Abstract
Tunnelled central venous catheters are commonly used for a variety of indications, including home parenteral nutrition, but are rarely associated with fracture and embolisation; the risk of embolisation is reported to be greater with catheters placed via the subclavian vein rather than the internal jugular route. We report the case of a 64-year-old woman with type 3 (chronic and irreversible) intestinal failure who presented with pain and swelling on infusion of parenteral nutrition through her internal jugular catheter. A chest x-ray showed fracture and embolisation of her catheter into the right ventricle. The embolised portion was retrieved and removed via the femoral route, without complication and the catheter replaced. We discuss causes of line embolisation, and highlight the possibility of embolisation occurring with an internal jugular catheter.
Background
Tunnelled central venous catheters are frequently used for the delivery of home parenteral nutrition (HPN) in type 3 (chronic and irreversible) intestinal failure. Catheter fracture with embolisation of the severed portion is a possible complication, which may lead to life-threatening haemodynamic or pulmonary complications. Catheter fractures at the level of the clavicle are often attributed to repeated compression and, in cases of subclavian catheter fracture, this is often attributed to the ‘pinch-off’ syndrome.
A recently published review of the causes of intravascular embolisation of venous catheters states that ‘pinch-off’ syndrome may be avoided by using the right internal jugular approach, as opposed to the subclavian approach.1 We report a case in which a tunnelled central venous catheter, placed using the right internal jugular approach, fractured at the level of the clavicle, with embolisation of the distal portion. Thus, we highlight that catheter fracture, at the level of the clavicle, is not necessarily obviated by adopting the internal jugular approach.
Case presentation
A 64-year-old woman with type 3 (chronic and irreversible) intestinal failure presented with pain on the right-hand side of her neck around the site of her tunnelled internal jugular venous catheter. The pain started on feed infusion via the catheter, and increased as feeding continued. However, she reported no resistance when flushing the catheter.
In 1976, she had been diagnosed with small and large bowel Crohn's disease, and underwent a colectomy with the formation of an end ileostomy in 1977. However, in 1983, she developed an entero-cutaneous fistula which culminated in her needing an extensive small bowel resection, which left her with only 60 cm of small bowel. Thus, she had short bowel syndrome, necessitating the use of long-term HPN.
For the last 30 years, she has been dependent on HPN, seven nights per week, via a tunnelled Broviac catheter. The catheter had been placed 5.5 months earlier, under x-ray guidance, via the right internal jugular vein, without complication. The previous catheter had been situated on her left, but was re-sited to the right following a tunnel infection. This right-sided catheter had been functioning normally until this presentation.
On examination, there was no visible swelling or dilated veins. The tunnelled portion of the catheter could be palpated up to the level of the clavicle. However, there was mild tenderness in the right supraclavicular fossa. Her body mass index was 19.1.
Investigations
A chest x-ray (CXR) was performed which confirmed fracture of her catheter at the level of the clavicle (figure 1). The fractured intravascular portion was visible within the cardiac shadow. ECGs performed at the time were normal. An echocardiogram confirmed the fractured catheter to be lying across the tricuspid valve between the right atrium and ventricle (figure 2).
Figure 1.

Chest x-ray showing the right internal jugular catheter fractured at the level of the clavicle. An arrow points to the embolised portion, which is visible within the cardiac shadow.
Figure 2.
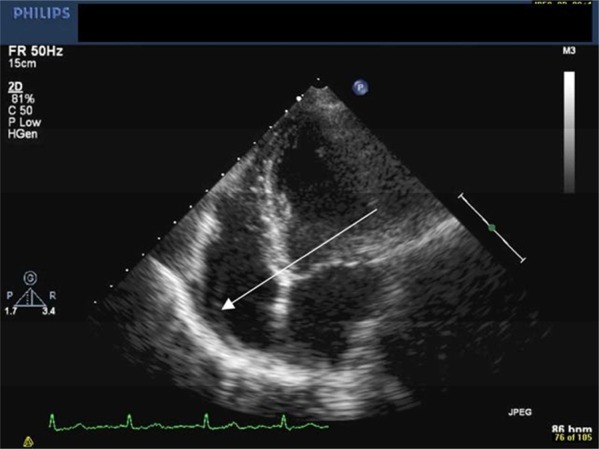
Echocardiogram with an arrow pointing to the fractured catheter within the right atrium.
Treatment
Following diagnosis, the patient was transferred to the care of an interventional cardiologist at a specialist cardiology centre. Percutaneous removal of the embolised catheter was performed, under local anaesthetic, via the right femoral vein. An Amplatz GooseNeck Snare was passed into the right atrium and the catheter was snared and retrieved through the venous access sheath, without complication.
Outcome and follow-up
In light of the patient's ongoing requirement for parenteral nutrition, a replacement tunnelled catheter was inserted using the same right internal jugular approach. This catheter has since (28 months) functioned without complication. No long-term effects have been encountered.
Discussion
In order to survive, patients with type 3 intestinal failure require long-term, safe and reliable intravenous access for delivery of nutrition and hydration. Intravenous access devices recommended for the delivery of HPN, in those patients expected to require therapy for over 3 months, include totally implanted ports and cuffed tunnelled central venous catheters.2 Tunnelled catheters, as used in this case, may be inserted into either the subclavian or internal jugular vein.
All venous access devices are associated with complications, such as infection, blockage, fracture and migration. Catheter fracture, with associated embolisation of the distal fragment, is relatively uncommon. A recent study, over a 22-year period, identified only 215 published cases of catheter-related embolisation, of which the majority (143) occurred with totally implanted ports rather than percutaneous, including tunnelled, catheters.1 In fact, only 21 of the cases involved tunnelled venous catheters, inserted into either the subclavian or internal jugular vein, as described in this case.
