Summary
The usefulness of electricity in daily life offers several advantages which cannot be underestimated. Electricity is needed by industries for manufacturing and also in homes for lighting, cooking, washing, etc. However, electricity can cause severe life-threatening complications. This study investigates the trend and mortality risk factors of electrical burn injuries at the Burns Intensive Care Unit (BICU) of the Komfo Anokye Teaching Hospital (KATH), Ghana. The Burns Registry at KATH BICU containing information on patients who were admitted for electrical burns was used. Data on the sex, age, occupation, cause of injury, Total Body Surface Area burned (TBSA) and outcome of admissions was obtained. GraphPad version 5 was used for the analysis. There were 13 (2.7%) electrical burns, suffered by 11 males (84.6%) and 2 females (15.4%) out of a total 487 BICU admissions over a 4-year period (July 1, 2009 – June 30, 2013); the mean age of the electrical burn victims was 37.8 years (range = 22–56); the TBSA ranged from 5.0% - 98.0%. Mortality risk factors identified were high voltage electrical burns, older age (P=0.0250) and TBSA>20% (P=0.048). Four cases (30.8%) were transferred to the Main Burns Ward (Ward D2C); 6 cases (46.1%) were discharged home; 3 patients (23.1%) died; all deaths were recorded in persons who had high voltage electrical burns. Electrical burns can be severe and can cause death. Even though the current study showed that a small population was affected by electrical burns, society has to be continually conscious of the detrimental effects of electrical energy and take the necessary precautions to minimize this type of accident.
Keywords: electrical burn injury, Burns Intensive Care Unit, mortality risk factors, total burns surface area, Ghana
Abstract
L’utilité de l’électricité dans la vie quotidienne offre plusieurs avantages qui ne peuvent être sous-estimés. L’électricité est nécessaire par les industries de fabrication et aussi dans les maisons pour l’éclairage, cuisson, lavage, etc. Toutefois, l’électricité peut provoquer de graves complications potentiellement mortelles. Cette étude examine l’évolution et les facteurs de risque de mortalité de brûlures électriques à l’Unité de soins intensifs aux brûlures de l’Hôpital Komfo Anokye, Ghana. Le registre des brûlures contenant des informations sur les patients qui ont été admis pour des brûlures électriques a été utilisé. Les données sur le sexe, l’âge, la profession, la cause de blessure, la surface corporelle total brûlée (SCT) et les résultats d’admissions ont été obtenu. GraphPad Prism 5 a été utilisé pour l’analyse. Il y avait 13 (2,7%) des brûlures électriques, subis par 11 hommes (84,6%) et 2 femmes (15,4%) sur un total de 487 admissions à l’Unité sur une période de 4 ans (du 1er juillet 2009 - 30 Juin, 2013) ; l’âge moyen des victimes de brûlures électriques était de 37,8 ans (extrêmes = 22-56); le SCT variait de 5,0% à 98,0%. Les facteurs de risque de mortalité identifiés pour les brûlures électriques à haute tension étaient: personnes plus âgés (p = 0,0250) et SCT >20% (p = 0,048). Quatre cas (30,8%) ont été transférés à la section principale pour le traitment des brûlures (Ward D2C); 6 cas (46,1%) ont obtenu leur congé; 3 patients (23,1%) sont décédés; tous les décès ont été enregistrés chez les personnes atteintes de brûlures électriques causées par la haute tension. Les brûlures électriques peuvent être graves et peuvent entraîner la mort. Même si l’étude a montré qu’une petite population a été affectée par des brûlures électriques, la société doit être constamment consciente des effets néfastes de l’énergie électrique et doit prendre les précautions nécessaires pour minimiser ce type d’accident.
Introduction
Electrical burns are burns that occur as a result of electricity passing through the body and causing extensive injuries. Extensive injury occurs sub-dermally whiles minor injuries are seen superficially. The extent of damage may involve the heart, brain and other internal organs of the body.1 Factors that determine the extent of electrical damage when a person is electrocuted are the current, voltage and resistance. Severe complications following electrical burns are possible and could eventually be fatal. Electrocution occurs when an individual comes into contact with any naked wire which is electrically active without any protective covering or apparatus, through playing with an electric wire that has current flowing through it, by inserting fingers into electrically live sockets, and sometimes from lightning.
