Summary
A 17-year-old male with burns to 8% of his total body surface area was treated for 10 days with Acticoat®, a nanocrystalline silver dressing. The burns, which were on his back and shoulder, healed without infection. However, a skin discoloration in the wound area and the adjacent uninjured skin appeared in the first days of treatment. The staining remained visible even after the treatment had ended and disappeared approximately three years later. Despite the outstanding antimicrobial properties, possible side effects of silver nanocrystalline dressings should be kept in mind.
Keywords: Acticoat, silver, burn, skin discoloration
Abstract
Un garçon de 17 ans avec des brûlures sur 8% de la surface corporelle totale a été traité avec Acticoat®, un pansement d’argent nanocristallin, pendant 10 jours. Les brûlures, qui étaient sur son dos et une épaule, ont guéri sans infections. Cependant, une décoloration de la peau dans la zone de la plaie et la peau indemne adjacente est apparue dans les premiers jours de traitement. La coloration est restée visible même après le fin du traitement et elle a disparu environ trois ans plus tard. Malgré ses propriétés antimicrobiennes importantes, il faut considérer les effets secondaires possibles de pansements d’argent nanocristallins.
Introduction
Preferable wound dressings are those that create a milieu in which the healing process can proceed undisturbed. The dressing should also relieve pain, be easy to handle and protect against wound infection. The material should be affordable and ideally have no side effects. The bactericidal effect of silver has been known since ancient times. Silver ions are used as disinfectants and as a therapeutic agent in wound therapy. They bind the DNA of bacteria and their spores, block enzymes and inhibit transport functions in the cell. Silver ions also affect the bacteria’s cell structures and damage their cell membrane.1,2
In the last 50 years, many different types of burn wound dressings containing silver have been developed, such as silver nitrate in the early 1960s, which was widely replaced by Silver Sulfadiazine Crème (SSD) in 1968.3,4 As a result of advances in micro-technology, such as plasma vapor deposition, Smith & Nephew were able to develop a new type of wound dressing containing silver in nanocrystalline form. This wound dressing was released under the name of Acticoat® (Smith and Nephew plc, London, UK). The advantage of this wound dressing is the consistent release of silver over a period of days. Since its development in the 1990’s, it has become an important part of treatment. Acticoat® is used mainly for the management of burn wounds, ulcers, donor and recipient graft sites. Many studies show the anti-bacterial efficacy of Acticoat®: Huang et al. show significantly shorter healing times when using Acticoat ® instead of SSD.5 Spear et al. also show a reduced length of hospital stay.6
A generally known side effect of silver dressings used in burn wound treatment is a local transient blackish staining of the burn wound and the surrounding unburned tissue. Permanent skin discoloration, however, is called argyria and thus the term “argyria-like symptom“ has been used to describe the generalized but transient skin discoloration after local application of silver coated dressing.7
In the following case report, we present a patient suffering from semi-permanent skin staining after the application of Acticoat® for burn wound treatment.
Case report
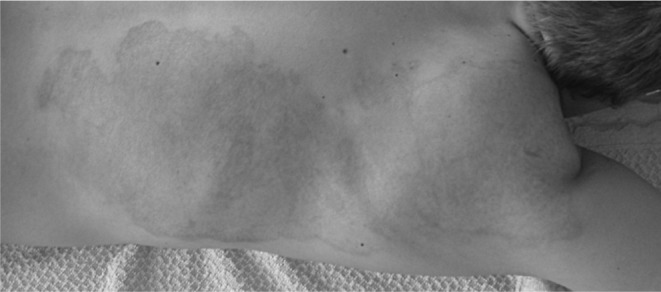
ln December 2006, while at work, hot oil drenched the shirt of a 17-year-old apprentice cook. He undressed immediately and cooled the wounds. The previously healthy young man sustained mixed dermal burns to 8% of his total body surface area (TBSA) on his right shoulder and back (Fig. 1). After initial resuscitation and analgesia at the local hospital, the victim was transferred to our burns unit two hours post injury. On admission, he was in a stable clinical condition, on a Ringer-Lactate drip and his wounds were covered with Burnshield®. Soon afterwards the patient was brought to the operating room for further wound evaluation and treatment. His body temperature was 36.3°C; he was conscious and pain free. The initial assessment of the wounds was that of mixed dermal burns.