Catheter embolisation may present with, or cause, catheter malfunction, haemodynamic or pulmonary compromise or sepsis. However, patients suffering from embolisation of a percutaneous venous catheter are most commonly asymptomatic (47%).1 Most commonly, patients present with symptoms of catheter malfunction. In these instances, the catheter may appear blocked or the patient may experience pain or localised swelling on the start of an infusion, as happened in our case. Our patient displayed no signs of haemodynamic compromise, which is reported to occur in up to 19% of cases in which the embolised fragment is located in either the right atria or ventricle.
Recognised mechanisms for catheter embolisation include disconnection, which is most common with totally implanted devices, operator-induced damage on catheter explantation or exchange, catheter clearance techniques and ‘pinch-off’ syndrome. In this case, the catheter had functioned well, without any episodes of occlusion, for 5.5 months following insertion. Forceful injection techniques had not been used. In addition, as the catheter had initially functioned normally, it was unlikely to have been damaged on insertion. ‘Pinch-off’ syndrome is characterised by fracture of the catheter in the infraclavicular region, as occurred in this case. It was first described by Aitken et al, in 1984, and occurs on average 5.3 months after insertion.3 4 In these cases, repeated compression of the catheter between the first rib and clavicle causes damage and ultimately fracture. CXRs taken prior to fracture may show evidence of compression. This method of catheter fracture is reported only to occur with catheters inserted using the subclavian approach, due to the narrowness of the costo-clavicular space through which the catheter passes.3
Fracture at the level of the clavicle, of tunnelled venous catheters placed using the internal jugular approach, is rarely reported. The recently reported systematic review of the causes of intravascular catheter embolisation included 215 cases, of which only 72 were percutaneous venous catheters.1 This percutaneous catheter group was composed of 30 peripherally inserted percutaneous central (PICC) lines, 21 tunnelled venous catheters, 10 dialysis catheters, 5 pulmonary artery catheters and 6 unidentified catheters. Of the 72 percutaneous catheters, only 15 used the jugular vein, while 26 used the subclavian vein, 9 used a peripheral vein and 22 used an unknown route. As the review did not define which type of catheter used which route, the total number of tunnelled venous internal jugular catheters which embolised remains unknown, but can be no greater than 15.
The review identified that only 8 (11%) percutaneous catheters fractured at the level of the clavicle, but did not report how many of these were internal jugular tunnelled catheters.1 As fracture at this level, with subclavian catheters, may be attributed to the ‘pinch-off’ syndrome, and as these cases were attributed to this, it must be assumed that all were subclavian catheters. Hence, the authors, in the discussion, highlight that the ‘pinch-off’ syndrome is avoided by use of the internal jugular vein.1
Very few case reports describe right internal jugular catheter fracture, and fewer describe a fracture occurring at the level of the clavicle. Right internal jugular haemodialysis catheter fracture has been reported, and attributed to its repeated manipulation and acute angle in the neck region (site of fracture).5 In another case involving a haemodialysis patient, the tip of a previous right internal jugular catheter was found in the right atrium, following a CXR for an unrelated problem.6 This patient had previously had multiple venous catheters. The fragment length and fracture site were not reported. Fracture of a right internal jugular, totally implanted, chemotherapy access port has been reported at the level of the clavicle.7 This fracture was attributed to repeated compression of the catheter against the clavicle, because the patient was regularly wearing a backpack over his right shoulder. To date, no reported cases describe the fracture of a right internal jugular catheter at the level of the clavicle in a patient receiving HPN. In our case, the fracture occurred at the level of the clavicle, suggesting that the catheter may have been traumatically damaged at this level. Although no direct cause of catheter damage was identified, the patient's low body mass index may have contributed, by means of reduced cushioning between it and the clavicle.
In summary, this case highlights that catheter fracture, although rare, may not only occur with subclavian catheters, but can also occur with catheters placed via the internal jugular approaches. As such, in cases of catheter malfunction, clinicians must not exclude the possibility of catheter fracture, without investigation, simply because a right internal jugular approach was used.
Learning points.
Catheter embolisation is rare, and may have few clinical signs.
Embolisation may occur with internal jugular catheters.
Embolisation may occur without an obvious precipitating cause.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Surov A, Wienke A, Carter JM, et al. Intravascular embolization of venous catheter—causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr 2009;33:677–85. [DOI] [PubMed] [Google Scholar]
- 2.Pittiruti M, Hamilton H, Biffi R, et al. ESPEN Guidelines on Parenteral Nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr 2009;28:365–77. [DOI] [PubMed] [Google Scholar]
- 3.Aitken DR, Minton JP. The ‘pinch-off sign’: a warning of impending problems with permanent subclavian catheters. Am J Surg 1984;148:633–6. [DOI] [PubMed] [Google Scholar]
- 4.Mirza B, Vanek VW, Kupensky DT. Pinch-off syndrome: case report and collective review of the literature. Am Surg 2004;70:635–44. [PubMed] [Google Scholar]
- 5.Verhage AH, van Bommel EF. Catheter fracture—an underrecognized and serious condition in haemodialysis. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association. Eur Ren Assoc 2000;15:901–3. [DOI] [PubMed] [Google Scholar]
- 6.Reddy A, Stangl A, Radbill B. Retained catheter fragment from a fractured tunneled catheter—a rare and potentially lethal complication. Semin Dial 2010;23:536–9. [DOI] [PubMed] [Google Scholar]
- 7.Shimizu T, Mekata E, Murata S, et al. A case of catheter fracture of a totally implantable access port introduced through the right internal jugular vein. J Surg Oncol 2011;103:460–1. [DOI] [PubMed] [Google Scholar]