Two types of voltage are known: high voltage and low voltage. Low voltage electrical burns occur when the electric current is below 500 volts and involves either the hands or oral cavity.2 Electrocution from this low voltage could be mild or superficial depending on the length of contact time between the body part involved and the electrical object. Since the quantum of current passing through a person is not enormous in the case of low voltage burns, the resulting tissue damage is not extensive. With high voltage electrocution, however, there is extensive damage to the individual due to the high level of energy passing through the person.3 Injury to internal organs is quite extensive due to the huge current passing through the individual.1
When an individual suffers electrocution, the first thing to do is turn off the main switch to the flow of the electric current before the individual is carried from the electrocution site.1 Since the extent of injury could be extensive, first aid in the form of assessing if the patient is conscious should be done before immediately taking them to a health facility for management. Management of electrocuted patients includes fluid replacement, administration of antibiotic and wound dressing4, while skin grafting or amputation may be necessary in some circumstances.
Patients and methods
Setting
KATH is the second largest hospital in Ghana. It is located in the middle belt of the country, in the city of Kumasi with a population of 2,035,064.5 KATH had an initial bed capacity of 1,000 but later expanded to 1,500, serving as a referral hospital for persons in the Ashanti, Brong Ahafo, Northern and Upper Regions. It is also a tertiary health institution affiliated to the School of Medical Sciences, Kwame Nkrumah University of Science and Technology. The Accident and Emergency (A&E) Centre located in the facility was established in 2009 to handle all emergencies. The A&E is a modern facility with a 160- bed capacity, housing units including the BICU of the Reconstructive Plastic Surgery and Burns Unit (RPSBU). The BICU of the RPSBU is a 6 unit room with sophisticated equipment to properly manage burns patients of all categories.
Protocol for Burns Management at KATH A&E Centre
Every burn patient is immediately attended to by the Emergency Physician team-on-duty after assessment by the triage nurses based on a protocol: “KATH accident and emergency centre protocol for burns management”, as noted in a study by Agbenorku P.6
Data collection
The Burns Registry at KATH BICU was used to obtain information on the patients. Data on the gender, age and occupation of victims, cause of burn injury, TBSA, treatment (including surgeries) performed, duration and outcome of admission were obtained.
Data Analysis
Information was displayed in graphs and analyzed with Graph pad version 5.