Fig. 1. Day 1, burns unit: 8% TBSA mixed dermal burns on right shoulder and back.

Under anesthesia, the victim was washed completely, his wounds cleansed, and any loose or devitalized tissue was removed. The Acticoat® wound-dressing was moistened with sterile water and applied to the complete burn area, followed by wet and dry sterile gauze dressing, and secured in place with elastic netting. Blood samples were taken. Later assessment showed that the patient’s body temperature was well maintained and that he felt comfortable. The Acticoat® dressing was kept moist with distilled water twice a day and changed every three days under sedoanalgesia. Macroscopically there were no symptoms of any local infection and the wounds were showing good healing progress with the Acticoat® treatment. The patient was doing well, lab tests were within normal range; blood and urine silver levels were not checked. On day 10 post injury, the patient was discharged home with few residual wounds and noticeable reticular shaped dark striae within the wound and blackish staining of the adjacent uninjured skin (Figs. 2 and 3). Two and half weeks post injury, all wounds were completely healed and the staining of the adjacent uninjured skin disappeared. However, the persisting dark, retiform discoloration of the previously injured skin and remarkably dark margins gave us cause for concern. From two and a half months to one year post injury, the local findings remained the same: retiform, dark staining of the skin and dark margin (Fig. 4). When touching the stained surface, the isolated striae felt slightly raised. Nevertheless, the burn wound healed scar free. After one year, the patient refused to return for further visits to our outpatient clinic and resigned to the fact that his burn tissue had been permanently “tattooed“.
Fig. 2. Day 6 (second change of Acticoat): reticular shaped striae within the wound and blackish staining of the adjacent uninjured skin.

Fig. 3. Day 9: darker striae, also slightly raised, and increased blackish staining.

Fig. 4. One year post injury: the local findings remained the same (retiform, dark staining of the skin and dark margin).
On a chance meeting with the patient five years later, surprisingly, the “tattoo” had gone completely (Fig. 5). The then adult man could not remember exactly when the dark discoloration disappeared, suggesting it was “…maybe two years [prior].” however, he was quite happy with his subsequently “tattoo-less” back.
Fig. 5. Five years post injury: surprisingly, the “tattoo“ has disappeared.

Discussion
Humans have been in contact with silver and its compounds for a long time: via natural environment, industry or through the use of silver medication. Chronic intake of silver can result in permanent cutaneous discoloration – argyria. This condition is caused by silver-protein complexes deposited in the skin and reduced to inert silver salt by sunlight.8 As a result the skin takes on a blue or bluishgray hue.
The term “argyria-like symptom“ has been used to describe a transient, grayish discoloration of the face in a 17-year-old male with 30% burns who was treated locally with Acticoat® for seven days. After the local wound treatment with Acticoat® was aborted, the clinical symptoms returned to normal within days; however, the silver levels in serum remained elevated for months.9
In this paper we report a patient who suffered from “semi-permanent argyria”. After three years, the dark skin staining fortunately vanished completely.
In our patient, the dark skin staining resulted from burn wound treatment using Acticoat® dressing which contains silver. Following the product information, the dressing was hydrated twice daily with sterile water. In our opinion, silver particles must have penetrated into the dermis layer while the wound was healing and persisted there for approximately three years: similar to a tattoo.
According to Wikipedia10 “...a traumatic tattoo occurs when a substance such as asphalt is rubbed into a wound as the result of some kind of accident or trauma. They tend to be spread across several different layers of skin, and scarring or permanent discoloration is almost unavoidable.”
