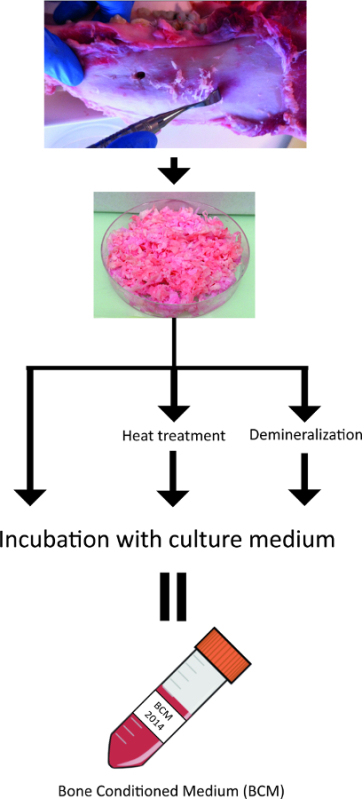 Figure 1. Summary of the process used to prepare bone-conditioned medium from fresh pig mandibles.
Please click here to view a larger version of this figure.
Figure 1. Summary of the process used to prepare bone-conditioned medium from fresh pig mandibles.
Please click here to view a larger version of this figure.
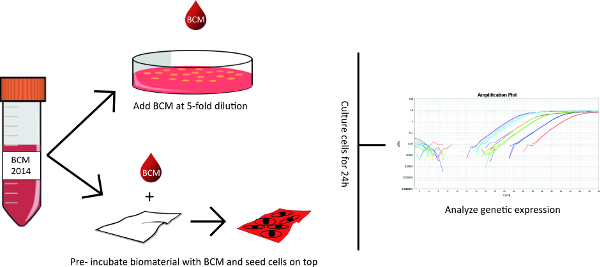 Figure 2. Summary of the bioassays based on mesenchymal cells with BCM.
Please click here to view a larger version of this figure.
Figure 2. Summary of the bioassays based on mesenchymal cells with BCM.
Please click here to view a larger version of this figure.
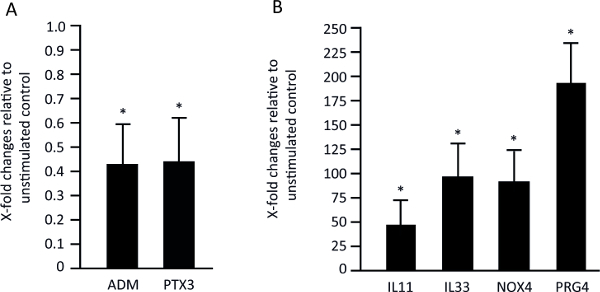 Figure 3. Gene expression of bone-conditioned medium target genes in oral fibroblasts. Typical results of six genes used to control the quality of BCM. Genes ADM and PTX3 are downregulated (A) and IL11, IL33, NOX4, PRG4 are upregulated (B). Please click here to view a larger version of this figure.
Figure 3. Gene expression of bone-conditioned medium target genes in oral fibroblasts. Typical results of six genes used to control the quality of BCM. Genes ADM and PTX3 are downregulated (A) and IL11, IL33, NOX4, PRG4 are upregulated (B). Please click here to view a larger version of this figure.
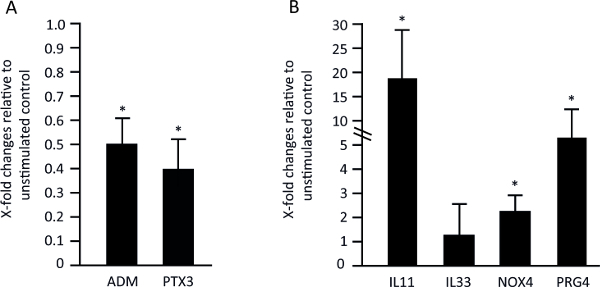 Figure 4. Gene expression of bone-conditioned medium target genes in oral fibroblasts seeded onto a collagen barrier membrane. Typical results of six genes used to control the quality of BCM. Genes ADM and PTX3 are downregulated (A) and IL11, NOX4, PRG4 are upregulated (B). Depending on the biomaterial used, the absorption of growth factors can differ. Collagen membranes failed to absorb factors that control IL33 expression, therefore IL33 expression is not regulated in this setting. Please click here to view a larger version of this figure.