Ethical clearance
Ethical clearance for the study was obtained from KNUST School of Medical Sciences/KATH Committee on Human Research, Publication and Ethics, Kumasi-Ghana.
Limitations of the study
This study did not cover all the electrical burn injuries during the period under review given that some of those affected had only minor injuries and were treated outpatients, and thus their records were not captured in the BICU. Patients in the current study were all persons who were admitted to the BICU. The number of more severe cases of electrocution in which victims died at the scene, is also not known.
Results
Basic data/demographics
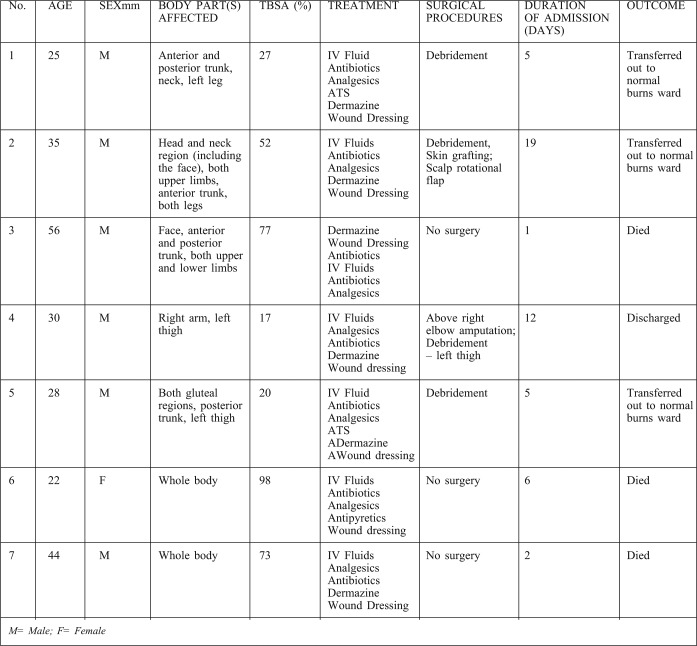
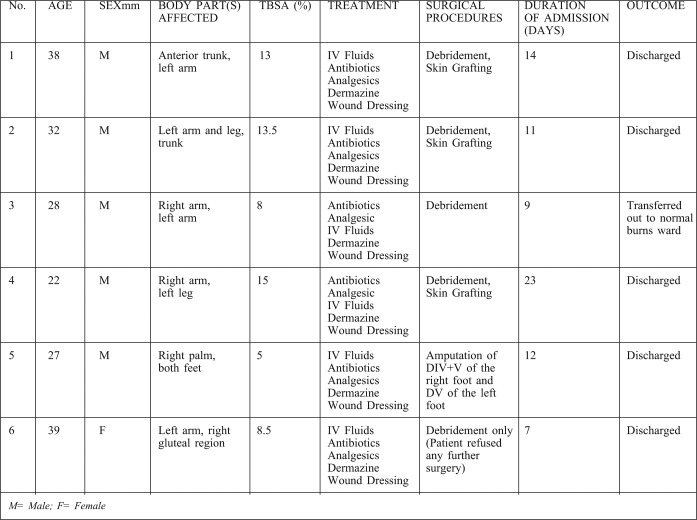
During the four (4) year period from July 1, 2009 to June 30, 2013, a total of 487 burn injury cases were recorded in the KATH BICU. Out of this total, there were 13 cases (2.7%) of electrical burns recorded, involving 11(84.6%) males and 2(15.4%) females. The mean age of the electrical burn victims was 37.8 years, with a range of 22-56 years. Occupations of the affected were driver’s mate (1), farmers (2), unemployed (1), artisans (5), caterer (1) and electrician (3). Seven (7= 53.8%) of these patients suffered high voltage injuries while 6 (46.2%) suffered low voltage burn injuries. The full data on the 13 patients, including their anatomical body parts affected, treatments received, duration and outcome of admission, etc., are listed in Tables I-II.
Table I. General data on the high voltage electrical burn injury patients in the study.
Table II. General data on the low voltage electrical burn injury patients in the study.
Extent of burns
These were severe burns, causing deep tissue damage to the affected area. The TBSA ranged from 5.0% - 98.0%. The parts of the body affected were variably the head and neck region (including the face), the anterior and posterior trunk, the whole body, and the limbs (Tables I-II).
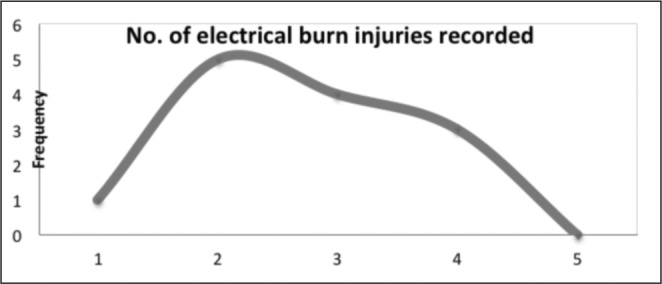
Trend of electrical burn injuries
The yearly trend over the 4 year period shows a drastic increase from one (1) in the last half (July – December) of 2009 to 5 cases in 2010, after which there was a gradual decrease to 4 and 3 in 2011 and 2012 respectively. No electrical burn injury was recorded within the first half (January – June) of 2013.
Fig. 1. Trend of electrical burn injuries.
Treatments received
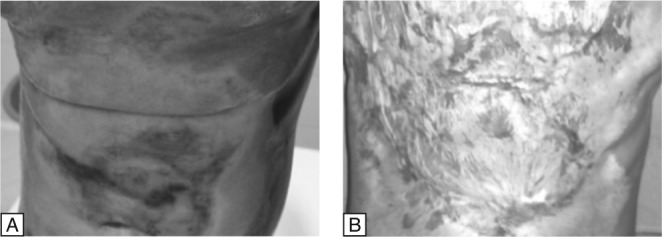
As in all burns, the same protocol was followed.5 Additionally, from Table I, debridement was carried out on 9(69.2%) patients and amputation on 1(7.7%); skin grafts on 4(30.8%); wound dressing on only 4(30.8%) - the 3 who died and one person who refused surgery; rotational scalp flap coverage on the scalp defect on 1(7.7%); and a combination of procedures on 5(38.5%). Some of these patients are shown in Figs. 2-5.