Walker et al.11 tested two silver-containing dressings, a Hydrofiber® dressing (Aquacel® Ag, ConvaTec Professional Services, Skillman, NJ, US) and a nanocristalline silver dressing (Acticoat®), for their potential to stain skin. When the dressings were hydrated with water, a significantly higher amount of silver was released from the nanocrystalline dressing compared to the hydrofiber dressing, which resulted in approximately 30 times more silver deposition. In contrast, when saline (0.9%) was used as the hydration medium, the release rates were low in both dressings and not significantly different.
Side effects of silver which have been documented in literature are transient skin discoloration6,12 and temporary elevated serum silver levels.12,13 In a comparative study of pediatric patients and a porcine model, Wang et al. postulate that the use of Acticoat® may lead to silver deposition in organs.13 In this model, he also showed the nature of skin discoloration in deep dermal burns. Histologically pigmented granulas were found throughout the burn scar tissue.
Conclusion
In the case study presented, we found neither an explanation for the prolonged existence of the skin staining nor any obvious reason why this “tattoo” should spontaneously disappear. Nevertheless, it should be noted that even a striking skin discoloration may disappear after years. To the best of our knowledge, there is no similar report in the literature.
Acknowledgments
Conflict of interest.None
Acknowledgements.The authors express their gratitude to Viktoria Horn for correction of the English manuscript.
References
- 1.Silver. Wikipedia. Oct, 2013.
- 2.Storm-Versloot MN, Vos CG, Ubbink DT, Topical silver for preventing wound infection. The Cochrane database of systematic reviews. 2010. CD006478. [DOI] [PubMed]
- 3.Walker M, Parsons D. The biological fate of silver ions following the use of silver-containing wound care products - a review. International wound journal. 2012 doi: 10.1111/j.1742-481X.2012.01115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khundkar R, Malic C, Burge T. Use of Acticoat dressings in burns: What is the evidence? Burns, journal of the International Society for Burn Injuries. 2010;36:751–8. doi: 10.1016/j.burns.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Huang Y, Li X, Liao Z, et al. A randomized comparative trial between Acticoat and SD-Ag in the treatment of residual burn wounds, including safety analysis. Burns, journal of the International Society for Burn Injuries. 2007;33:161–6. doi: 10.1016/j.burns.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 6.Spear M, editor. Skin Grafts - Indications, Applications and Current Research. Rijeka: 2011. Application of the nanocrystalline silver in treatment of burn wounds in children. pp. 237–64. [Google Scholar]
- 7.Trop M. The safety of nanocrystalline silver dressing on burns: A study of systemic silver absorption. Burns, journal of the International Society for Burn Injuries. 2009;35:306. doi: 10.1016/j.burns.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 8.White JM, Powell AM, Brady K, et al. Severe generalized argyria secondary to ingestion of colloidal silver protein. Clinical and experimental dermatology. 2003;28:254–6. doi: 10.1046/j.1365-2230.2003.01214.x. [DOI] [PubMed] [Google Scholar]
- 9.Trop M, Novak M, Rodl S, et al. Silver-coated dressing acticoat caused raised liver enzymes and argyria-like symptoms in burn patient. The Journal of trauma. 2006;60:648–52. doi: 10.1097/01.ta.0000208126.22089.b6. [DOI] [PubMed] [Google Scholar]
- 10.Tattoo. Wikipedia. Oct, 2013.
- 11.Walker M, Cochrane CA, Bowler PG, et al. Silver deposition and tissue staining associated with wound dressings containing silver. Ostomy/wound management. 2006;52:42–50. [PubMed] [Google Scholar]
- 12.Vlachou E, Chipp E, Shale E, et al. The safety of nanocrystalline silver dressings on burns: A study of systemic silver absorption. Burns: journal of the International Society for Burn Injuries. 2007;33:979–85. doi: 10.1016/j.burns.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Wang XQ, Kempf M, Mott J, et al. Silver absorption on burns after the application of Acticoat: data from pediatric patients and a porcine burn model. Journal of burn care & research: official publication of the American Burn Association. 2009;30:341–8. doi: 10.1097/BCR.0b013e318198a64c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