Figure 4. Gene expression of bone-conditioned medium target genes in oral fibroblasts seeded onto a collagen barrier membrane. Typical results of six genes used to control the quality of BCM. Genes ADM and PTX3 are downregulated (A) and IL11, NOX4, PRG4 are upregulated (B). Depending on the biomaterial used, the absorption of growth factors can differ. Collagen membranes failed to absorb factors that control IL33 expression, therefore IL33 expression is not regulated in this setting. Please click here to view a larger version of this figure.
| Abbreviation | Primer forward | Primer reverse |
| GAPDH | AGCCACATCGCTCAGACAC | GCCCAATACGACCAAATCC |
| ADM | GGACATGAAGGGTGCCTCTC | TGTTCATGCTCTGGCGGTAG |
| IL11 | TGCACCTGACACTTGACTGG | AGTCTTCAGCAGCAGCAGTC |
| IL33 | TCAGGTGACGGTGTTGATGG | GGAGCTCCACAGAGTGTTCC |
| NOX4 | TCTTGGCTTACCTCCGAGGA | CTCCTGGTTCTCCTGCTTGG |
| PRG4 | CGACGCCCAATGTAAGAAGT | GGTGATGTGGGATTATGCACT |
| PTX3 | TGTATGTGAATTTGGACAACGAA | CATTCCGAGTGCTCCTGAC |
Table 1: Primer sequence of the 6 genes used.
| Genes | 80 °C Mean ± SD | 121 °C Mean ± SD |
| ADM | 0.2 ± 0.1 | 1.1 ± 0.2 |
| PTX3 | 0.1 ± 0.1 | 0.9 ± 0.2 |
| IL11 | 20 ± 10 | 1.5 ± 1 |
| IL33 | 15 ± 5 | 1.2 ± 4 |
| NOX4 | 35 ± 15 | 2 ± 1 |
| PRG4 | 40 ± 10 | 1.8 ± 1 |
Table 2: Typical gene expression of ADM, PTX3, IL11, IL33, NOX4 and PRG4 in oral fibroblasts stimulated with 20% of conditioned medium from heat-treated bone chips.
| Genes | Mean ± SD |
| ADM | 0.1 ± 0.1 |
| PTX3 | 0.1 ± 0.1 |
| IL11 | 15 ± 5 |
| IL33 | 20 ± 10 |
| NOX4 | 60 ± 15 |
| PRG4 | 50± 20 |
Table 3:Typical gene expression of ADM, PTX3, IL11, IL33, NOX4 and PRG4 in oral fibroblasts stimulated with 20% of conditioned medium from demineralized bone chips.
Discussion
Bone-conditioned medium reflects the released activity of bone grafts during the early stages of bone regeneration. The protocol described here can be adapted to study the response of different types of cells involved in bone regeneration. Furthermore, the protocol can be used to prepare conditioned medium from processed bone or bone fillers. The methods are easy to perform and rely on a simple concept: the factors released from various native and processed bone. Understanding how BCM affects mesenchymal cells can help to learn more about graft consolidation and properties of bone autografts. Based on this concept we have accumulated knowledge on the impact of BCM obtained from native 11,15 and processed bone 14,20 on gene expression of mesenchymal cells, but also on proliferation, migration, and differentiation into the three main lineages; osteoblasts, adipocytes and chondrocytes 11. BCM was also examined for its capacity to target hematopoietic cells, for example with respect to the modulation of osteoclastogenesis 13. Many potential target cells are waiting to respond to BCM in vitro, the protocols presented here, can serve as a primer for this research.
The presented protocols should also animate to further reveal the molecular mechanisms of how BCM activates particularly TGF-β-regulated genes in mesenchymal cells. For example, the TGF-β receptor I antagonist SB431542 blocked the effect of BCM on the expression of the gene panel ADM, IL-11, NOX4, PRG4, and PTX3 11,15. Interestingly, alkaline phosphatase and IL33 were not reversed by SB431542 11,15 suggesting that other as yet unknown pathways are regulated by BCM. Another open question is what are the molecules in BCM being responsible for the cellular response? BCM contains TGF-β but is does not explain the complex cellular reactions 10,11. Besides the in vitro cellular aspects, the overall question remains: to which extend does the released activity of bone grafts as reflected by BCM, have an impact on the in vivo process of bone regeneration? The protocols and data from bioassays should introduce research in this direction.
This protocol has limitations. BCM cannot be fully standardized because of variations between donors and harvesting techniques. Moreover, how enzymes present in vivo can affect the composition or activity of BCM remains unknown. Future studies should, for example, focus on how harvesting techniques affect the “biological activity” of BCM. The role of osteocytes on the composition of BCM should also be studied in detail. BCM contains sclerostin, a molecule released almost exclusively by osteocytes 12. Limitations, however, provide the inspiration for the next steps in research. Even though the clinical relevance of research with BCM remains hypothetical, our protocols support the long-standing concept that bone grafts, either native or after processing, release a “biological activity”. Understanding how BCM affect cells in vitro can presumably help to understand how bone autografts will work in vivo.