Fig. 2. Electrical burns injury to the arm: A - Following fasciotomy; B - Above elbow amputation at 3 weeks after total gangrene of the forearm; C - Healing at 5 weeks.
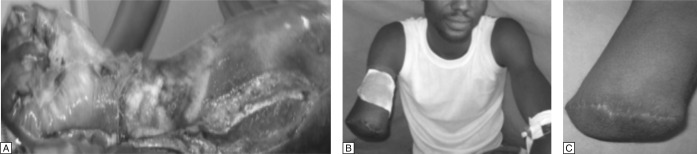
Fig. 5. Electrical burns in the right palm and both feet: A – Scar in the right palm showing entry point of current; B – resulting in the loss of digits 4 and 5 of the right foot; and C – loss of digit 5 of the left foot.

Fig. 3. Electrical burns injury to the leg: A - Total debridement complete after 2 sessions; B - Healing at 10 weeks having used only wound dressings; the patient refused any further surgery after the 2 debridements.
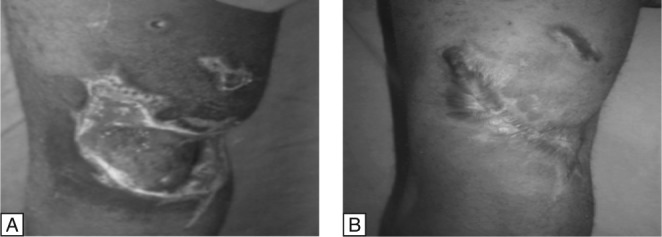
Fig. 4. Electrical burns on the anterior trunk region: A - Prior to wound debridement; B - Post debridement and healing on wound dressings only (10 weeks) with hypertrophic scarring; the patient refused skin grafting.
Length of stay
Duration of hospitalization/Length of stay (LOS) in the current study ranged from 1 day to 23 days with a mean LOS of 9.7 days (Table I). The mean length of stay of survivors in the hospital was 11.7 days.
Outcome of admission
Outcome of the electrical burns admissions were: transferred (trans-out) to the Main Burns Ward (Ward D2C) – 4(30.8%), discharged home, 6(46.1%) and death, 3(23.1%).
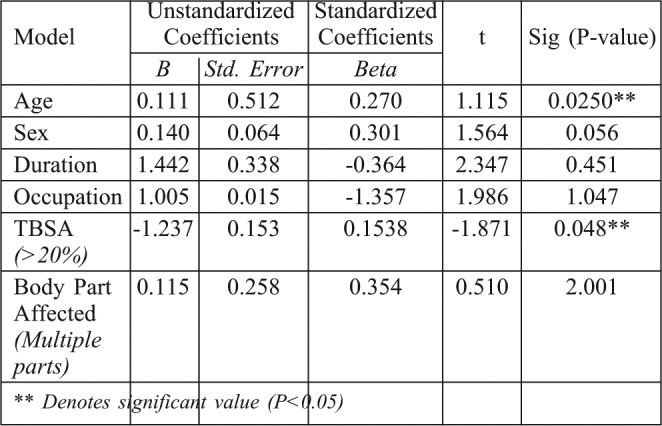
Mortality Risk Factors
Multiple regression analysis was used to determine socio- demographic features which are mortality predisposing factors in the current study. Using “deaths” (outcome of admission) as the dependent factor, all the demographic features of the participants were involved in the analysis with a probability value (P- value) of less than 0.05 considered to be statistically significant at 95% confidence interval (Table III).
Table III. Mortality risk factors of electrical burns in the study.
Discussion
Debilitating sequelae may follow electrical burn injuries. Victims and care takers may also be affected psychologically as a result of these complications.7,8 In as much as there is a need for electricity in our various homes, safety should be paramount. Electrical wiring of houses by inexperienced persons could result in electrical burn injuries if the work is not done correctly.9 In the current study, all electrical burns casualties were self-employed and so safety precautions were not as strictly enforced as they should have been. The extent of burns injuries cannot be estimated easily as extensive damage occurs sub-dermally and may require examination using Magnetic Resonance Imaging (MRI), hence extra care is needed when dealing with electricity. Deaths from electrical burn injuries cause particular pain to surviving members of the family, as most of them realize that such accidents could have been prevented. Also, in working environments where there is a possibility of an individual being exposed to electrical burn injury, the necessary safety precautions should be taken so that burns are prevented. Equally important is the administration of first aid to the victims in situations where the unexpected happens and an individual is electrocuted. Most of the people who suffered from low voltage burns from the study were exposed to low power live wires and were electrocuted by stepping on low lying electric cables or while wiring a house, or working on a roof top. No major internal damage was found in persons who suffered electrocution from low voltage. The high voltage injuries occurred through contact with high tension power cables, with injuries resulting from the following activities: mounting bill boards, fixing television antennae; and working on an electric pole near a high tension cable. Extensive damage to organs such as the heart, kidney, bone and the central nervous system was seen in persons with high voltage injuries. All deaths were recorded in persons who came into contact with high voltage current. All three electricians got electrocuted in their line of duty through one of the following means: working and accidentally touching a live wire, wiring a house, or working on an electric pole.
Morbidity resulting from electrical burn injury is possible in persons who may have to undergo surgery for amputation. Persons faced with this situation may become a burden on family members who would have to spend extra time and hours taking care of their needs resulting in under-productivity and an increased economic burden. Amputations become necessary when there is damage to nerves, tendons, skin and all blood vessels.10 A study has reported close relations between high serum creatinine level and risk of limb amputation and mortality in electrical burns patients.11
Electrical burns not only result in loss of precious human lives but also valuable properties, hence leading to economic hardship as the individual would have to start life all over again. Anlatici et al. and Lary et al. reported that damage caused by electrical burns as compared to other burn types, such as scalds, is extremely extensive.12,13 Management of burns in general and especially electrical burn injury patients requires much expertise. This is a reason for immediate transportation of the victim to the health facility since the outcome of electrical burns could result in death, as happened to the three (3) victims that lost their lives in the current study.It has been reported that annually about 1000 people die as a result of electrical burns injury in the United States.14,15 About 1500 severe burns cases are recorded yearly in Ghana with petrol-related fire as common aetiology.16 According to WHO, an estimated 43,000 persons die of burns annually in Africa with a rate of 6.1 per 100,000.17
Generally, children are more prone to suffer scalds than any other type of burn, as has been reported by some authors.18, 19-22 In the current study, only records obtained in the BICU were used and there was no record of children admitted to the unit for burns caused by electricity. It is probable that some children who might have suffered some form of electrocution and had minor burns were treated by the triage nurses according to the “Protocol on Patient Management at the Accident and Emergency Centre” 6 and transferred to Ward D2C as the BICU handles only severe burns cases. Equally, some of these burned children (and some adults as well) might have received treatments in nearby hospitals if the injuries did not require intensive care.
Length of stay (LOS) depends on the type of burns; for example, scalds burns may require shorter hospital stay compared to burns caused by electricity where extensive tissue damage may require surgical procedures such as debridement, local or free flap or grafting or amputation where necessary.23 However, in this study LOS ranged from 1 day to 23 days with a mean LOS = 9.7 days for all the patients, whilst for the survivors in the study the LOS = 11.7 days. These durations are by no means excessive, which might be due to the small study population. A mean length of stay (LOS) of survivors of 23.56 days was reported in a study of burns caused by petrol-related fires.16
Age and TBSA have been reported as risks factors for burns mortality.24,25 In their study to determine factors influencing burns mortality, Gokdemir et al. reported a TBSA >21% and Age >40 years as mortality risk factors.26 Similar outcomes were observed in the current study, which was solely on electrical burns, identifying mortality risk factors as high voltage burns, older age and TBSA >20%. This study supports the need for extra caution when working with high voltage electricity. The trend over the four year period under review shows a small population (n=13) affected by electrical burns, implying that electrical burns are not a major threat to society. However, the associated complications of such injuries can be fatal, as seen in the current study. For this reason, there is a need for public sensitization and education on prevention of electrical burns especially, and burns in general. The yearly figures suggests people are increasingly cautious when coming into contact with electricity, hence the trend.
Contractures and functional disability following burns injury in general have a tendency to create difficulties with activities of daily living.27 Such functional disability results in morbidity and consequently under-productivity, as well as affecting the quality of life of burns victims. Subsequently, it affects to a greater extent family members or caregivers who spend much time on these persons.28-30 Shyness, teasing from peers and others, and itching, as well as painful sensations from keloidal body parts was reported by participants who had some form of disability resulting from burns, thus causing them to develop a negative selfimage. 31 Often, in situations where there is extensive tissue damage as a result of electrical burns injury, decompression fasciotomy or amputation is required.31 Even though amputations due to severe electrical burns (and other forms of burns as well) can be compensated for by fitting a prosthesis, normal body function may not always be achieved. Electrical burn injury is thus a major form of trauma in our society, hence this study among the Ghanaian population, underlining the trend of such injuries as well as the morbidity and mortality in the selected sample population.