Disclosures
The authors have nothing to disclose. Jordi Caballé-Serrano received a scholarship from the Foundation of Dental Research and Education, Basel, Switzerland.
Acknowledgments
Authors would like to thank Catherine Solioz for her skillful assistance.
References
- Buser D. Long-term Stability of Early Implant Placement with Contour Augmentation. Journal of dental research. 2013. [DOI] [PMC free article] [PubMed]
- Chiapasco M, Casentini P, Bone Zaniboni M. augmentation procedures in implant dentistry. The International journal of oral & maxillofacial implants. 24 Suppl. 2009. pp. 237–259. [PubMed]
- Giannoudis PV, Dinopoulos H, Bone Tsiridis E. substitutes: an update. Injury. 36, Suppl 3. S20-S27. 2005. [DOI] [PubMed]
- Jensen SS, Broggini N, Hjorting-Hansen E, Schenk R, Bone Buser D. healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate. A histologic and histomorphometric study in the mandibles of minipigs. Clinical oral implants research. 2006;17:237–243. doi: 10.1111/j.1600-0501.2005.01257.x. [DOI] [PubMed] [Google Scholar]
- Jensen SS. Evaluation of a novel biphasic calcium phosphate in standardized bone defects: a histologic and histomorphometric study in the mandibles of minipigs. Clinical oral implants research. 2007;18:752–760. doi: 10.1111/j.1600-0501.2007.01417.x. [DOI] [PubMed] [Google Scholar]
- Grabowski G, Bone Cornett CA. graft and bone graft substitutes in spine surgery: current concepts and controversies. The Journal of the American Academy of Orthopaedic Surgeons. 2013;21:51–60. doi: 10.5435/JAAOS-21-01-51. [DOI] [PubMed] [Google Scholar]
- Khan SN. The biology of bone grafting. The Journal of the American Academy of Orthopaedic Surgeons. 2005;13:77–86. [PubMed] [Google Scholar]
- Bohr H, Ravn HO, Werner H. The osteogenic effect of bone transplants in rabbits. The Journal of bone and joint surgery. British. 1968;50:866–873. [PubMed] [Google Scholar]
- Bone Urist MR. formation by autoinduction. Science. 1965;150:893–899. doi: 10.1126/science.150.3698.893. [DOI] [PubMed] [Google Scholar]
- Caballé-Serrano JD, Buser D, Gruber R. Proteomic analysis of porcine bone conditioned medium. The International journal of oral & maxillofacial implants. 2014. [DOI] [PubMed]
- Peng J. Bone-Conditioned Medium Inhibits Osteogenic and Adipogenic Differentiation of Mesenchymal Cells In Vitro. Clinical implant dentistry and related research. 2014. [DOI] [PubMed]
- Brolese E, Buser D, Kuchler U, Schaller B, Gruber R. Human bone chips release of sclerostin and FGF-23 into the culture medium: an in vitro pilot study. Clinical oral implants research. 2014. [DOI] [PubMed]
- Caballé-Serrano J, Bosshardt DD, Gargallo-Albiol J, Buser D, Bone Gruber R. conditioned medium enhances osteoclastogenesis in murine bone marrow cultures. Clin Oral Impl Res; in. Int J Oral Maxillofac Surg. 2015. [DOI] [PubMed]
- Zimmermann M. Bone-conditioned medium changes gene expression in bone-derived fibroblasts) IJOMI accepted. 2014. [DOI] [PubMed]
- Fulzele K. Myelopoiesis is regulated by osteocytes through Gsalpha-dependent signaling. Blood. 2013;121:930–939. doi: 10.1182/blood-2012-06-437160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra J, Andrades JA, Ertl DC, Sorgente N, Nimni ME. Demineralized bone matrix mediates differentiation of bone marrow stromal cells in vitro: effect of age of cell donor. Journal of. 1996;11:1703–1714. doi: 10.1002/jbmr.5650111114. [DOI] [PubMed] [Google Scholar]
- Kupcova Skalnikova , H Proteomic techniques for characterisation of mesenchymal stem cell secretome. Biochimie. 2013. [DOI] [PubMed]
- Romanello M. Bone: 2013. Osteoblastic cell secretome: A novel role for progranulin during risedronate treatment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuldt Filho , G Conditioned medium of demineralized bone matrix activates TGF-β signaling pathways in mesenchymal cells in vitro. J Cranio Maxill Surg. 2015.
- Buser D, Chen ST, Weber HP, Belser UC. Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures) The International journal of periodontics & restorative dentistry. 2008;28:441–451. [PubMed] [Google Scholar]
- Stoecklin-Wasmer C. Journal of dental research. Vol. 92. progress: 2013. Absorbable collagen membranes for periodontal regeneration: a systematic review; pp. 773–781. [DOI] [PubMed] [Google Scholar]