Electrical injuries can be avoided if correct preventive measures are put in place. Work involving contact with electricity should be planned very well to ensure that anyone required to handle the various tasks has the competence to do them. Protective clothing should also be worn and equipment should be inspected regularly by the person in charge/supervisor so that any faults can be repaired before the equipment is used for the intended job. The electrical current should be switched off before any work is started. In situations where a person has to work on a live wire, he must be accompanied by another who has the competence to offer help when the need arises, such as by turning off a main supply or providing first aid to an injured person.
Supervisors should also ensure that those working under them follow the right procedures and methods during their course of work to avoid the occurrence of accidents.32
Conclusion
Electricity could be seen as a “good servant but a bad master”. Even though the current study showed a small cohort (2.7%) affected as a result of electrical burns injury, debilitating sequelae coupled with some high risk consequences, including death, is a very strong indication of the need to be cautious when handling things which could have current flowing through them. Safety should be encouraged at all times and in all places from the home to the workplace, and any other sites where people may be at high risk of exposure to electricity and possible electrocution. These necessary precautions when adhered to would minimize this type of accident.
Acknowledgments
Conflict of interest. None.
Acknowledgement. The authors are grateful to the personnel of the RPSBU – doctors, nurses, anaesthetists, physiotherapists, etc. – who all helped to manage these patients; also thanking especially Miss Elizabeth Anthony who diligently collected the data that formed the basis of this work, and also Dr. Paul Saunderson for his useful comments on this work.
References
- 1.Health Care Advisor: Burn Treatment Self Help Guide, 2011. [Accessed November, 2013]. Available at: http://www.burnremedies.com/Electrical.html .
- 2.Nichter LS, Morgan RF, Bryant CA, et al. Electrical burns of the oral cavity. Compr Ther. 1985;11:65–71. [PubMed] [Google Scholar]
- 3.Electrical burns. Wikipedia. Oct, 2013. Available at: http://en.wikipedia.org/wiki/Electrical_burn .
- 4.How to Treat an Electrical Burn, 2010. [Accessed November, 2013]. Available at: http://www.livestrong.com/article/234861-how-to-treat-an-electrical-burn/
- 5.Ghana Statistical Service. Population and Housing Census, 2010. [Accessed January, 2014]. Available at: http://www.statsghana.gov.gh/pop_stats.html .
- 6.Agbenorku P. Modernized standards in burns management: A comparative study in Komfo Anokye Teaching Hospital, Kumasi, Ghana. Burns. 2013;39:990–6. doi: 10.1016/j.burns.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Herndon DN, editor. Total Burn Care. 1st ed. London: WB Saunders Company; 1996. Epidemiological, demographic, and outcome characteristics of burn injury. [Google Scholar]
- 8.Kimmo T, Jyrky VS, Sirpa AS. Health status after recovery from burn injury. Burns. 1998;24:293–8. doi: 10.1016/s0305-4179(98)00007-2. [DOI] [PubMed] [Google Scholar]
- 9.Turegun M, Sengezer M, Selmanpakoglu N, et al. The last 10 years in a burn centre in Ankara, Turkey: An analysis of 5264 cases. Burns. 1997;23:584–590. doi: 10.1016/s0305-4179(97)00081-8. [DOI] [PubMed] [Google Scholar]
- 10.Electrical burns. [Accessed March, 2014]. Available at: http://emedicine.medscape.com/article/1277496-overview?src=emailthis#aw2aab6b4)
- 11.Kopp J, Loos B, Spilker G, Horch RE. Correlation between serum creatinine kinase levels and extent of muscle damage in electrical burns. Burns. 2004;30:680–3. doi: 10.1016/j.burns.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Anlatici R, Ozerdem OR, Dalay C, et al. A retrospective analysis of 1083 Turkish patients with serious burns. Burns. 2002;28:231–7. doi: 10.1016/s0305-4179(01)00095-x. [DOI] [PubMed] [Google Scholar]
- 13.Lary AR, Alaghehbandan R, Nikui R. Epidemiological study of 3341 burns patients during three years in Tehran. Iran Burns. 2002;26:49–53. doi: 10.1016/s0305-4179(99)00102-3. [DOI] [PubMed] [Google Scholar]
- 14.Skoog T. Electrical injuries. J Trauma. 1970;10:816–30. doi: 10.1097/00005373-197010000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Cawley JC, Homce GT. Occupational electrical injuries in the United States, 1992-1998, and recommendations for safety research. J Safety Res. 2003;34:241–8. doi: 10.1016/s0022-4375(03)00028-8. [DOI] [PubMed] [Google Scholar]
- 16.Agbenorku P, Akpaloo J, Farhat BF, Hoyte-Williams PE, Yorke J, Agbenorku M, Yore M, Neumann M. Burn disasters in the middle belt of Ghana from 2007 to 2008 and their consequences. Burns. 2010;36:1309–15. doi: 10.1016/j.burns.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 17.Mock C, Peck M, Peden M, Krug E. A WHO Plan for Burn Prevention and Care. Geneva: World Health Organization; 2008. [Google Scholar]
- 18.Agbenorku P. Early childhood severe scalds in a developing country: A 3-year retrospective study. Burns and Trauma. 2013;1:122–7. doi: 10.4103/2321-3868.123073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balseven-Odabasi A, Tümer AR, Keten A, et al. Burn injuries among children aged up to seven years. Turk J Pediatr. 2009;51:328–35. [PubMed] [Google Scholar]
- 20.Akita S, Nakagawa H, Tanaka K, et al. Analysis of pediatric burns in Nagasaki University from 1983 to 2002. Burns. 2005;31:1041–4. doi: 10.1016/j.burns.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Akerlund E, Huss FRM, Sjoberg F. Burns in Sweden: An analysis of 24538 cases during the period 1987-2004. Burns. 2007;33:31–6. doi: 10.1016/j.burns.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Lin T-M, Wang K-H, Lai C-S, et al. Epidemiology of pediatric burns in southern Taiwan. Burns. 2005;31:182–7. doi: 10.1016/j.burns.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 23.Sahin I, Ozturk S, Alhan D, et al. Cost analysis of acute burn patients treated in a burn centre: The Gulhane experience. Ann Burns Fire Disasters. 2011;24:9–13. [PMC free article] [PubMed] [Google Scholar]
- 24.McGwin G Jr, George RL, Cross JM, et al. Improving the ability to predict mortality among burn patients. Burns. 2008;34:320–7. doi: 10.1016/j.burns.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Smith DL, Cairns BA, Ramadan F, et al. Effect of inhalation injury, burn size, and age on mortality: A study of 1447 consecutive burn patients. J Trauma. 1994;37:655–9. doi: 10.1097/00005373-199410000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Gokdemir MT, Aldemir M, Sogut O, et al. Clinical outcome of patients with severe burns presenting to the Emergency Department. J Current Surg. 2012;2:17–23. [Google Scholar]
- 27.Thakur JS, Chauhan CGS, Diwana VK, et al. Perineal burn contractures: An experience in tertiary hospital of a Himalayan State. Indian J Plast Surg. 2008;41:190–4. doi: 10.4103/0970-0358.39666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Esselman PC, Thomas BD, Magyar-Russell G, et al. Burn rehabilitation: State of the science. Am J Phys Med Rehabil. 2006;85:383–413. doi: 10.1097/01.phm.0000202095.51037.a3. [DOI] [PubMed] [Google Scholar]
- 29.Esselman PC, Ptacek JT, Kowalske K, et al. Community integration after burn injuries. J Burn Care Rehabil. 2001;22:221–7. doi: 10.1097/00004630-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Dyster-Aas J, Kildal M, Willebrand M. Return to work and healthrelated quality of life after burn injury. J Rehabil Med. 2007;39:49–55. doi: 10.2340/16501977-0005. [DOI] [PubMed] [Google Scholar]
- 31.Agbenorku P. Burns functional disabilities among burn survivors: A study in Komfo Anokye Teaching Hospital, Ghana. Int J Burns Trauma. 2013;3:78–86. [PMC free article] [PubMed] [Google Scholar]
- 32.Electricity at work: Safe working practices. HSG85, Third edition. Health and Safety Executive; 2013. pp. 1–33. [Google Scholar]